Basics of Elbow Arthroscopy: Positioning, Setup, Anatomy, and Portals
William B. Stetson
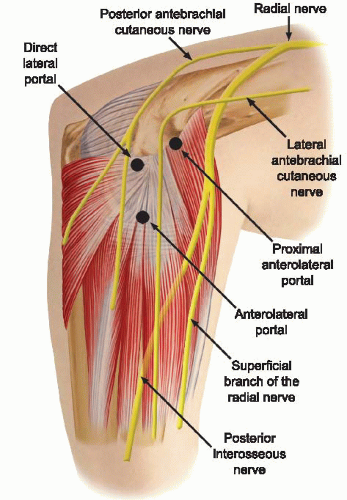
Elbow arthroscopy is a technically demanding procedure. When performed with appropriate judgment and technique, elbow arthroscopy is an excellent tool for the correction of many lesions of the elbow joint and provides an opportunity for both diagnostic and therapeutic intervention with minimal risk (1). However, arthroscopy of the elbow joint is perhaps the most hazardous in terms of its potential for causing injury to important nearby nerves and vessels. The reason for this relates to the complex relationship of these structures to the joint (2) (Fig. 31.1). Because of the surrounding neurovascular structures, familiarity with the normal elbow anatomy and portals will decrease the risk of damage to important structures.
In 1985, Andrews and Carson (3) described the patient-supine technique and the use of various portals for elbow arthroscopy. In 1989, Poehling et al. (4) described the patient-prone position for elbow arthroscopy. Since then, the techniques and indications for elbow arthroscopy have expanded and there have been many more reports describing variations in operative technique. The purpose of this chapter is to give an overview of positioning, setup, anatomy, and the portals used for elbow arthroscopy.
ANATOMY
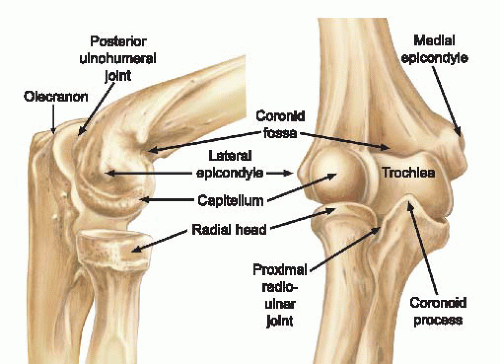
A clear understanding of the anatomy of the elbow is important before proceeding with arthroscopy. Important bony anatomic landmarks should be palpated, which include the lateral and medial epicondyle, the olecranon process, and the radial head (Fig. 31.2). On the lateral side, the lateral epicondyle, the olecranon process, and the radial head form a triangle. Located in the center of this triangle is a “soft spot” called the anconeus triangle. This is often used to inflate the joint with fluid before introducing any instruments or cannulas and can also be the landmarks for a direct lateral portal (Fig. 31.3). Posteriorly, important structures include the triceps muscle, tendon, and the tip of the olecranon.
Anteriorly, the antecubital fossa is formed by three muscular borders: laterally, by the “mobile wad of three”—the brachioradialis, the extensor carpi radialis brevis, and the extensor carpi radialis longus muscles; medially, by the pronator teres muscle; and, superiorly, by the biceps muscle. The anconeus muscle, which is located on the posterolateral aspect of the joint, originates on the lateral epicondyle and posterior elbow capsule and inserts on the proximal ulna.
Sensory nerves around the elbow include the medial brachial cutaneous, the medial antebrachial cutaneous, the lateral antebrachial cutaneous, and the posterior antebrachial cutaneous nerves. The medial brachial cutaneous nerve penetrates the deep fascia midway down the arm on the medial side and supplies skin sensation to the posteromedial aspect of the arm to the level of the olecranon. The medial antebrachial cutaneous nerve supplies sensation to the medial side of the elbow and forearm. The lateral antebrachial cutaneous nerve is a branch of the musculocutaneous nerve, which exits between the biceps and the brachialis muscles laterally to supply sensation to the elbow and lateral aspect of the forearm. Finally, the posterior antebrachial cutaneous nerve branches from the radial nerve and courses down the lateral aspect of the arm to supply sensation to the posterolateral elbow and posterior forearm (5).
The main neurovascular structures about the elbow are the median nerve, radial nerve, ulnar nerve, and brachial artery. The radial nerve spirals around the posterior humeral shaft, penetrates the lateral intermuscular septum, and descends anteriorly to the lateral epicondyle between the brachioradialis and the brachialis muscles. The radial nerve then branches to form the superficial radial nerve, which supplies sensation to the dorsoradial wrist and posterior surface of the radial three and one-half digits, and the posterior interosseous nerve, which provides motor branches to the wrists, thumb, and finger extensors. The ulnar nerve penetrates the medial intermuscular septum in the distal one-third of the arm, courses posteriorly to the median epicondyle, and then descends distally between the flexor carpi ulnaris and the flexor digitorum superficialis muscles. Finally, the brachial artery courses just medial to the biceps tendon in the antecubital fossa
and then descends to the level of the radial head, where it bifurcates into the radial and ulnar arteries (5) (Fig. 31.1).
and then descends to the level of the radial head, where it bifurcates into the radial and ulnar arteries (5) (Fig. 31.1).
CLINICAL EVALUATION
History
A comprehensive history should be taken including the occupation of the patient, whether they are right or left handed, and the duration of their symptoms. It is also important to determine the details of whether their symptoms started with a single traumatic event or from repetitive activities. One should inquire about the presence and character of the pain, swelling, locking, and catching episodes, which can indicate intra-articular loose bodies. The location of the pain is also important as medial pain is most often medial epicondylitis, but can also be a medial epicondyle avulsion fracture, a medial collateral ligament sprain, ulnar neuritis, or ulnar nerve subluxation.
Symptoms in the lateral region of the elbow may be indicative of radiocapitellar chondromalacia, osteochondral loose bodies, radial head fracture, osteochondritis dissecans (OCD) lesions, and most commonly lateral epicondylitis.
The differential diagnosis for symptoms of the anterior elbow includes distal biceps tendon rupture, which can be partial or complete, an anterior capsular strain, and a brachioradialis muscle strain (6).
Symptoms in the posterior compartment can reflect valgus extension overload syndrome, posterior impingement, osteochondral loose bodies, triceps tendonitis, triceps tendon avulsion, or olecranon bursitis (7). Deep, aching pain in the posterior region of the elbow may also be indicative of an olecranon stress fracture (8).
A careful neurovascular history is also important as ulnar nerve paresthesias can be the result of cubital tunnel syndrome, a subluxing ulnar nerve, or a traction injury from valgus instability (5).
Throwing athletes are a unique patient population and it is important to gather information about prior injury and any changes in the throwing mechanism or rehabilitation regimen (6). A patient whose symptoms are related to throwing and are located medially may have an injury to the medial collateral ligament. Throwing athletes who report lost velocity and control or inability “to let the ball go” may have pain posterior on forced extension, which could be a sign of posterior olecranon impingement secondary to a medial collateral ligament injury. The typical patient is a baseball pitcher in his mid-20s who has posterior elbow pain during the acceleration and follow-through phases of pitching and complains of the inability to fully extend the elbow (5). Young throwing athletes (<18 years) with OCD lesions often report progressive lateral elbow pain during late acceleration and follow-through phases, with loss of extension and episodes of locking (7).
Physical Examination
A careful physical examination of all three compartments of the elbow is critical to determine the correct diagnosis. Each compartment should be examined individually in order to fully evaluate the elbow. The physical examination starts with careful inspection of the skin and soft tissues to make sure there are no scars, swelling, ecchymosis, soft-tissue masses, or bony abnormalities. The alignment of the elbow should also be inspected noting any significant varus or valgus deformities. Range of motion of the elbow in flexion, extension, supination, and pronation should be noted and compared with the contralateral side. Those with posteromedial impingement or valgus extension overload may reveal a flexion contracture and pain over the posteromedial olecranon tip (5).
Medially, pain along the medial aspect to palpation at the medial epicondyle usually indicates medial epicondylitis with provocative testing with the elbow extended and resisted wrist flexion reproducing the pain. In adolescents, pain medially can suggest a medial epicondyle avulsion fracture. It is important to differentiate medial epicondylitis from an injury to the ulnar or medial collateral ligament. Pain just distal to the medial epicondyle along the medial collateral ligament is usually indicative of an injury to the ligament. Palpation of the proximal flexor-pronator mass can indicate tendinopathy. The ulnar nerve should also be palpated, and a Tinel’s sign demonstrates ulnar neuropathy. The elbow is also flexed and extended as the nerve is palpated to determine whether the nerve subluxates.
