Chapter 4C Bone Marrow Stimulating Techniques
Autologous Matrix-Induced Chondrogenesis (AMIC)
Introduction
Chondral and osteochondral defects may affect any major joint, but they more often affect the large weight-bearing joints such as the knee and ankle joints. They may be of traumatic or hereditary origin (osteochondrosis dissecans). The original hyaline cartilage may as yet not be restored, so a permanent loss of the original cartilaginous surface is inevitable and responsible for premature arthritis and eventually destruction of the affected joint. However, a stable fibrous cartilage may develop from mesenchymal stem cells invading the defects from the underlying blood vessels, which will yield the patient pain free and slow down the process of joint destruction. Several methods in cartilage reconstruction are available such as ACT/ACI (autologous chondrocyte transplantation/implantation),1 matrix-induced autologous chondrocyte transplantation/implantation (MACT/MACI)2,3,4,5,6 and microfracturing. The membrane-associated chondrogenesis is well documented in vitro. A variety of collagen scaffolds is commercially available and may be applied. Fixation is possible either with fibrin glue (allogenic or partially autologous) or sutures.
An advantage of the autologous matrix-induced chondrogenesis (AMIC) procedure is that it is a one-step process for the patient, allowing the blood clot yielded after microfracturing to stay at the desired location and the chondrocytes to develop on a collagen scaffold in situ. Any collagen matrix will suffice.
Surgical Principles and Objective
Step 2: Miniarthrotomy
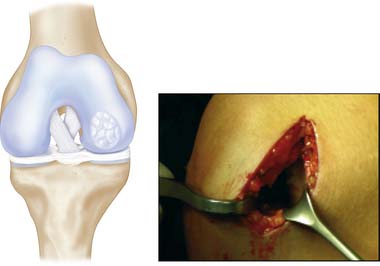
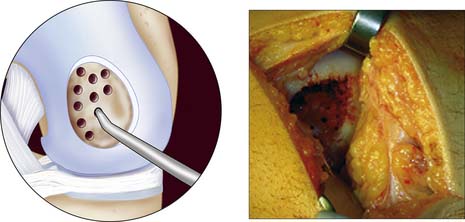
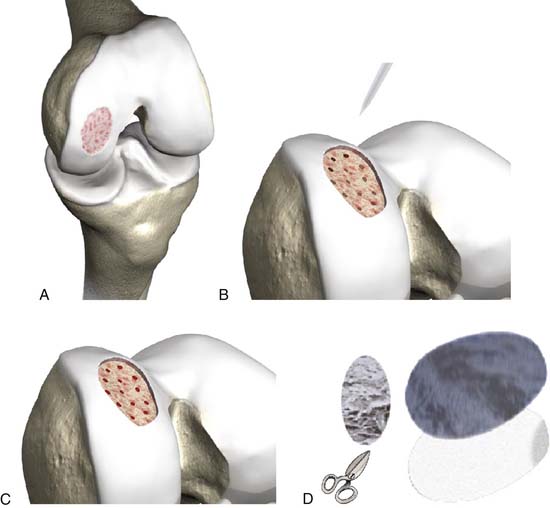
Debridement of lesion: degenerated and detached cartilage is completely removed, microfracturing with a sharp awl or pick, and, if necessary, a mallet to perforate the subchondral bone every 5 mm; a template is made that matches the size of the defect, not overlaying the defect (Figs. 4C-1, 4C-2, and 4C-3).
Step 4
In the meantime, a 10-ml blood sample is taken from the patient; derive the serum by centrifugation (using a hand centrifuge) or allow it to settle, discard 50% of the thrombin of the commercially available fibrin glue (double syringe system: one syringe is thrombin and the other is fibrinogen, for example Tissucol/Tisseel, Baxter Biosciences, Vienna, Austria), replace it with the autologous serum, and mix it so you get the partial autologous fibrin glue (PAF).
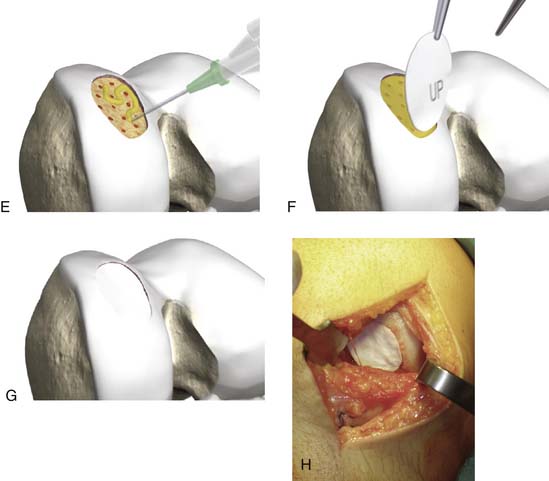
Step 5: Fixation of Matrix with PAF
The matrix is glued directly onto the prepared defect and is adjusted digitally. Finally the knee joint is held in an extended position for 5 minutes (Fig. 4C-4, A-H).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree