Biceps Instability and Tendinitis
Keith D. Nord
Paul C. Brady
Bradford Wall
Biceps pathology has been recognized for centuries, but the function of the biceps has been controversial and its treatment varied. Neer described the long head of the biceps (LHB) tendon as a depressor of the humeral head. Even this early observation is still questioned. Pathology of the biceps tendon is frequently associated with other conditions such as impingement, Superior Labrum Anterior and Posterior (SLAP) tears, and supraspinatus or infraspinatus tears. The anatomy of the biceps has been studied extensively, yet only recently have we begun to understand the significance of the medial sling. Monteggia recognized instability of the biceps tendon, yet identification of this condition has been difficult and often unrecognized or incidentally noted. Treatment of this condition has been rapidly improving, as we begin to understand the progression of and the restraints to instability.
Arthroscopy has shed more light on the anatomy and biomechanics of the biceps and pulley system. In this overview of the LHB tendon, we will review the well-accepted anatomy and more controversial topics such as its function, pathophysiology, and treatment of instability, tendinitis, and tears.
BASIC SCIENCE
Anatomy
The anatomy of the LHB is well described, yet our understanding of its function is still progressing. The LHB originates at and around the supraglenoid tubercle. The LHB is intra-articular, yet extrasynovial, because it is lined by a synovial sheath. The proximal and middle portions receive blood supply from branches of the anterior humeral circumflex artery by the vincula, which move with the tendon in the groove. The distal third of the tendon receives nourishment from branches of the deep brachial artery. Despite the vincula, the blood supply in the portion of the tendon within the groove is still markedly reduced.
The LHB has been observed to originate primarily from the posterosuperior labrum 48% of the time by Habermayer et al. (1) and 70% by Pal et al. (2) Origin from the supraglenoid tubercle was reported to occur 20% and 25%, respectively, and Habermayer et al. noted that in 28% of the specimens the biceps originated from both the labrum and the tubercle.
The tendinous portion of the LHB measures approximately 9 cm in length, and the musculotendinous junction is at the level of the deltoid and pectoralis major insertions. Its shape is relatively flat at its origin, becoming more tubular as it proceeds distally and into the intertubercular groove. The LHB tendon is weakest at its midpoint and this is the site of most ruptures.
The LHB courses from the posterosuperior glenoid obliquely over the top of the humeral head. This oblique course is at a 30° angle, which decreases its effectiveness in comparative anatomy and increases the pressure on the medial side of the bicipital (intertubercular) groove. This groove is formed by the confluence of the lesser tuberosity (anteriorly) and the greater tuberosity (posterosuperiorly). The depth of the groove is typically 4 mm. Ueberham and Le Floch-Prigent (3) described a ridge on the upper portion of the lesser tuberosity (termed a supra-tubercular ridge) in 45% of anatomic specimens, which was postulated to “push” the biceps anteriorly and could be a cause of primary biceps lesions. Whereas some authors have suggested that a shallow inclination of the groove predisposes to dislocation (1) others have found no such association (3).
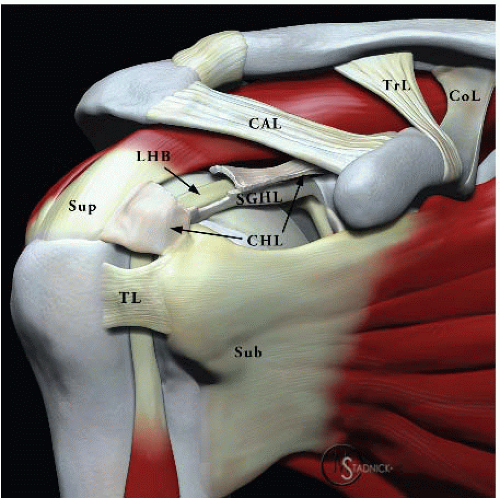
The most critical anatomic consideration regarding the LHB is its stabilizing structures. Specifically, a thorough understanding of the rotator interval (RI) and medial pulley system is essential. The RI is the triangular interval bordered superiorly by the anterior margin of the supraspinatus, inferiorly by the superior margin of the subscapularis, and medially by the anterior aspect of the glenoid. Within this triangular space exists the anterior glenohumeral capsule as well as the coracohumeral ligament (CHL) and the superior glenohumeral ligament (SGHL). The SGHL and the medial head of the CHL join to form a medial sling, or pulley system, for the LHB, and this is the major restraint to medial subluxation/dislocation of the LHB (4) (Fig. 15.1).