One should test for valgus instability with the elbow flexed to 30° to relax the anterior capsule and free the olecranon from its bony articulation in the olecranon fossa. A valgus stress is then applied with the elbow in full supination. Discomfort along the medial aspect of the elbow can indicate ulnar collateral ligament injury. Valgus laxity, however, is often difficult to discern, particularly if there is tearing of the undersurface of the ulnar collateral ligament (9). Comparing the contralateral elbow can help differentiate physiologic laxity from pathologic instability.
Posteriorly, the triceps muscle insertion and the posterolateral and posteromedial joint areas are palpated to assess for tenderness, bone spurs, and posterior impingement lesions. The so-called clunk test is performed to demonstrate posterior olecranon impingement. The upper arm is grasped and stabilized as the elbow is brought into full extension. Reproduction of pain at the posteromedial aspect of the joint suggests compression of the olecranon into the fossa and indicates valgus extension overload.
Laterally, the lateral epicondyle and extensor origin are palpated to assess for lateral epicondylitis. The radiocapitellar joint is palpated while the forearm is pronated and supinated to elicit crepitus or catching, which can be caused by chondromalacial lesions or impingement from a lateral synovial fringe. The “soft spot” is also inspected to determine whether there is synovitis or an effusion in the elbow joint (5).
Stability can be assessed with O’Driscoll’s posterolateral rotatory instability test (10). The test is best done under general anesthesia because of the patient’s apprehension while awake, which may give a false-negative result. However, it can be done with the patient awake with the extremity over the patient’s head and the shoulder in full external rotation. During the test, a valgus, supination, and axial compression load is applied to the elbow, which is flexed approximately 20° to 30°. With the elbow in extension, subluxation or dislocation of the radius and of the proximal ulna creates a posterior prominence and sulcus sign. When the elbow is flexed, radiohumeral and ulnohumeral joints are visibly or palpably reduced (5).
A careful neurovascular examination should be done on every patient paying close attention to the ulnar nerve medially to differentiate cubital tunnel syndrome from concomitant medial epicondylitis or a medial collateral ligament injury.
Diagnostic Imaging
Routine diagnostic radiographs include an anterior-posterior (AP) view with the elbow in full extension and a lateral view with the joint in 90° of flexion. An axial view can also be obtained to outline the olecranon and its medial and lateral articulations. This is the best view for identifying and assessing a posteromedial osteophyte. When there is a history of trauma, an oblique view should also be done and careful attention should be paid to the radial head and the coronoid process for subtle fracture lines. Also, X-rays should be reviewed for more obvious anterior or posterior elbow dislocations along with more subtle degenerative changes, osteophytes, and loose bodies. However, plain radiographs are not always able to demonstrate all loose bodies.
A gravity stress test radiograph can be used to detect valgus laxity of the elbow. The patient is placed in a supine position and the shoulder is abducted and brought to maximum external rotation so that the elbow is parallel to the floor. If there is an injury to the ligament or bony attachment, increased joint space can be seen on radiographs (5).
Both MRI and CT arthrogram have been found to be accurate in diagnosing a complete tear of the ulnar collateral ligament (9). Early studies found CT arthrogram is more sensitive in detecting a partial undersurface tear of the ulnar collateral ligament (11). This was described as a “T sign” lesion by Timmerman and Andrews that represents dye leaking around the detachment of the deep portion of the ulnar collateral ligament (UCL) from its bony insertion, but remaining within the intact superficial layer, UCL, and capsule (9). MRI may not demonstrate subtle undersurface tears of the ulnar collateral ligament. Magnetic resonance arthrography with saline contrast or gadolinium, however, can increase the sensitivity for detecting undersurface tears of the ulnar collateral ligament and has now become the test of choice to detect these tears (9).
MRI is also useful for evaluating osteochondral lesions in the radiocapitellar joint and for demonstrating early vascular changes that are not yet apparent on plain radiographs and it can be used to assess the extent of the lesion and displacement of fragments (5). MRI is also helpful for evaluating the soft-tissue structures of the elbow including the tendinous insertions of the flexor and extensor musculature to help in diagnosing medial and lateral epicondylitis, the triceps insertion and associated musculature to evaluate for triceps tendonitis.
Decision-Making Algorithms
Appropriate conservative measures should always be tried before making the decision to proceed with elbow arthroscopy depending on the diagnosis. The indications include treatment for the diagnosis of intra-articular lesions of the elbow, the removal of loose and foreign bodies, irrigation of the joint, debridement of an infected joint, excision of osteophytes, treatment for lateral epicondylitis, and the treatment of intra-articular fractures. Each of these diagnoses has its own types of conservative treatments, which should be rendered before proceeding with elbow arthroscopy and are discussed in detail in later chapters.
TREATMENT
Nonoperative Treatment
Appropriate conservative measures should always be tried before making the decision to proceed with elbow arthroscopy. However, many times the diagnosis is not often clear until the time of diagnostic arthroscopy as loose bodies, articular cartilage damage, or other pathology cannot always be detected by physical examination, X-ray, or MRI.
Operative Indications
In 1992, O’Driscoll and Morrey (12) described the early indications for elbow arthroscopy, which was pain or symptoms that were substantial enough to interfere with work, daily activities, sports, or sleep and did not resolve after conservative treatment. In this early study, they analyzed their results of 71 elbow arthroscopies as the indications for such a procedure were evolving. Not surprising, the best early results were seen for arthroscopic removal of loose bodies, assessment of undiagnosed snapping, idiopathic flexion contractures, local debridement of damaged articular surfaces, and synovectomy. They found that the patients least likely to benefit were the ones in whom there was a disparity between objective and subjective findings.
Since then, the indications for elbow arthroscopy have evolved. In 1994, Poehling and Ekman (1) further refined the indications that included its use for the diagnosis of intra-articular lesions of the elbow, the removal of loose and foreign bodies, irrigation of the joint, debridement of an infected joint, excision of osteophytes, synovectomy, capsular release, excision of the radial head, and treatment of acute fractures of the elbow.
A number of authors have since reported on the usefulness of elbow arthroscopy for the removal of loose bodies (3, 5, 12, 13 and 14), and this continues to be the primary indication for elbow arthroscopy. Several pathologic processes may initiate the formation of a loose body including trauma and synovial chondromatosis. Regardless of the etiology, the patients usually present with swelling, locking, pain, and loss of motion, all of which can be improved with the removal of loose bodies. These loose bodies can be found both in the anterior and posterior compartment and also in the posterior medial gutter and removing them can be a technically demanding procedure.
Elbow arthroscopy can also be an effective tool if the diagnosis of an infection is made or suspected. It is a less invasive way to enter into the joint with minimal trauma to confirm the diagnosis of an infection, irrigate the joint, debride infected tissue, and assess the condition of the underlying bone, cartilage, and synovial tissue (1).
The presence of osteophytes, or osseous spurs, is another condition that lends itself to arthroscopic management and removal (12, 13, 14 and 15). A true lateral radiograph of the elbow is useful for the identification of osteophytes that may limit full extension of the elbow with impingement of the posterior olecranon spur in the olecranon fossa (1, 12). An axial view may also show a posteromedial osteophyte (5). This can be easily removed arthroscopically.
The term “valgus extension overload” was coined to describe these findings, which can be found in baseball pitchers and other overhead athletes. The tremendous repetitive valgus forces generated during the acceleration and follow-through phases of pitching, as the elbow goes into extension, can result in osteochondral changes in the olecranon and distal humerus. A significant osteophyte
forms on the posteromedial aspect of the olecranon fossa with continued pitching or overhead activities, creating an area of chondromalacia (5). The inability to reliably visualize the anterior bundle of the medial collateral ligament with the arthroscope limits the value of the arthroscope when assessing medial collateral ligament injuries (16, 17).
forms on the posteromedial aspect of the olecranon fossa with continued pitching or overhead activities, creating an area of chondromalacia (5). The inability to reliably visualize the anterior bundle of the medial collateral ligament with the arthroscope limits the value of the arthroscope when assessing medial collateral ligament injuries (16, 17).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree