Avoiding ACL Graft Impingement: Principles for Tunnel Placement Using the Transtibial Tunnel Technique
Keith W. Lawhorn
Stephen M. Howell
INDICATIONS/CONTRAINDICATIONS
The transtibial tunnel technique in which the femoral tunnel is drilled through the tibial tunnel is a common technique for tunnel placement. This technique can be used regardless of the type of graft material and fixation. The transtibial technique can be used in all patients requiring a primary anterior cruciate ligament (ACL) reconstruction both acute and chronic, revision ACL surgery, and ACL reconstruction in the setting of the multiligament knee injury. There are no absolute contraindications to use of the transtibial tunnel technique for ACL reconstruction. Correct tunnel placement for ACL reconstruction is imperative to the success of the procedure. Graft sources, fixation methods, and rehabilitation cannot overcome the adverse consequences of poor tunnel placement.
There are three criteria of correctly placed tibial and femoral tunnels for ACL reconstruction: (a) the avoidance of roof impingement, (b) avoidance of posterior cruciate ligament (PCL) impingement, and (c) the establishment of the tensile behavior in the ACL graft similar to the native ACL. All three criteria are required for a successful ACL reconstruction.
Roof impingement occurs when the ACL graft prematurely makes contact with the intercondylar roof of the notch before the knee reaches terminal extension, which causes loss of extension and anterior laxity. The cause of roof impingement is positioning the tibial tunnel too anterior in the sagittal plane.
PCL impingement occurs when the ACL graft makes contact with the leading edge of the PCL before the knee reaches terminal flexion, which causes loss of flexion and anterior laxity. The cause of PCL impingement in the transtibial technique is positioning the tibial tunnel too vertical and medial in the coronal plane.
Finally, correct femoral tunnel position in both the sagittal and coronal planes is required to establish the tensile behavior in the ACL graft similar to the native ACL. Because the femoral tunnel is drilled through the tibial tunnel using size-specific aimers, the position of the tibial tunnel determines the position of the femoral tunnel with the transtibial technique. Therefore, the tibial tunnel sets up the position of the femoral tunnel, which means that the key tunnel in the transtibial tunnel technique is the tibial tunnel.
PREOPERATIVE PLANNING
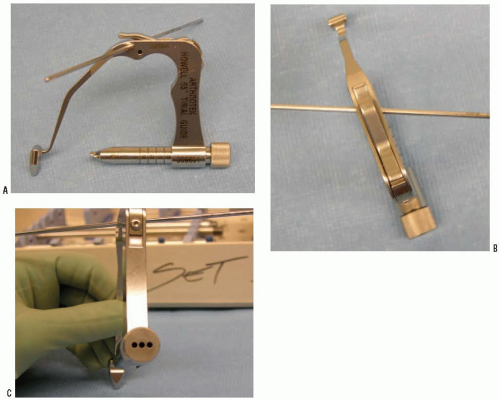
Once the decision has been made by the patient to undergo surgical treatment of the ACL deficient knee, the surgeon must decide on the technique for placing the tunnels, graft choice, and fixation. All tunnel placement techniques including the transtibial, transportal, and two-incision technique can be used with any type of graft and fixation. Scientific studies by a variety of authors support the use of the transtibial tunnel technique and the use of the 65-degree tibial guide (Arthrotek, Warsaw, IN) that references the intercondylar roof with the knee in full extension for placing the tibial tunnel (Fig. 14-1).
An advantage of the transtibial technique with the 65-degree tibial guide is that the tunnel placement is accurate and customized without the need for tedious preoperative planning or time-consuming intraoperative imaging. Customization begins with the use of the 9.5-mm wide tip of the 65-degree tibial guide to gauge the width of the space between the lateral edge of the PCL and the lateral femoral condyle. Generally, the space between the PCL and the lateral femoral condyle is substantially smaller than the width of the ACL graft. The portion of the notch allocated to the ACL graft varies among patients as evidenced by some notches being narrower than others, and by the cross-sectional area of some notches being dominated by the PCL, leaving little room for the ACL graft. We advocate widening the notch by removing bone from the medial edge of the lateral femoral condyle (i.e., wallplasty) until the space between the PCL and lateral femoral condyle exceeds the width of the ACL graft by 1 mm. Since most grafts range from 8 to 10 mm, the free insertion of the 9.5-mm wide tip of the guide between the PCL and lateral femoral condyle indicates that the notch is sufficiently wide. Customizing the width of the notch to accommodate the width of the ACL minimizes PCL impingement by moving the tibial tunnel, femoral tunnel, and ACL graft lateral away from the PCL, which minimizes PCL impingement improving flexion and anterior stability.
A second step of customization is that the 65-degree tibial guide accounts for the anatomic variability in the angle of the intercondylar roof and knee extension that exists between patients and consistently positions the tibial tunnel in the posterior half of the native ACL tibial footprint and avoids roof impingement without a roofplasty. The roof angle (23 to 60 degrees) and knee extension (- to 30 degrees) both vary widely among patients. The correlation between the two is weak, so that patients with the same roof angle often have a different knee extension and patients with the same knee extension often have a different roof angle. Surgeons need to account for these two independent variables simultaneously. By drilling the tibial tunnel with the knee in full extension while referencing the intercondylar roof with the 65-degree tibial guide, the sagittal placement of the tibial tunnel has simultaneously accounted for the patient’s unique combination of roof angle and knee extension. Magnetic resonance imaging studies have demonstrated the native ACL is located posterior and parallel to the intercondylar roof with the knee in terminal extension. The tibial tunnel is positioned posterior and parallel to the intercondylar roof and prevents roof impingement of the ACL graft without performing a roofplasty, which improves knee extension and anterior stability.
A third step of customization is that the 65-degree tibial guide incorporates the use of a coronal alignment rod, which improves the accuracy of setting the angle of the tibial tunnel in the coronal plane, further minimizing the risk of PCL impingement. Setting the angle of the tibial tunnel at 65 ± 5 degrees in the coronal plane avoids PCL impingement. The use of the transtibial technique and a tibial tunnel at 65 ± 5 degrees in the coronal plane positions the femoral tunnel so that the tensile behavior of the ACL graft is similar to the native ACL while improving knee flexion and anterior stability.
The last step in customization is the use of size-specific femoral aimers through a tibial tunnel placed to create a femoral tunnel with a 1-mm back-wall for any diameter ACL graft. The use of the size-specific femoral aimers in a knee in which the notch has been sufficiently widened, without roof impingement and without PCL impingement, ensures correct placement of the femoral tunnel. The remnants of the ACL origin in the over-the-top position must be removed so that the femoral aimer rests on bone. Resting the femoral aimer directly on bone creates a femoral tunnel with a thin 1-mm back-wall and eliminates “blowingout” the posterior wall of the femoral tunnel. Therefore, the advantage of the transtibial technique is that the surgeon needs to focus on the meticulous placement of only one tunnel, the tibial tunnel, reducing the error associated by placing the femoral and tibial tunnels independently.
For surgeons, choosing to use a point-and-shoot guide, preoperative lateral radiographs taken with the knee in full extension, helps determine the intercondylar roof angles and knee extension and aids them intraoperatively when positioning the tibial tunnel in the sagittal plane. Surgeons must estimate coronal plane positioning with these guides since there are no coronal alignment devices on these guides. The standard is to use intraoperative fluoroscopy to check the position of the tibial guidewire in both the sagittal and coronal planes before drilling the tibial tunnel.
SURGERY
Patient Positioning
Position the patient supine on the operating table. After induction of anesthesia, perform an examination under anesthesia. Place a tourniquet around the proximal thigh of the operative leg. Position the operative leg in a standard knee arthroscopy leg holder with the foot of the operating table flexed completely. Alternatively, surgeons may decide to use a lateral post instead of a leg holder. Position the contralateral leg in a gynecologic leg holder with the hip flexed and abducted with mild external rotation. Ensure there is no pressure on the peroneal nerve and calf (Fig. 14-2). Alternatively, surgeons can position the operative leg flexed over the side of the table using a lateral post and maintaining the contralateral leg extended on the operating table.
Technique
After sterile prep and drape, exsanguinate the leg and inflate the tourniquet. Establish inferolateral and inferomedial portals touching the edges of the patella tendon starting 1 cm distal to the inferior pole of the patella. Alternatively, a transpatellar inferolateral portal can be used with a medical portal placed along the medial border of the patella tendon (Fig. 14-3). The medial portal must touch the edge of the patella tendon because if it is placed more medial, the tibial guide may not stay seated in the intercondylar notch with the knee in full extension. An optional outflow portal can be established superiorly.
Perform a diagnostic arthroscopy. Treat meniscal or articular cartilage injuries. Identify and remove the torn remnant ACL stump (Fig. 14-4). It is not necessary to denude the tibial insertion of the native ACL tissue. In fact, retaining the insertion of the native ACL helps seal the edges of the ACL graft at the joint line and does not result in roof impingement if the tibial tunnel has been appropriately positioned. Remove the synovium and soft tissue in the notch to expose the lateral edge of the PCL (Fig. 14-5). Remove any of the ACL origin from the over-the-top position using an angled curette and shaver (Fig. 14-6).
Insert the tibial guide through the medial portal. Advance the guide into the intercondylar notch (Fig. 14-7




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree