Brachymetatarsia
Michelle L. Butterworth
Dennis E. Martin
Brachymetatarsia, a shortened metatarsal, is characterized by premature closure of the growth plate (1,2). The exact cause of this early epiphyseal closure of the metatarsal is unknown (3). Although brachymetatarsia is largely hereditary, it can be a congenitally, developmentally, surgically, or traumatically induced deformity (3). Brachymetatarsia most commonly affects the fourth metatarsal (4); however, it can affect any or multiple metatarsals. When the condition affects more than one metatarsal, it is known as brachymetapody. The condition is typically bilateral but may present unilaterally, especially in iatrogenic or traumatic situations.
Brachymetatarsia may be idiopathic or it can be associated with congenital anomalies, Down syndrome, Albright hereditary osteodystrophy, osteodystrophy, diastrophic dwarfism, multiple epiphyseal dysplasia, myositis ossificans, Turner syndrome, pseudohypoparathyroidism, pseudo-pseudohypoparathyroidism, and poliomyelitis (5,6,7,8 and 9). In poliomyelitis, the shortened metatarsal is primarily asymmetrical involving only the paralyzed limb (10). The correlation between these medical disorders and brachymetatarsia is unclear. Brachymetatarsia of the third and fourth metatarsals is frequently the result of pseudohypoparathyroidism or chromosomal abnormalities of the trisomy 21 pattern (11). Also, it is possible that a neurotrophic disorder or injury to the distal epiphysis could cause early union of the epiphyseal plate, causing cessation of the metatarsal growth (12).
When considering surgical intervention for the repair of brachymetatarsia, there are three main techniques that may be employed: lengthening/slide osteotomy, osteotomy with insertion of bone graft, and callus distraction. Although all of these techniques have been performed with some success, callus distraction remains the procedure of choice by the author for surgical repair of brachymetatarsia and is the focus of the remainder of the text.
Brachymetatarsia represents one of the best and most useful indications for callus distraction in the foot (13). Callus distraction is a technique in which an osteotomy is performed, a distraction device is applied, and the bone and surrounding structures are gradually lengthened. Callus distraction provides a significant improvement over the old bone grafting procedures (14,15). The gradual lengthening process provides sufficient time for the soft tissues to slowly adapt; therefore, the chances of vascular insult are greatly decreased since immediate, abrupt lengthening of the vasculature is avoided. Also, callus distraction is a more forgiving procedure, and the surgeon can control the amount of lengthening over time as opposed to being restricted to the degree of correction achieved at the time of surgery. It is because of these advantages and many other aspects unique to callus distraction that the author favors this surgical technique for brachymetatarsia repair.
EVALUATION/DIAGNOSIS/FUNCTIONAL ANATOMY
Brachymetatarsia is usually not noticed at birth but becomes clinically evident in children between 4 and 15 years old. It is more common in females with a female-to-male ratio of 25:1 (16,17). The signs and symptoms vary with the degree of deformity, age, and sex of the patient. In the younger patient, especially females, the major concern is typically cosmetic or psychological (11). These patients may become self-conscious about the appearance of their foot and their short-appearing toe, and they usually do not want to wear open-toed shoes or go barefoot.
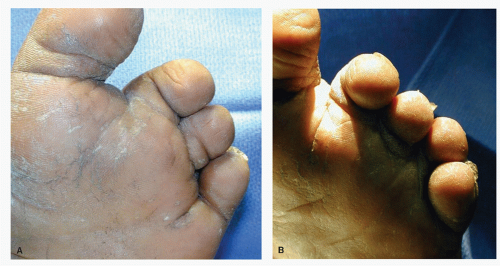
The older patient may experience more pain (11). The shortened metatarsal results in overloading of the adjacent, longer metatarsals. This excessive loading can then result in plantar calluses or metatarsalgia. These symptoms are more common in obese patients or in patients who stand or walk for long periods of time. In addition to plantar calluses under adjacent metatarsals, a floating toe on the shortened metatarsal may also develop. Since the short metatarsal bears no weight, its flexor plate fails to load, the digit does not purchase the ground, and an unstable, floating toe results. This floating toe syndrome is characteristic of brachymetatarsia (Fig. 72.1). The unstable digit remains shortened and contracted over the shortened metatarsal and may begin overlapping on to an adjacent toe. Over a period of time, this overlapping can cause soft tissue changes resulting in contracture of the extensor tendons, flexor tendons, and skin. Since failure of the extrinsic tendons to load on the short ray results in an increased loading on other toes, some degree of digital deformity of the adjacent toes may also result. The resulting digital deformities can cause pain and discomfort, especially when wearing shoes.
Since brachymetatarsia clinically reveals a short, contracted, floating toe dorsally, the toe is usually not seen plantarly (Fig. 72.2). A deep sulcus is usually found beneath the involved, shortened metatarsal, and adjacent toes tend to migrate into the space vacated by the floating toe.
Radiographic findings include a short, underdeveloped metatarsal (Fig. 72.3). Typically, there is deficient bone content in general with osteoporosis of the metatarsal head in particular (18). The toe is usually straight but in an extended position
and floats above the weight-bearing surface. Often, in addition to the metatarsal being short, the phalanges in the respective toe are also short, particularly the proximal phalanx.
and floats above the weight-bearing surface. Often, in addition to the metatarsal being short, the phalanges in the respective toe are also short, particularly the proximal phalanx.
CRITERIA/SELECTION OF PROCEDURE/CONTRAINDICATIONS
The treatment of brachymetatarsia may vary with the degree of metatarsal shortening, symptoms, age, and activity level of the patient. Conservative treatments consist of palliative care, padding and strapping, orthotics, and shoe gear modifications. Conservative treatment will not correct the cosmetic, psychological, or underlying anatomical and structural problems of the deformity. Surgical intervention can be pursued if structural correction is desired by the patient for the attempt at reduction or relief of pain. Although this deformity has many cosmetic and psychological components, the author does not advocate this procedure strictly for cosmetic purposes. This surgical technique has many possible complications including scarring and persistent digital deformity, which can often be cosmetically displeasing and require further surgical intervention.
There are basically three main techniques for surgical intervention for brachymetatarsia: lengthening/slide osteotomy, osteotomy with insertion of bone graft, and callus distraction. The decision of which procedure to employ is highly dependent upon the clinical and radiographic presentation. When a small amount of length is needed to obtain correction or there is a sagittal plane deformity within the metatarsal, a lengthening or slide osteotomy, such as a sagittal Z-osteotomy, can be employed. This osteotomy can provide length as well as correct for plantarflexion or dorsiflexion deformities within the metatarsal; however, it can be technically very difficult to perform. Also, this technique is often inadequate for treatment of brachymetatarsia because it can be very difficult to obtain the amount of length needed in the majority of these patients for successful results.
Historically, brachymetatarsia has also been successfully treated with an osteotomy of the metatarsal and insertion of a bone graft (1,2 and 3,17,19,20,21,22,23,24,25,26 and 27). This interpositional bone grafting technique is a single procedure in which all correction is obtained at the time of surgery. In cases in which significant correction is required, neurovascular compromise is a great concern when a one-stage lengthening procedure is performed. When the bone graft is placed, not only is the bone itself lengthened, all of the surrounding soft tissues have to be stretched and lengthened as well. Often, the tendons and skin must also be surgically lengthened to gain full correction with this technique. The greatest potential risk with this procedure is that lengthening the soft tissues in one acute setting can place undue tension on the vascular structures. This creates vasospasm and can ultimately result in loss of the digit. Furthermore, the soft tissues will limit the total amount of lengthening that may be achieved in a single stage procedure so that residual shortening and deformity may persist. Bone grafting also has other disadvantages such as a second surgical procedure for the donor site with possible subsequent complications and graft failure. The use of callus distraction has all but eliminated these problems. If there is a patient, however, that the surgeon feels will not comply with the rigorous postoperative course involved with the callus distraction technique or the patient themselves are uncomfortable with the idea of an external fixator being on their foot for several weeks, then bone grafting may be the treatment of choice for that patient.
