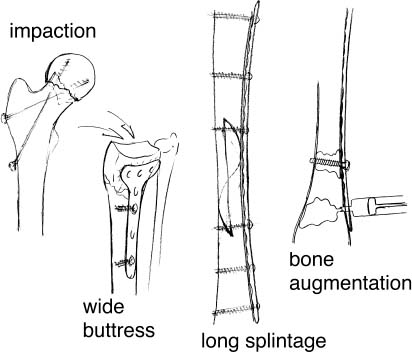
Chapter 7 Restoration of best possible function is the common aim of fracture treatment. For the senior population special considerations are given to the possible ways to obtain the desired functional restoration. Treatment options can differ significantly from those applicable to a young adult. The main difference is the quality of the bone and hence the potential of obtaining a secure purchase of the available fixation devices. Further difficulties may arise if the patient’s ability to cooperate is reduced as overload of the compound system may lead to failure. Preoperative planning begins with the definition of realistic goals. Rapid restoration of mobility should be the most important short-term goal in this group of patients. The relative merits of conservative versus operative treatment should be carefully weighted. If operative treatment is chosen, the procedure selected should be the least invasive, yielding a low complication rate and warranting an adequate long-term outcome. As in general fracture treatment the correct balance between mechanical stability and preservation of bone perfusion is the key issue to obtain a successful osteosynthesis. The issue is embraced by the term “biological osteosynthesis.” The reader is referred to Mast and coworkers’ classic work1 where the essentials of minimal exposure and indirect reduction techniques are exposed. Fractures of the lower extremity require a fairly stable fixation because early mobilization is the main concern. Operative treatment is generally indicated to avoid restrictive and dangerous immobilization. The main dangers of immobilization arise from cardiopulmonary and thromboembolic complications. Given the difficulties the elderly may have in complying with limited weight-bearing protocols, any osteosynthesis must be stable enough to resist the occasional uncontrolled full weight bearing. Alternatively the fixation must be externally protected, inevitably losing some of the benefits of early mobilization. For fractures of the upper extremity conservative treatment is indicated in a large number of patients. Splints, casts, or bandages do not excessively limit ambulation, provided that the lower extremities are functional, although the marginally autonomous patient may become temporarily or permanently dependent and therefore requires special consideration. It may be necessary to treat upper limb injuries operatively to allow a marginally compensated patient to remain in his usual environment or to facilitate the use of crutches and similar devices in multiply injured patients. Since the impaired anchorage of the implant jeopardizes osteosynthesis of osteoporotic bone, solutions are directed toward increasing the stability of the compound system by transferring more load to the bone thus relatively unloading the implant. The implant should be used in a load-sharing rather than in a load-bearing configuration. A complementary approach is the modification and adjustment of the implants to the specific requirements of osteopenic bone. In the diaphysis, osteoporosis is associated with a reduction of cortical thickness and an increasing width of the medullary cavity.2,3 Also, the material properties of cortical bone deteriorate with increasing age and the bone becomes increasingly brittle, which may lead to micro- and macrocracking when standard screws are inserted. Both processes will reduce the holding strength of cortical screws. It has been shown that reduction of cortical thickness and the inclination of screw threads are directly proportional to the holding strength.4 These findings have led to extensive basic research to optimize screw design. Morphologic and mechanical changes of cancellous bone are also of concern. The main process is rarefaction of trabeculae. Initially, a relative thickening of the mechanically relevant trabeculae might compensate for the general rarefaction. With time the remaining trabeculae will gradually be resorbed. It is essential to understand that screw purchase in advanced osteopenia relies essentially on the thin shell of peripheral cortical bone and not on the cancellous trabeculae. A pertinent comparison can be made with a fractured egg shell that requires a wide buttress (using an eggcup for instance) to provide adequate support. Oversized, stiff, and nonforgiving implants should be avoided. It is preferable to use elastic fixations that may temporarily give way and that are better adapted to the weak bone. FIGURE 7–1 Four basic principles to obtain stable fixation of osteoporotic bone. For practical purposes, basic principles of internal fixation in osteoporotic bone are: impaction, wide buttress, long splintage, bone augmentation, and bone substitution (Fig. 7–1). The chosen method should be as forgiving as possible and should allow the inevitable occasional overload imposed on the construct by a marginally cooperating patient. Impaction is a key factor in stability. In many cases impaction is created by the trauma itself. A typical example is the valgus impacted abduction fracture of the femoral neck. The primary stability induced by impaction of the fragments may be sufficient for functional rehabilitation. Also valgus impacted fractures of the proximal humerus, impacted fractures of the distal radius, and compression fractures of the vertebral bodies generally have sufficient stability for functional rehabilitation. Taking advantage of the benefits of impaction is a useful concept that should be applied in the osteosynthesis of osteoporotic bone whenever possible. For instance, the strength of fixation of pertrochanteric fractures may be significantly improved when impaction of the main fragments is obtained previous to the application of the definitive fixation device. In practical terms this can be achieved by the following steps: (1) preliminary reduction of the main fragments (abduction and internal rotation); (2) preliminary fixation with Kirschner wires; (3) impaction of the main fracture fragments using a broad impactor (a conventional slotted hammer will do) placed over the trochanteric region and hit with a heavy mallet. Following impaction a suitable implant such as a hip sliding screw may be used. Controlled impaction can also be achieved by deliberately tensioning internal fixation devices (plate, wire, or nail). One should consider that compression of fracture planes dramatically increases the stability of the compound system. The concept is to shift from a load-bearing to a load-sharing constellation thus relatively unloading the implant. Controlled impaction can also be planned to occur in the postoperative phase, as is the case for a number of K-wire fixations and endomedullary fixations. The concept of postoperative gradual and controlled impaction has several advantages. The main advantage is its forgiveness. The dynamic hip screw illustrates this concept. The implant acts as a rail on which axial movement is allowed. Weight bearing leads to gradual impaction, thus increasing stability of the fixation. The disadvantage of postoperative autoimpaction is the limited control that the surgeon may have on the amount of the originating deformity. Overimpaction is not infrequent and may lead to clinical problems such as femoro-acetabular impingement. Nevertheless the degree of the deformity is fortunately usually well tolerated by the elderly patient and may be looked upon as the price to pay for stability and consolidation.
BASIC PRINCIPLES AND
TECHNIQUES OF INTERNAL
FIXATION IN OSTEOPOROTIC BONE
PRINCIPLES OF INTERNAL FIXATION OF OSTEOPOROTIC BONE
IMPACTION
WIDE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree