20. Bacterial and fungal skin infections
Pathogenesis and risk factors
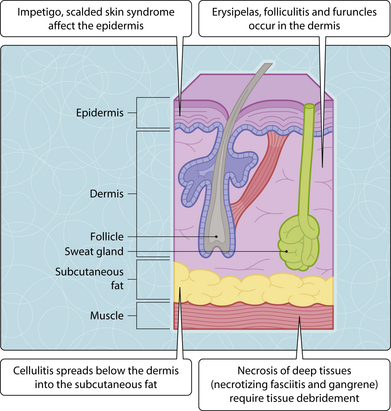
Some infections involve only the superficial structures of the skin, while others affect the deeper soft tissues below the dermis (Fig. 3.20.1). The infection may be localized or spreading depending on the tissue plane involved and the virulence of the pathogen.
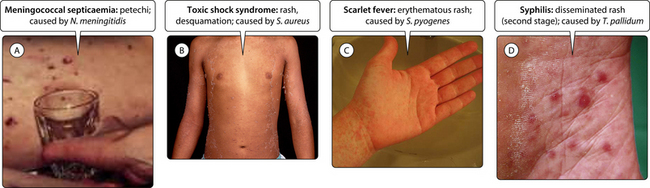
Bacterial super-infections may complicate skin disorders such as eczema. In addition some systemic infections also present with skin features (Fig. 3.20.2).
Bacterial skin infections
Synergistic gangrene is a polymicrobial infection (multiple different bacteria) that leads to necrosis of the groin and genital soft tissue. Necrotizing or gangrenous conditions require antibiotics and extensive debridement to avoid a fatal outcome.
Mycobacterial infections of the skin in primary infection with M. tuberculosis (lupus vulgaris) is rare, whereas M. leprae classically causes red anaesthetic lesions on the face, body and limbs in tuberculoid leprosy (Ch. 15). Other skin infections may be caused by atypical mycobacteria, notably the ‘fish-tank’ or ‘swimming pool’ granuloma (M. marinum) or the necrotizing tropical Buruli ulcer (M. ulcerans).