Avoiding Complications in Elbow Arthroscopy
Rhett E. Hobgood
Larry D. Field
Elbow arthroscopy is a useful technique in the management of various pathologic conditions. It has demonstrated utility in the treatment of loose bodies, plicae, osteoarthritis, rheumatoid arthritis, osteochondritis dissecans, contracture, fractures, and even some causes of elbow instability. However, it is a technically demanding procedure due to the remarkable congruity of the articular surfaces as well as the close proximity of neurovascular structures. Because of these factors, complications can often occur.
Complications include superficial infection, persistent drainage from portal sites, postoperative contracture, compartment syndrome, septic arthritis, and, most commonly, nerve injury. Some authors have shown the rate of complications after elbow arthroscopy to be much higher (approximately 10%) than that reported after knee or shoulder arthroscopy (1% and 2%). Although permanent neurologic injuries are uncommon, when they do occur, they can be devastating.
Avoiding complications requires a thorough knowledge of both intra-articular and extra-articular anatomy of the elbow combined with a systematic operative technique. The aim of this chapter is to help surgeons avoid complications by reviewing anatomic considerations, proper positioning, and use of instruments. Specific complications and associated risk factors are also discussed. Finally, we present the authors’ preferred method of treatment and situations that deserve special consideration.
ANATOMIC CONSIDERATIONS
Neurovascular injury is the primary concern during elbow arthroscopy. Understanding several important anatomic considerations can help decrease the likelihood of injuring these vital structures. These considerations influence our surgical technique in the following ways: (1) marking anatomic landmarks prior to initiating the procedure, (2) positioning the elbow in 90° of flexion, (3) understanding the effect of joint distention on the relationship between the joint capsule, the bone, and the neurovascular structures, (4) incising only the skin to protect cutaneous nerves, and (5) utilizing proximal portals in the anterior compartment.
The bony landmarks of the elbow, the ulnar nerve, and the portal sites are marked on the skin prior to joint distention (Fig. 39.1). This is important because anatomic landmarks may become obscured secondary to swelling once the procedure is initiated. The important bony landmarks to outline include the medial and lateral epicondyles, radial head, and olecranon. It is especially important to mark the position of the ulnar nerve, as subluxation and anterior dislocation can occur in approximately 16% of the population. This can place it at risk during the placement of the anteromedial portal.
Positioning the elbow in 90° of flexion is recommended. In this position, the neural structures are further away from both the bone and the capsule than in the extended position. Miller et al. demonstrated in a cadaveric study that the capsule-to-nerve and the bone-to-nerve
distances increased for both the radial and the median nerves in flexed elbows when compared with matched extended elbows. However, they found that the distance between the ulnar nerve and the capsule did not vary with elbow flexion and extension, remaining essentially on the capsule in most specimens. Most importantly, elbow extension eliminates the protective effect of insufflation.
distances increased for both the radial and the median nerves in flexed elbows when compared with matched extended elbows. However, they found that the distance between the ulnar nerve and the capsule did not vary with elbow flexion and extension, remaining essentially on the capsule in most specimens. Most importantly, elbow extension eliminates the protective effect of insufflation.
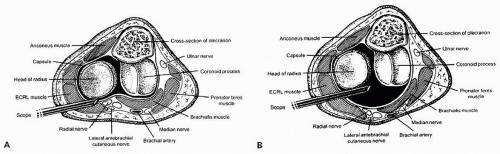
Joint insufflation with 20 mL of sterile saline should always be performed prior to portal placement. Insufflation increases the distance between the bone and the radial and median nerves. However, the bone-to-ulnar nerve distance does not change significantly with insufflation. Importantly, joint distention does not increase the distance between the joint capsule and the adjacent neurovascular structures (Fig. 39.2A, B). Therefore, it does not protect these structures from work performed against the joint capsule. An additional benefit is that joint distention makes capsule penetration easier and more reliable. However, distention of the joint with more than 25 mL of saline risks capsular rupture. This may result in poor visualization and fluid extravasation during the procedure. In addition, exercise caution when insufflating degenerative or posttraumatic elbows as they may not have the capacity to hold more than 10 mL.
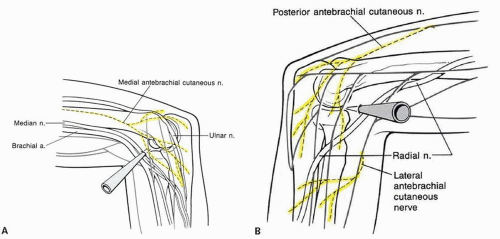 FIGURE 39.3. A: Diagram of the medial elbow cutaneous nerves. B: Diagram of the lateral elbow cutaneous nerves. |
Cutaneous nerves should be protected during portal placement (Fig. 39.3A, B). When establishing portals, we advise only incising the skin to protect the subcutaneous nerves. Blunt dissection through the subcutaneous tissues is then performed prior to cannula insertion. Stab incisions should always be avoided.
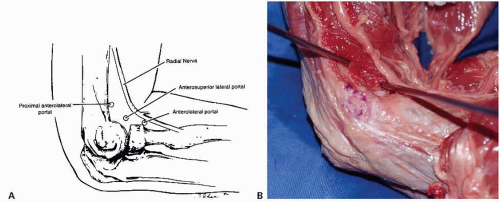
When performing arthroscopy in the anterior compartment, utilize proximal portals, as they are safer than distal portals. Field et al. showed that a proximal anterolateral portal is located farther away from the radial nerve than the standard anterolateral portal (Fig. 39.4A, B). In addition, they found that the more
proximal portal provided equivalent visualization. The proximal anteromedial portal popularized by Poehling et al. has also been shown to be safer than the anteromedial portal. As Figure 39.5 demonstrates, the median nerve is significantly further from a more proximally placed anteromedial portal than a standard anteromedial portal. In addition, the more proximal position allows the arthroscope to be directed distally, resulting in the arthroscope being almost parallel to the median nerve in the coronal plane.
proximal portal provided equivalent visualization. The proximal anteromedial portal popularized by Poehling et al. has also been shown to be safer than the anteromedial portal. As Figure 39.5 demonstrates, the median nerve is significantly further from a more proximally placed anteromedial portal than a standard anteromedial portal. In addition, the more proximal position allows the arthroscope to be directed distally, resulting in the arthroscope being almost parallel to the median nerve in the coronal plane.
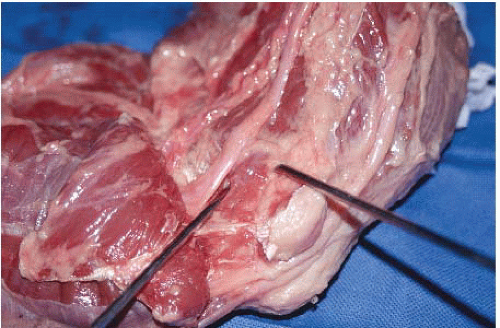 FIGURE 39.5. Anatomic dissection of the medial side of the elbow demonstrating the proximity of the median nerve to the proximal anteromedial (right) and standard anteromedial (left) portals.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|