Blount disease is a developmental disorder associated with childhood obesity. Based on whether the deformity is first noted before or after 4 years of age, early-onset and late-onset forms of Blount disease have been described. Besides physeal abnormalities of the proximal tibia, compensatory changes in the intra-articular morphology of the medial compartment of the affected knee are often noted on MRI scan. Both guided growth and acute and gradual correction via a proximal tibial osteotomy have roles in the surgical management of these patients. In order to optimize clinical outcome, frequent follow-up until skeletal maturity is recommended.
Key points
- •
Blount disease is a developmental disorder associated with childhood obesity.
- •
Based on whether the deformity is first noted before or after 4 years of age, 2 distinct forms (early onset and late onset) of Blount disease have been described.
- •
Radiographic changes primarily affect the posteromedial aspect of the proximal tibial physis, although a distal femoral varus deformity is seen in some adolescents with the late-onset form of the disease.
- •
Besides physeal abnormalities of the proximal tibia, compensatory changes in the intra-articular morphology of the medial compartment, including thickening of the medial meniscus, is often noted on MRI scan.
- •
Guided growth and acute and gradual correction via a proximal tibial osteotomy have a role in the surgical management of these patients.
- •
In order to optimize clinical outcome, frequent follow-up until skeletal maturity is recommended.
Introduction
Blount disease, also known as tibia vara, is a developmental disorder of unknown cause that primarily affects the posteromedial portion of the proximal tibial growth plate. Although there are many unresolved issues related to the pathogenesis and treatment of Blount disease, this clinical entity is often seen in overweight and obese children and adolescents. This article discusses some of the clinical findings and controversies related to this disorder that have emerged over the past decade.
Introduction
Blount disease, also known as tibia vara, is a developmental disorder of unknown cause that primarily affects the posteromedial portion of the proximal tibial growth plate. Although there are many unresolved issues related to the pathogenesis and treatment of Blount disease, this clinical entity is often seen in overweight and obese children and adolescents. This article discusses some of the clinical findings and controversies related to this disorder that have emerged over the past decade.
Causes and pathogenesis
Obesity
The association of increased body weight with Blount disease is well known and is most likely related to the effect of increased compressive forces on growth inhibition around the knee. In a study of 45 children and adolescents with Blount disease, we noted a strong association between body mass index (BMI) and varus malalignment of the affected extremity in patients with early-onset disease ( r = 0.74; P <.0001) and patients with BMI greater than or equal to 40 kg/m 2 , irrespective of age of disease onset ( r = 0.78; P <.0002). In a retrospective study of 69 children (aged 2–4 years) who presented with genu varum at a single institution, Scott and colleagues noted that the 20 children who were ultimately diagnosed with early-onset Blount disease had significantly higher BMIs (23.6 vs 18.3 kg/m 2 ; P <.001). In another study, from a cohort of 102 children presenting with Blount disease (average age, 5.9 years), Pirpiris and colleagues reported that those who were scheduled for surgical correction at initial presentation had greater BMIs and more severe deformities than those children who treated with observation. They conjectured that weight reduction in patients with Blount disease may decrease the number of children needing surgical intervention for their lower limb deformities.
Bowen and colleagues observed that obesity-related pediatric disorders such as Blount disease, slipped capital femoral epiphyses, and type 2 diabetes may represent distinct phenotypes, because each of the 151 such adolescents presenting at their center had only 1 of these 3 diagnoses. The BMIs were highest (mean BMI, 40.8 kg/m 2 ) among the Blount subgroup.
Metabolic Abnormalities
There are recent reports of a possible association of certain metabolic abnormalities with Blount disease. In a retrospective review of 890 patients seen at a pediatric obesity clinic, patients with vitamin D deficiency (25-vitamin D level <16 ng/mL) were 7.33 times more likely to be diagnosed with Blount disease than those with higher levels of vitamin D ( P = .002). In a study from Nigeria, children with early-onset Blount disease had significantly lower serum levels of zinc and higher levels of alkaline phosphatase compared with age-matched and sex-matched controls.
Deformity analysis
It is sometimes difficult to differentiate between physiologic genu varum and mild cases of early-onset Blount disease. Although assessing the metaphyseal-diaphyseal angle (MDA) of the tibia in young children is useful in differentiating physiologic genu varum from early-onset Blount disease, there is some variability in the landmarks used for measuring this angle. Auerbach and colleagues measured the MDA on 132 knee radiographs of 66 children with bow legs using 2 separate distal lines for the diaphysis (lateral border and center of the tibial shaft). Among children with MDA greater than 11°, both measurement methods were acceptable and excellent correlation ( r = 0.90; P = .0087) was reported between the two assessment techniques. In a similar study comparing the two measurement techniques, but with the use of digital radiographs, Lavelle and colleagues reported excellent reliability for assessing the MDA among 27 pediatric orthopedic surgeons.
There are distinct radiologic findings in both early-onset and late-onset Blount disease. Although there is proximal tibial varus deformity noted in both types, there are certain differences between the two forms of this disorder. In a radiographic review of full-length anteroposterior lower limb radiographs of 38 patients with Blount disease (21 early onset, 17 late onset), Myers and colleagues reported that adolescents had greater distal femoral varus than both the infantile group and normal reference values, whereas neither group of patients with Blount disease had any statistically significant distal tibial malorientation in the coronal plane. Based on a radiographic analysis of 73 patients (109 extremities) with Blount disease (56 early onset, 53 late onset), Gordon and colleagues also reported similar findings. Furthermore, among the adolescent group, the distal femur contributed approximately 30% (6°–20°) of the varus deformity.
We performed a multiplanar deformity analysis using clinical examination including rotational profile and biplanar radiographs of the lower extremity in 40 patients with 60 affected extremities (26 early onset, 34 late onset). We observed a greater magnitude of proximal tibial varus, procurvatum, and internal rotation in the early-onset group. Similar to previous reports, in the late-onset group, about one-third of the varus deformity originated from the distal femur. Furthermore, neither age group showed any clinically significant frontal plane deformity of the proximal femur and distal tibia, or any sagittal plane deformity of the distal femur and distal tibia. Using clinical examination and computed tomography (CT) torsional profile of the lower extremity of 14 Zulu children with Blount disease (9 early onset, 5 late onset), Aird and colleagues found that, besides internal tibial torsion, femoral anteversion (26° greater than reference values) contributed to the intoeing in these children.
The presence of procurvatum deformity of the proximal tibia in children with Blount disease is well known. We recently studied the correlation between clinical and radiographic measurements of the sagittal alignment in 43 patients (47 affected limbs) with Blount disease. We found that the visual inspection of the extremity can underestimate the procurvatum noted on full-length tibial radiographs. Furthermore, reestablishing the normal sagittal profile of the proximal tibia with an osteotomy did not lead to clinical hyperextension of the extremity.
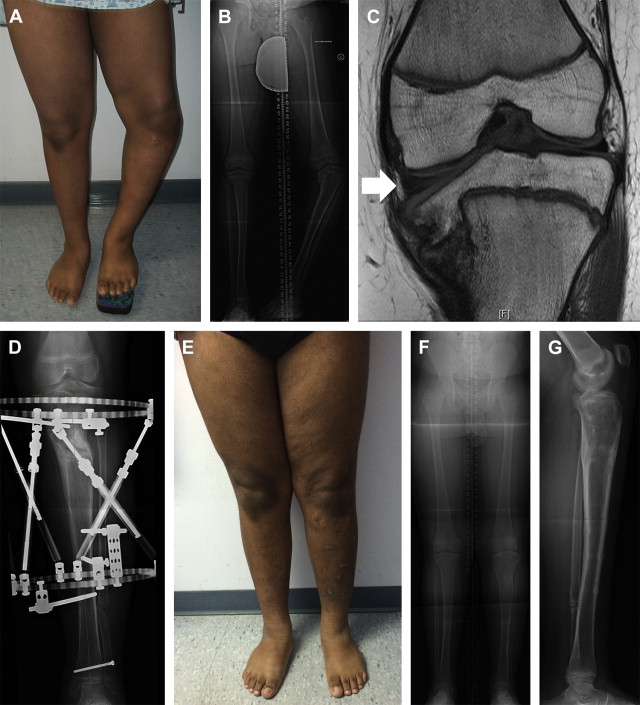
There is some controversy regarding the intra-articular morphology of the knee joint in children with Blount disease. Using MRI, we compared the coronal and sagittal morphometric measurements between 26 children (33 knees) with Blount disease and 20 children (20 knees) who served as controls. Children with Blount disease had significantly greater thickness of the medial proximal tibial chondroepiphysis, increased height and width of the medial meniscus, and greater frequency of abnormal signals in the posterior horn of the medial meniscus ( Fig. 1 ). Because of the compensatory changes in the medial compartment, the overall coronal and sagittal inclination of the knee joint in the children with Blount disease was similar to that of the control group. The BMI of the patients with Blount disease correlated with the height of the medial meniscus. Despite these findings, it is plausible that the thickened unossified proximal tibial chondroepiphysis may not have the same capacity to withstand compressive forces as that of the proximal tibial epiphysis in a similar-aged child without Blount disease. Based on MRI of 11 children (18 knees) with early-onset Blount disease, Ho-Fung and colleagues reported similar morphologic changes in the medial menisci. Furthermore, they reported increased prevalence of abnormal signal intensity in the medial femoral condyle and tibial epiphysis compared with age-matched controls.
Perioperative considerations
Childhood obesity is associated with altered physiology affecting various organ systems. For instance, obstructive sleep apnea was identified in morbidly obese juveniles and adolescents with Blount disease. Gordon and colleagues reported that 11 of 18 (61%) children 9 years of age or older with Blount disease were diagnosed with sleep apnea based on polysomnography and required preoperative noninvasive positive pressure ventilation. These investigators recommended that such individuals should be screened for snoring and, if it is present, should be further evaluated for sleep apnea before surgical correction of their lower extremities.
It is well known that obese children are prone to precocious puberty. This predisposition can also affect skeletal growth and have surgical implications. Based on a case-control study, we recently reported advanced bone age in children with Blount disease. Compared with their chronologic age, the bone age (based on the Greulich and Pyle method) of 33 children with Blount disease was advanced by an average of 16 months (26 months in the early-onset group and 10 months in late-onset group). The discrepancy between the chronologic and skeletal age decreased as the chronologic age increased. Given the potential for limited growth remaining in some of these patients, preoperative assessment of skeletal age should be considered because it can affect the timing and magnitude of (over)correction for surgical options such as physeal bar excision, guided growth, and realignment osteotomy.
Surgical treatment options
Hemiepiphysiodesis and Guided Growth
There has been a resurgence of interest in using the principles of physeal growth manipulation for addressing lower limb angular deformities in Blount disease. Such guided growth can be accomplished with permanent ablation of a portion of the growth plate, such as by using drills and curettes for a lateral hemiepiphysiodesis effect or placing extraperiosteal implants like staples, transphyseal screws, or nonlocking plates across the faster-growing lateral portion of the affected physis with the potential for growth resumption following implant removal. When reporting their results, investigators often report on patients undergoing the temporary and permanent growth modulation techniques together, and thus make subgroup analysis of the outcome of each technique challenging. Wiemann and colleagues recently compared the efficacy of staples (39 limbs) versus 8-plate implants (24 limbs) for angular deformities around the pediatric knee, including patients with Blount disease. Although the overall rates of correction and complication were similar between the two implant groups, patients with abnormal physes (such as those with Blount disease) had a higher complication rate than those with a normal physes (27.8% vs 6.7%; P = .04), irrespective of the type of implant.
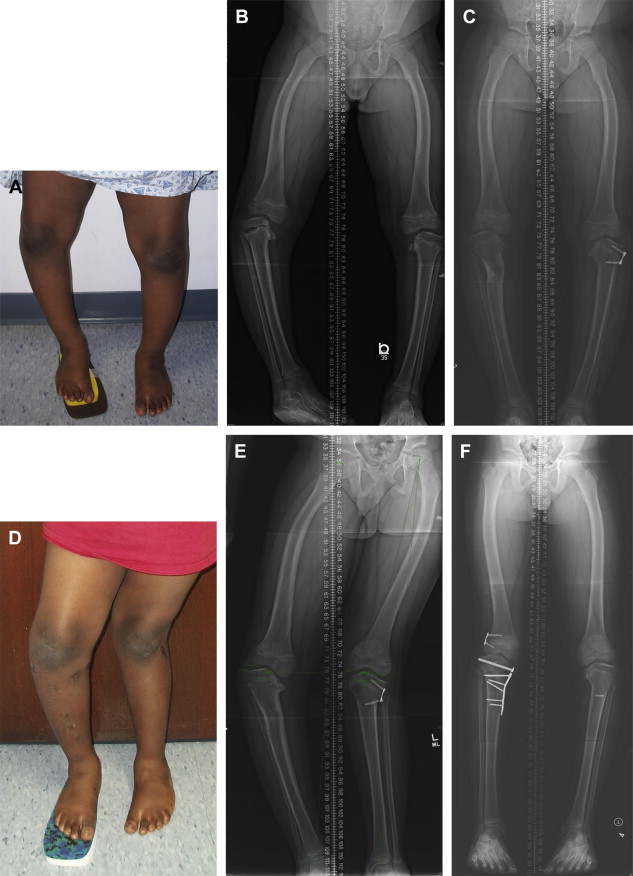
In the past, hemiepiphysiodesis, including the use of staples, has been advocated for adolescents close to skeletal maturity. However, with the introduction of the tension band plates for guided growth, there is a potential to use these implants for younger children. In a retrospective review of 12 children (18 limbs) with early-onset Blount disease who were treated with lateral tension band plating, an 89% success rate was noted. Failures and delayed correction was related to wound infection, requiring premature implant removal and screw breakage. Some children showed recurrence of deformity following elective plate removal ( Fig. 2 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