The CHL originates from the base of the coracoid process and divides into two bands—a superior band, which inserts into the anterior supraspinatus to form the
lateral or superior pulley, and an inferior band whose medial head inserts into the superior subscapularis and then onto the superior aspect of the lesser tuberosity. The SGHL also contributes to this medial sling as it courses from the anterior labrum (just anterior to the biceps origin) and inserts onto the superior aspect of the lesser tuberosity (Fig. 15.2). The fibers of the medial head of the CHL are much more robust and structurally important to the medial sling than the fibers of the SGHL. This medial sling or reflection pulley, is critical in preventing the LHB from displacing medially onto the lesser tuberosity. In this way, the sling protects the proximal insertion of the subscapularis from the stresses that would result from a medially displaced LHB.
lateral or superior pulley, and an inferior band whose medial head inserts into the superior subscapularis and then onto the superior aspect of the lesser tuberosity. The SGHL also contributes to this medial sling as it courses from the anterior labrum (just anterior to the biceps origin) and inserts onto the superior aspect of the lesser tuberosity (Fig. 15.2). The fibers of the medial head of the CHL are much more robust and structurally important to the medial sling than the fibers of the SGHL. This medial sling or reflection pulley, is critical in preventing the LHB from displacing medially onto the lesser tuberosity. In this way, the sling protects the proximal insertion of the subscapularis from the stresses that would result from a medially displaced LHB.
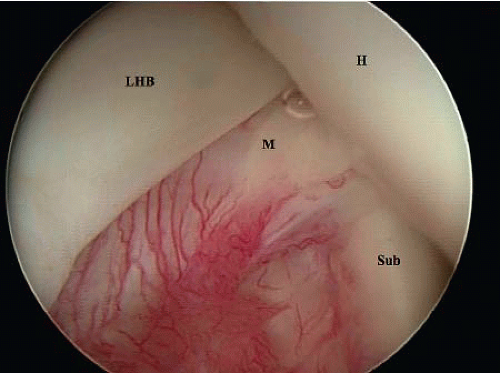
The medial sling and its relationship to the biceps tendon have been described as “the comma sign” by Lo and Burkhart (5). This comma sign is an arthroscopic description of the medial sling based on its appearance. The comma sign consists of the medial head of the CHL and SGHL (medial sling of the biceps) intersecting with the superior border of the subscapularis. Although the comma sign is visible in the absence of pathology, it is much more prominent, recognizable, and useful in the presence of a torn and retracted subscapularis tendon. When the subscapularis is torn from its insertion on the lesser tuberosity, the medial sling of the biceps is also pulled off and its association maintained with the subscapularis. Identification of this comma structure is critical when searching for the subscapularis tendon because it is always located at the superolateral border of the subscapularis tendon (Fig. 15.3).
Historically, it was felt that the transverse humeral ligament was the vital structure in regard to retaining the biceps within the bicipital groove (BG). However, this view is no longer well accepted. Ruotolo et al. (6) described the arthroscopic release of the sheath of the biceps tendon and dividing the transverse humeral ligament. Yet postoperative dislocation or subluxation of the biceps tendon did not occur. Ruotolo et al. emphasized that the CHL must be preserved with this technique to prevent biceps instability.
Biomechanics
The critical role of the biceps brachii at the elbow joint and its function has been well documented. It is the LHB’s role at the shoulder that causes arguments. Many authors have suggested that the LHB has a role in humeral head depression—particularly with shoulder external rotation. Andrews et al. (7) observed the biceps arthroscopically while electrically stimulating the biceps muscle and saw
the labrum lift superiorly and compression of the glenohumeral joint. However, other studies showed no humeral head motion with active biceps contraction.
the labrum lift superiorly and compression of the glenohumeral joint. However, other studies showed no humeral head motion with active biceps contraction.
Electromyography (EMG) studies have also demonstrated varying findings. Basmajian (8) demonstrated that the LHB did have EMG activity during active shoulder flexion. The LHB was estimated to contribute 7% of the power of shoulder flexion. Jobe et al. (9) showed peak biceps activity during follow through and deceleration in the throwing motion. However, in separate studies, Yamaguchi et al. (10) modified the EMG experiment to control (limit) elbow flexion and showed minimal to no EMG activity during isolated shoulder flexion. Another intriguing EMG finding has been an increase in EMG activity of the LHB in patients with rotator cuff deficiency. This increased activity may result in increased tendon diameter. Although still somewhat controversial, there is current literature that suggests the LHB has a depressing function in the shoulder and helps stabilize the humeral head in the glenoid. Even so, these effects are not dramatic.
Pathophysiology
Multiple classification schemes have been developed to describe disorders of the LHB tendon. These divisions have been only marginally useful with regard to diagnostic and treatment decisions. Understanding the various pathologic processes involving the biceps tendon and how to treat each process is more important. The three biceps tendon pathologies discussed here are biceps tendinitis, rupture, and instability.
BICEPS TENDINITIS
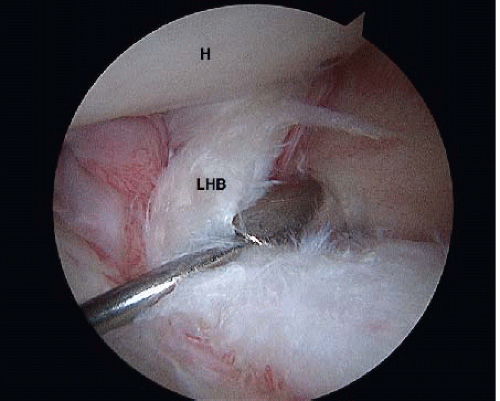
Biceps tendinitis can be referred to as primary or secondary. Primary tendinitis involves inflammation of the tendon within the BG. To be considered primary, no other pathologic findings (such as impingement, bony abnormalities within the groove, or biceps subluxation) should be present. It is considered an uncommon condition, and Habermayer and Walch (11) felt that this diagnosis could only be made during arthroscopy. Visualization of that part of the LHB in the groove is facilitated by pulling the tendon into the joint with a probe or advancing the scope into the BG (Fig. 15.4).
Secondary biceps tendinitis is more common and well recognized. The LHB coexists with the anterior supraspinatus and superior subscapularis under the anterolateral acromion and, therefore, is affected by the same forces. Although subacromial impingement produces undue forces on the anterior rotator cuff, it also compresses the underlying LHB and produces concomitant pathology (and thereby symptoms) in this structure. In fact, the impingement upon the LHB worsens as a rotator cuff tear progresses and increased contact between the LHB and the coracoacromial arch occurs. Up to one-third of patients with rotator cuff disease will have biceps involvement.
Another potential cause of secondary biceps tendinitis is the presence of bony anomalies of the proximal humerus. Most commonly these bony anomalies are secondary to malunion or nonunion of a proximal humerus fracture. If a fracture extends into the BG, significant irritation of the LHB can occur. Younger patients with biceps tendinitis may be more likely to have groove anomalies such as narrowing or osteophytes, but it is difficult to determine the sequence of events in such conditions.
BICEPS TENDON RUPTURE
While acute ruptures of the LHB do occur, they are more commonly the end result of chronic biceps tendinitis and impingement and frequently associated with rotator cuff disease. Acute ruptures can occur with a fall on an outstretched hand or with rapid deceleration of the arm during throwing activities. In this case, the deceleration force can result in trauma to the origin of the LHB resulting in a SLAP lesion. If the force is great enough from a single traumatic event or on a repetitive basis, it can result in LHB rupture with or without an associated SLAP tear.