The technique of callus distraction has been used since the early 1900s, but it has only been recently that the methodology has evolved and surgeons have taken advantage of this alternative surgical approach to bone grafting (28). Callus distraction has been described by many authors for the repair of brachymetatarsia (7,9,15,29,30,31,32,33,34,35,36,37,38,39 and 40). The author feels callus distraction offers many advantages over other techniques for surgical correction of brachymetatarsia. Technically, the procedure is easier than procurement and placement of bone graft or complex lengthening osteotomies. Also, correction is closely monitored and achieved over time. The surgeon slowly obtains correction through a gradual process; therefore, he or she can modify the amount of correction needed by lengthening more and possibly shortening slightly if overlengthened. This gradual lengthening process allows the soft tissues, including skin, tendons, vessels, and nerves, to slowly adapt to the change; therefore, there is less vascular embarrassment and nerve complications. Also, it is rare that the skin subsequently needs to be lengthened. Although callus distraction has many advantages over these other techniques, it is not without its limitations. The postoperative course is rigorous and the success of the procedure is highly dependent upon patient compliance. Due to the intense patient involvement postoperatively, this is not the
procedure of choice for a potentially noncompliant patient. Careful patient selection is of the utmost importance when choosing this procedure for the repair of brachymetatarsia.
procedure of choice for a potentially noncompliant patient. Careful patient selection is of the utmost importance when choosing this procedure for the repair of brachymetatarsia.
CALLUS DISTRACTION
PHYSIOLOGY AND HISTOLOGY
The use of callus distraction techniques in the lower extremity is constantly growing. There are various indications, including but not limited to, brachymetatarsia repair, Evans calcaneal osteotomy, medial column osteotomies, and tibial osteotomies. Although advances in surgical technique have been made through the years, the basic physiology and histology of callus distraction remains the same. Understanding the physiology behind callus distraction can be summarized by reviewing Ilizarov’s law of tension stress (41). The law states that living tissue, when it is subject to slow steady distraction, can become metabolically activated in both the biosynthetic and proliferative pathways. This theory has been tested and confirmed by several other surgeons (42,43,44,45,46 and 47).
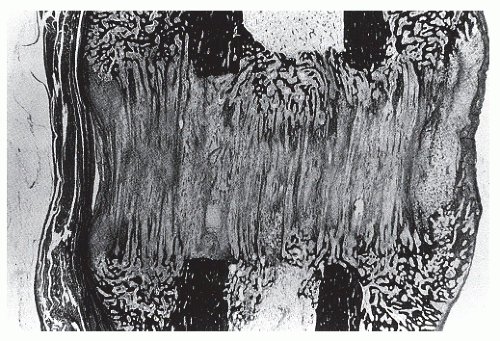
When distraction of the osteotomy is initiated, a gap is created and filled with hematoma and fibrous exudate. Within days, the gap is invaded by immature connective tissue. Vascular channels then appear, and at approximately 3 weeks, callus begins to form as fine cancellous bone is laid down in columns (Fig. 72.4). The callus is initially represented by longitudinally oriented collagen fibers, around which bone spicules eventually form. Some of these fibers span the entire distance between the bone ends (Fig. 72.5). At either end of the gap, fibrocartilage is seen between the bone end and the ossified or sclerotic edge of the distraction zone. The central growth zone appears in the center of the gap and is primarily composed of fibroblasts and chondrocytes (Fig. 72.6).
Regenerating bone continuously matures during and after lengthening. The radiolucent growth zone becomes ablated approximately 4 weeks after distraction has been stopped (Fig. 72.7). Cortex formation, called corticalization, takes place around 4 to 6 months after surgery and continues to remodel over a period of a year or more. Radiographically, the difference between regenerate bone and fracture callus is the organized longitudinal striations seen in callus distraction. Fracture callus is typically more bulbous in shape and lacks longitudinal striations.
 Figure 72.5 Radiograph 6 weeks postoperatively demonstrating the axial callus formation spanning the distance of the osteotomy site. |
There are also differences seen histologically between regenerate bone and normal bone, at least in the early stages of repair. Walsh et al (48) determined that the tensile properties of the lengthened bone improved and increased with time following the cessation of distraction. However, they remained significantly weaker (50%) compared with the controls, even at 12 weeks. Hamdy et al (49) added that even when 80% to 90% of the cortices regained their continuity, the strength of the lengthened bone was only 50% to 60% that of normal controls, hence the importance of initiating a slow gradual return to activity. Sferra et al (50) found that on torsional testing of the lengthened tibia, five out of six bones fractured within the diaphysis but outside the regenerate area. These findings suggested that the strength of the lengthened segment exceeded that of the original diaphysis, which was exposed to stress shielding by the external fixator.
SURGICAL TECHNIQUE FOR BRACHYMETATARSIA REPAIR WITH CALLUS DISTRACTION
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree