Bone Biopsy Techniques
Bone biopsy ranges from procurement of a bone specimen as part of an open incision and drainage or amputation procedure to an isolated percutaneous trephine technique. Needle biopsy has been shown to be a highly accurate method of diagnosing osteomyelitis, providing valid qualitative results with sensitivity and specificity rates above 70 % and 95 %, respectively [22, 23]. The trephine biopsy technique also has the advantage of being relatively noninvasive and inexpensive and can be performed at bedside or in the outpatient clinical setting. The larger bones of the rearfoot and ankle are more easily identifiable without the need for intraoperative imaging making bedside needle biopsy more practical. The smaller bones of the forefoot are less amenable to closed needle or trephine biopsy in part because it is difficult to obtain the biopsy without causing significant damage to the structure of the lesser (2–5) digital phalanges or even metatarsals. Ultimately, any bone in the foot could be accessed for a needle biopsy, but fluoroscopic guidance may be helpful to ensure correct bone identification (Fig. 4.1). There are risks associated with needle or trephine bone biopsy including pathologic fracture, joint damage, spreading or seeding bone infection, soft tissue damage, pain, bleeding, and nerve injury.
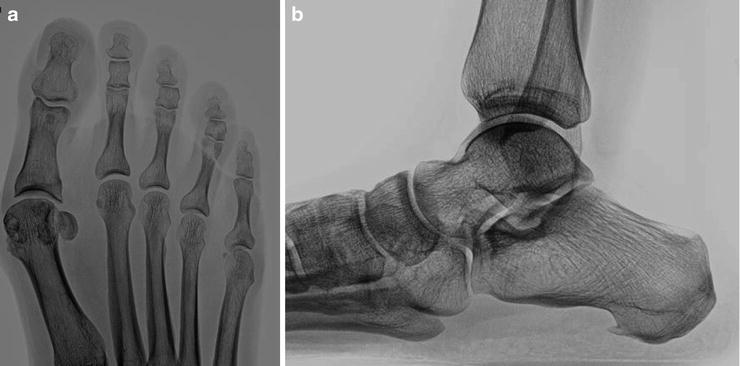
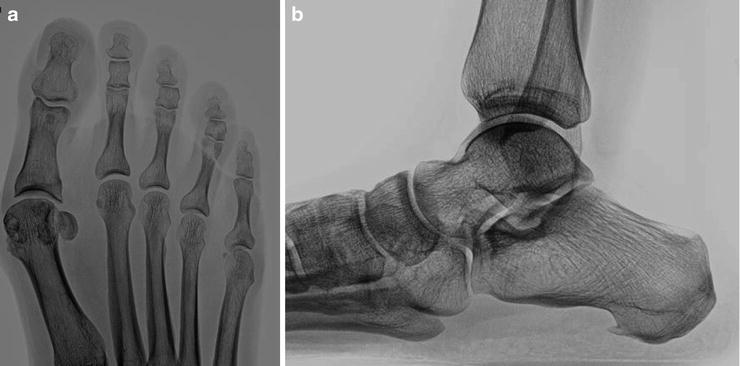
Fig. 4.1
Selection of the ideal bone biopsy technique. (a) The small bones of the forefoot are less amenable to percutaneous trephine biopsy and more amenable to open biopsy or wide resection. (b) The larger bones of the midfoot and rearfoot are less amenable to wide resection due to concerns about loss of structural integrity of the foot and more amenable to trephine techniques. Open biopsy is frequently the most practical approach for osteomyelitis associated with contiguous spread of infection from an adjacent wound since incision and drainage procedures are typically needed for wound-related infection. There is greater risk of cross contamination with open biopsy yet the location from where the specimen is extracted is more accurate with regard to the bone most likely to be infected
Open bone biopsy is typically performed in the operating room but clinic-based open biopsy is possible under certain circumstances such as digital infection and ulceration. Open biopsy may involve joint arthroplasty, cortical debridement of exposed bone after wound excision, or wide resection including partial foot amputation or partial calcanectomy. Biopsy is commonly performed at the time of the incision and drainage procedure and is often repeated for staged surgery. Repeat cultures are not necessary at revision surgery unless infection is not responding to current antibiotic therapy. The bone specimen is frequently taken from bone that would otherwise be discarded, as in the case of amputation or digital arthroplasty.
Trephine Bone Biopsy of the Small Bones of the Forefoot
While less practical for digits 2–5, trephine biopsy of the hallux and first metatarsal is common due to large bone structure with less likelihood of joint injury or pathologic fracture. An office or bedside protocol is demonstrated in Fig. 4.2. A medial midline approach is most practical to avoid the plantar weight bearing surface, the dorsal and plantar tendons, the nail or nail matrix, and neurovascular structures. Dorsal and plantar amputation flaps are also unaffected by this biopsy location.


Fig. 4.2
Trephine bone biopsy of the hallux. (a, b) Bone biopsy was performed for clinical appearance of first toe infection with correlating suspicious radiographic changes (arrow). The phalanges of the first toe are large enough for small trephine biopsy although there is risk of pathologic fracture or joint damage with this technique. Bedside or office-based biopsy is possible and requires minimal instrumentation. A small stab incision was made directly over the desired area of biopsy. (c) Care was taken to avoid neurovascular structures along the medial side of the toe and midline incision is helpful from this regard. Blunt dissection down to the bone level was performed with a mosquito hemostat. (d) The trephine or biopsy needle was positioned against the medial cortex of the proximal phalanx. The trephine was then carefully advanced through the cortex and into the medullary canal. A slight “wobble” technique disengages the biopsy specimen from the surrounding bone and minimizes chance for pathologic fracture. (e, f) The plunger was then used to extract the bone graft from the trephine. (g) Several small specimens can be obtained through one cortical puncture. Direct inspection of the biopsy specimen confirmed a relatively normal bone appearance without intraosseous pus or necrosis. (h) A small specimen was placed in the culture jar and the remainder was placed in formalin for histopathologic evaluation. (i) A simple suture can be placed which minimizes bleeding and risk of postprocedure contamination
Wound Excision and Open Corticotomy with Bone Biopsy
Wound infection with secondary contiguous spread of osteomyelitis to the prominent underlying bone is commonly treated with wound excision, decortication, bone biopsy, and remodeling of bone irregularity. A staged approach is common and flap surgery may be used to provide coverage of the exposed cancellous bone. This surgical protocol is detailed in Fig. 4.3.
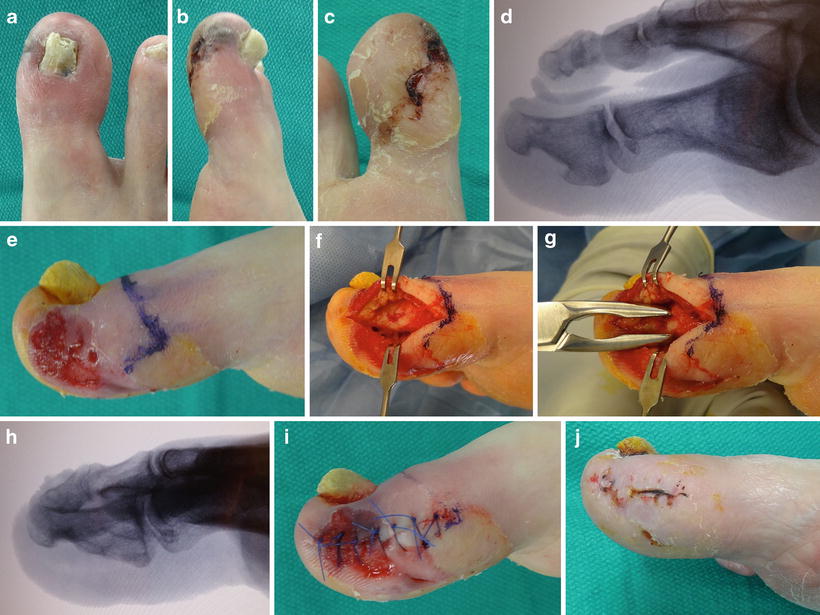
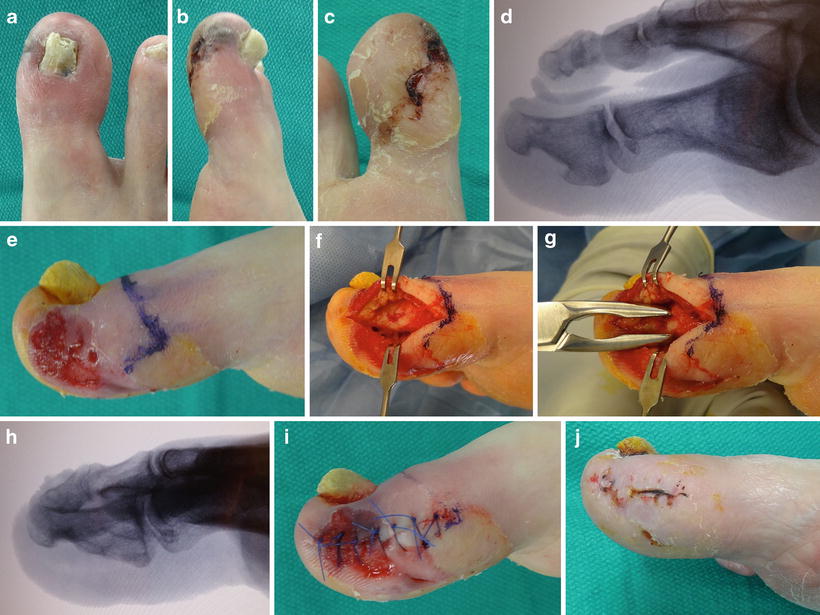
Fig. 4.3
Open resection biopsy of the hallux distal phalanx.(a–d) Local infection at the tip of the first toe combined with radiographic evidence of bone erosion within the distal phalanx raised concern for osteomyelitis. (e, f) Medial incision directly through the wound is not ideal for biopsy but allowed direct access for bone resection and biopsy. Note how the distal symes incision is drawn, which is the planned procedure if osteomyelitis is not resolved with biopsy and medical treatment. (g) A rongeur is used to take a nip of bone from the medial aspect of the distal phalanx. Prominent bone is oftentimes the nidus for recurrent ulceration which is also the bone most likely to develop osteomyelitis. (h) Bone biopsy that removes the source of the ulcer is ideal to allow wound healing and avoid wound recurrence. (i, j) Primary closure allows delayed revision surgery depending on clinical response and biopsy results
Joint Arthroplasty with Bone Biopsy
Inter-phalangeal and metatarsal phalangeal joint wounds complicated by osteomyelitis are typically associated with deformity including hammertoe contracture, bone spurs, and hallux valgus. Deformity is largely responsible for the non-healing wound and a biopsy is obtained through an open procedure. This approach, which is outlined in Fig. 4.4, allows for wound excision, drainage of joint infection, joint arthroplasty, deformity correction, bone biopsy, and possible wound closure. Digital procedures can be performed in the clinic and staged surgery is common with subsequent conversion to ray amputation depending on biopsy results and clinical response.
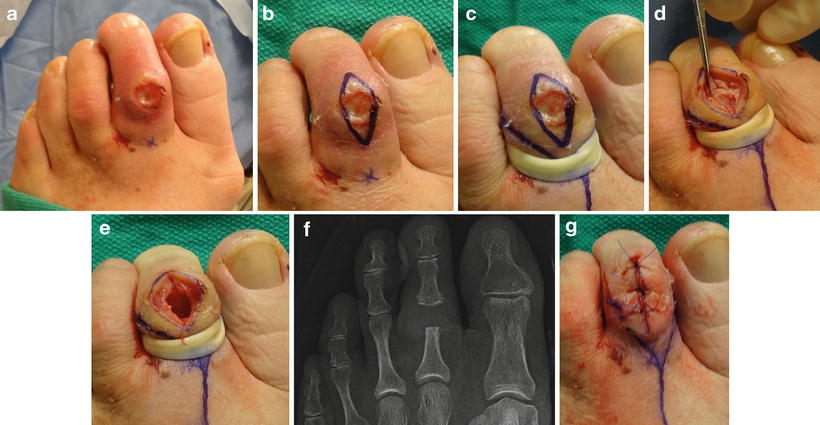
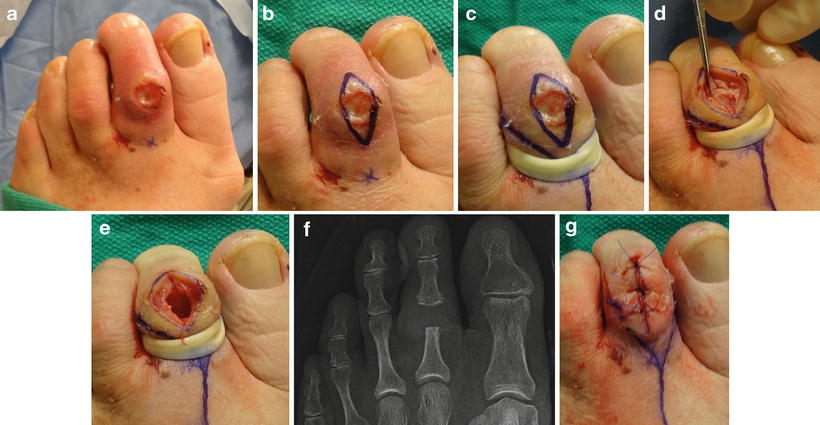
Fig. 4.4




Open biopsy of the second proximal interphalangeal joint. (a) Dorsal proximal interphalangeal joint (PIPJ) ulceration associated with hammertoe deformity commonly leads to osteomyelitis and joint infection. Trephine biopsy does not resolve the bone prominence and does not allow incision and drainage of the infection. (b) Open biopsy allows excision of the ulcer and access to the involved bone and joint. (c) An elastic drain tourniquet is used for office-based biopsy. Incisions are drawn here for planned toe amputation which may be required depending on clinical response and biopsy results. (d) Full depth excision of the wound and disarticulation of the PIPJ allows direct access for biopsy. (e, f) Resection of the head of the proximal phalanx allows biopsy as well as reduction of bone prominence and relaxation of contracture deformity. (g) Primary closure can be performed depending on the quality of the surrounding tissue and size of the wound defect
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