Chronic biceps tendinitis is a more common cause for LHB rupture and tends to occur from repetitive overuse with the arm in adduction and internal rotation or from multidirectional or inferior instability. The LHB becomes attenuated and weakened by the continued impingement between the humeral head and the coracoacromial arch. In the case of impingement causing a rupture, the rupture typically occurs around the area of the rotator cuff interval (a weak point for the LHB) rather than at its origin.
BICEPS INSTABILITY
Biceps instability takes the form of either frank dislocation or more subtle subluxation. As previously noted, the
primary restraining structures holding the LHB in the BG are the medial sling and subscapularis tendon. Habermayer and Walch (11) divided LHB tendon dislocations into extra-articular and intra-articular. The much less common extra-articular dislocations dislodge from the BG and travel over (anterior to) an intact subscapularis tendon. Extraarticular dislocations are extremely uncommon and occur with roof disruption due to CHL and supraspinatus tears.
primary restraining structures holding the LHB in the BG are the medial sling and subscapularis tendon. Habermayer and Walch (11) divided LHB tendon dislocations into extra-articular and intra-articular. The much less common extra-articular dislocations dislodge from the BG and travel over (anterior to) an intact subscapularis tendon. Extraarticular dislocations are extremely uncommon and occur with roof disruption due to CHL and supraspinatus tears.
The more common intra-articular LHB dislocation is associated with a partial or complete tear of the subscapularis tendon, which allows the LHB to dislocate posterior to the subscapularis. The medial sling remains attached to the superolateral border of the subscapularis tendon—even when that tendon retracts medially. This arthroscopic anatomic landmark has been termed the “comma sign” (5). It is a critical arthroscopic finding because the comma easily guides the surgeon to the superolateral border of the subscapularis tendon, thereby assisting in anatomic arthroscopic repair of the tendon back to the lesser tuberosity bone bed (8) (Fig. 15.3).
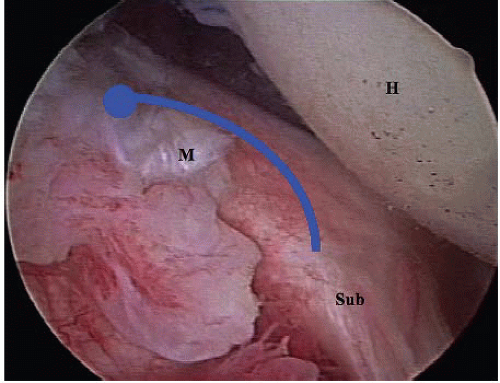
Biceps tendon subluxation can be a much more subtle diagnosis and is frequently missed even during arthroscopy. Walch has referred to this as the “hidden lesion.” As with dislocation, the critical anatomic components that prevent biceps subluxation are the medial sling and subscapularis tendon. In the early phases of biceps subluxation, the medial sling structures may remain largely intact while creating mechanical wear to the anteromedial portion of the LHB, which resides in the BG. It is, therefore, quite important to thoroughly examine the anteromedial portion of the LHB by pulling the structure intra-articularly with a probe while visualizing “over the top.” As the pathology progresses, the medial sling becomes detached from its insertion on the superior aspect of the lesser tuberosity and the LHB begins to act as a knife cutting its way through the subscapularis tendon insertion, detaching it from the lesser tuberosity. Early findings of this phenomenon can only be seen with the 70° scope visualizing “over the top” to look down at the bone bed of the lesser tuberosity. Lo and Burkhart (5) have described this view with the 70° scope as the “aerial view.”
As the humerus is internally and externally rotated the biceps tendon can be seen “breaking” posterior to the plane of the anterior border of the subscapularis (Fig. 15.5). As a normal biceps tendon should remain anterior to the plane of the subscapularis, this “broken plane” phenomenon is a sure sign of early biceps instability and if not recognized will likely progress to LHB dislocation and complete tearing of the upper subscapularis insertion.
CLINICAL EVALUATION
Pertinent History
Anterior shoulder pain (particularly in the region of the BG) is the hallmark of biceps tendon problems. With biceps tendinitis, the pain is usually described as a chronic aching pain, which is worsened by lifting and overhead activities. The pain frequently radiates distally to approximately the mid-arm level, but seldom radiates proximally. There is such a close association between subacromial impingement and biceps tendinitis that the two conditions have closely overlapping symptoms. They can be very difficult to distinguish and generally occur in tandem. Biceps instability may present with a painful click with arm elevation and/or rotation. Symptoms can be very similar to biceps tendinitis and are frequently seen at the same time.
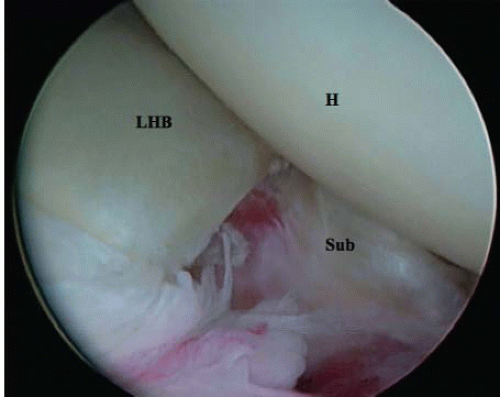 FIGURE 15.5. The LHB tendon is seen cutting posterior to the plane of the torn anterior subscapularis (Sub). |
Patients who present with rupture of the LHB are usually much easier to diagnose. These patients complain of a history of chronic anterior shoulder pain consistent with biceps tendinitis and/or impingement. Then, they usually report an episode of a painful “pop” in the shoulder, which was followed by partial or complete relief of their impingement symptoms. Subsequently, they may develop ecchymosis in the arm and an associated muscular deformity in the arm—frequently termed the “Popeye” muscle (Fig. 15.6). Sometimes, the “Popeye” deformity does not develop because the LHB becomes incarcerated in a stenotic BG.
Physical Examination
Distinguishing anterior shoulder pain caused by biceps tendon disorders as opposed to subacromial impingement can be difficult, as these two entities usually coexist. Although there are some exam maneuvers that attempt to isolate the biceps tendon, there is still a fair amount of overlap and the definitive diagnosis of isolated biceps tendon pathology is extremely difficult based on history and physical exam alone. Often selective injections are helpful in differentiating the etiology of the pain.
The hallmark of biceps tendon pathology is point tenderness in the BG. Without this finding, it is extremely unlikely the LHB is involved in the patient’s symptoms. The BG is best palpated approximately 3 below the acromion with the arm in 10° of internal rotation. As the arm is internally and externally rotated, the pain should move with the arm (Bennett rotation test). This is distinct from subacromial bursitis where the pain location remains relatively constant despite the position of the arm. This “tenderness in motion” sign can be quite specific for biceps tendon disorders. In the situation in which it is unclear whether the pain is secondary to the LHB or to possible impingement/bursitis, selective injections of these areas can help make the diagnosis.
There are several provocative tests, which can be helpful in the diagnosis of LHB pathology. However, the sensitivity and specificity of these tests intended for the diagnosis of LHB pathology are questionable.
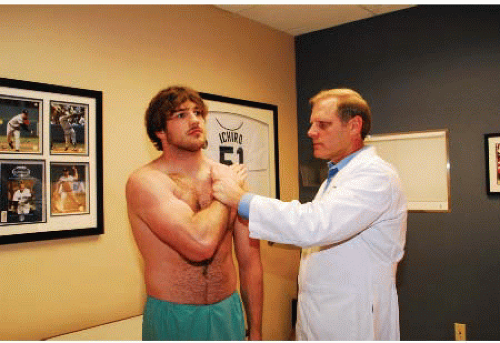
Speed’s test (12) (Fig. 15.7)—With the elbow in extension, the patient flexes the shoulder against resistance from the examiner. Pain in the BG is considered positive.
Yergason test (13)—The patient attempts to supinate the wrist against resistance (with the elbow flexed at the side). Pain in the BG is considered positive.
Bear hug test (14) (Fig. 15.8)—This test was developed by Barth et al. to better isolate upper subscapularis lesions. Since these lesions are almost always associated with LHB instability, it is a good test for LHB pathology. The patient places the open palm of the affected extremity on the contralateral shoulder. In so doing, the ipsilateral elbow is held well anterior to the plane of the patient’s body. As the examiner tries to lift the hand off the shoulder (resisted internal rotation), the patient tries to keep the palm on the shoulder. Weakness (in comparison with the contralateral side) is a positive test and indicative of a tear of the upper subscapularis (and thereby likely LHB instability). In general, the examiner should not be able to lift the hand off the contralateral shoulder unless there is tearing of the upper subscapularis, in which case there is usually concomitant subluxation of the biceps tendon.
 FIGURE 15.7. Speed’s test: The examiner applies a downward force to the patients extended arm while the patient resists the downward force. Pain in the region of the biceps tendon is positive. |
Napoleon test (15, 16) (Fig. 15.9)—This test also attempts to assess the integrity of the subscapularis. The patient
pushes on the abdomen with the palm of the affected extremity and tries to keep the wrist completely straight. If the patient is unable to keep the wrist straight, but rather flexes the wrist to perform the test, this is considered a positive or intermediate test and suggestive of a subscapularis tear.
pushes on the abdomen with the palm of the affected extremity and tries to keep the wrist completely straight. If the patient is unable to keep the wrist straight, but rather flexes the wrist to perform the test, this is considered a positive or intermediate test and suggestive of a subscapularis tear.
Belly-press test (16, 17) (Fig. 15.10)—This test is similar to the Napoleon test in that the patient places the palm on the abdomen with the wrist held straight. The physician then tries to pull the hand off the abdomen. If the physician is able to pull the hand off easily, this is considered a positive test and suggestive of a subscapularis tear.
Lift-off test (18) (Fig. 15.11)—This is the fourth test to assess subscapularis integrity. The patient places the back of the hand of the affected extremity on the ipsilateral buttock. The examiner then lifts the hand posteriorly and asks the patient to hold it in that position. Weakness or inability to lift the hand off the lower back is considered positive and suggestive of a subscapularis tear.
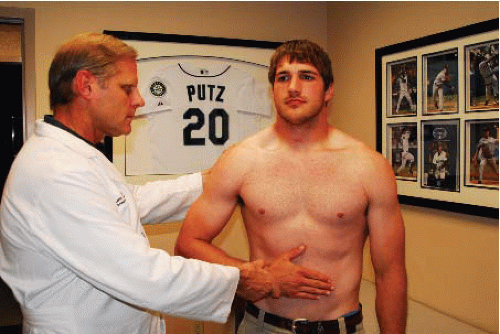 FIGURE 15.10. Belly-press test: Examiner resists patient pressing against his abdomen. If the examiner is able to lift hand from abdomen, this is a positive test. |
 FIGURE 15.11. Lift-off test: The patient is asked to place the hand behind the back and then lift the dorsum of the hand off the back. Inability to do so is considered a positive test. |
The biceps instability test (18)—This test is performed to demonstrate biceps subluxation. It is performed with the shoulder abducted 90° and with full external rotation while palpating over the BG. As the arm is internally rotated, an audible or palpable click occurs as the biceps subluxates over the lesser tuberosity.
The Ludington test—This test is utilized when a biceps rupture is not clearly visible. The patient places both hands behind his head and flexes the biceps. The contour of the muscle can be better appreciated in this position.
The described tests can be useful in assisting the clinician with the diagnosis of biceps tendon disorders. However, the sensitivity/specificity of most of these tests has not been examined. The exceptions include Speed’s test, which Bennett (19) determined to be 90% sensitive for shoulder pain but only 13% specific for bicipital pathology. Its positive predictive value was 23%, whereas its negative predictive value was 83%. The bear hug test was determined to have a sensitivity of 60% and specificity of 92% for tears of the upper subscapularis (17).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree