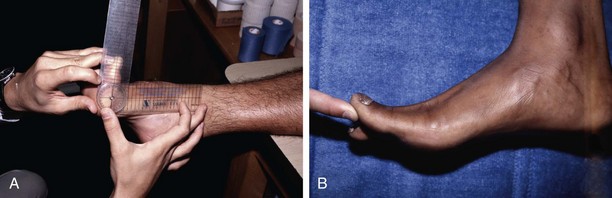
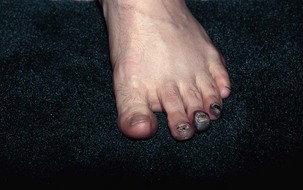
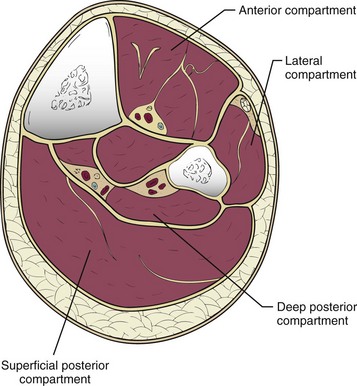
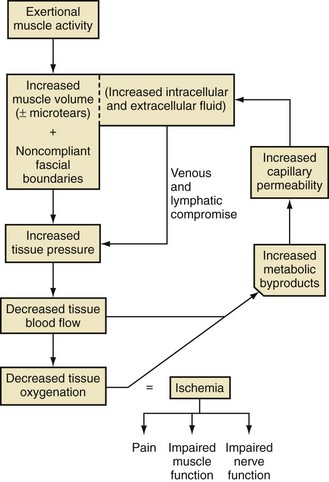
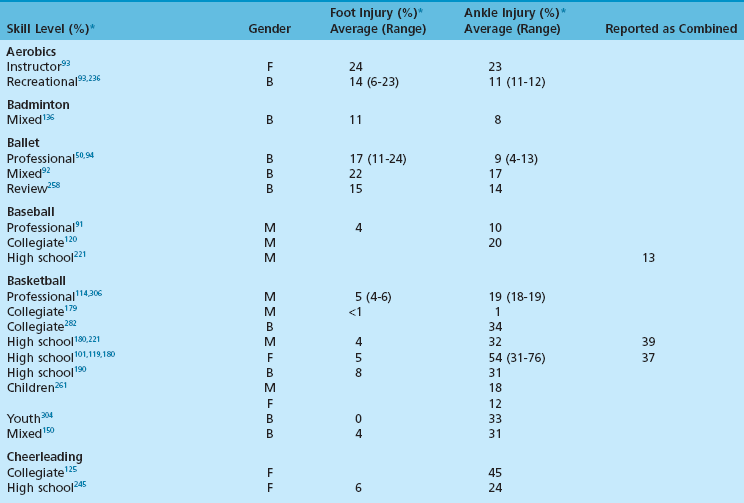
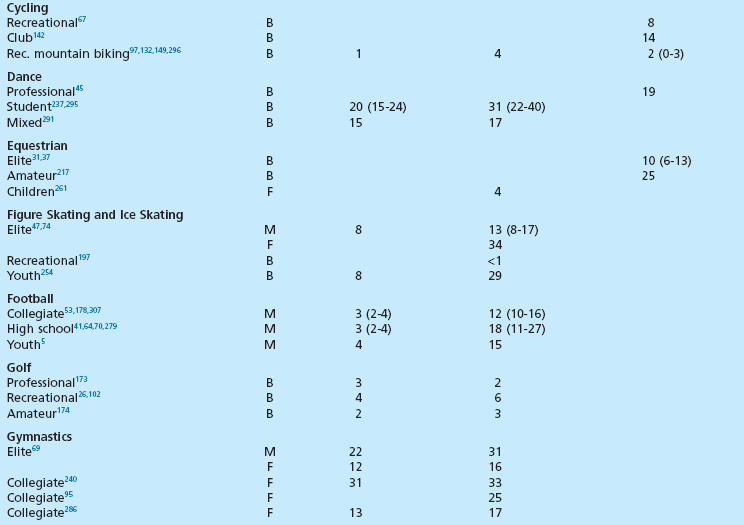
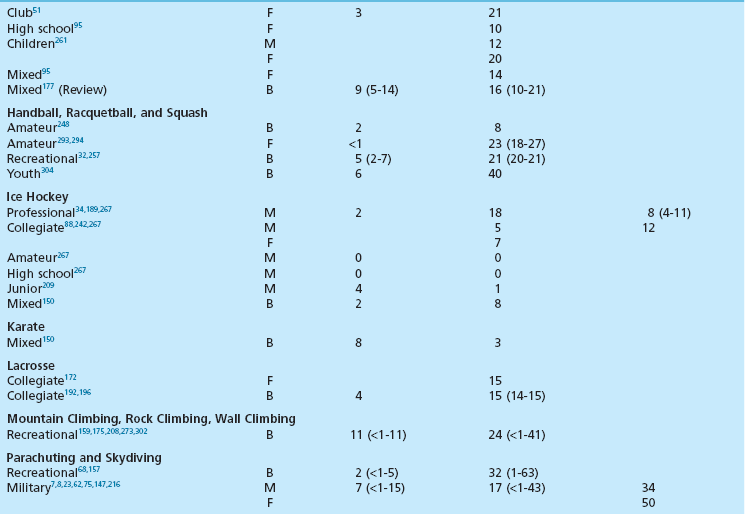
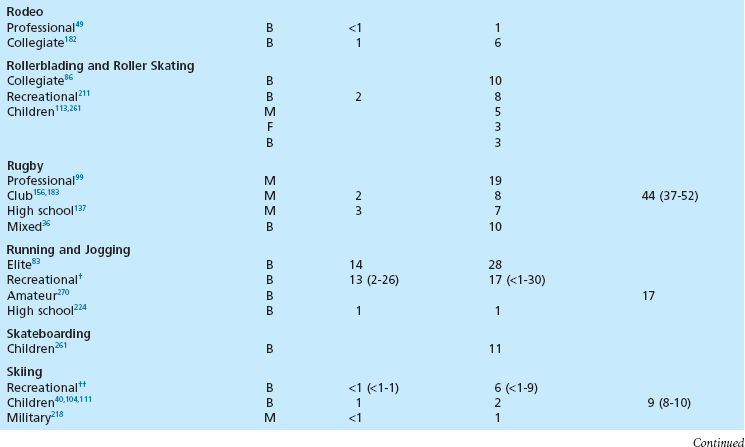
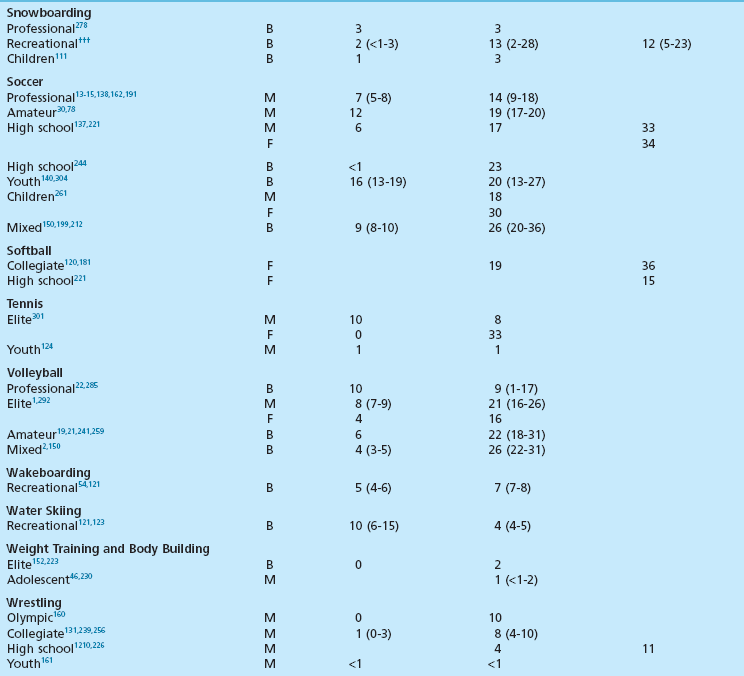
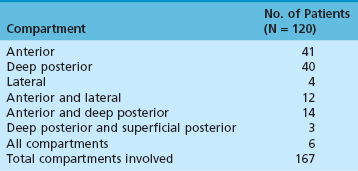
Chapter 30 Chronic Exertional Compartment Syndrome Stress Fractures of the Tibia and Fibula Popliteal Artery Entrapment Syndrome SYNDESMOSIS SPRAINS OF THE ANKLE (HIGH ANKLE SPRAIN) History and Physical Examination Surgical Treatment of Tendinitis, Tendinosis, and Haglund Deformity ( Injuries to the ligaments, tendons, fascia, and other soft tissues of the leg, foot, and ankle are discussed in this chapter, along with a brief review of etiologic factors for such injuries. Acute fractures and stress fractures are common in sports but are not a part of this chapter (see Part VIII, Chapter 31). Specific problems related to the foot in running are addressed in Part VIII, Chapter 31. The chapter on injuries in dancers has been eliminated, but the wisdom of Bill Hamilton has been incorporated into other chapters dealing with the specific injuries common to dance, many of which are included in this chapter. Arthroscopic evaluation and treatment are mentioned where they are important, but Part VIII, Chapter 32 deals with the specific role of arthroscopy. Some conditions reviewed here are found in other sections of the textbook as well (e.g., bunion and hallux rigidus), but they are considered with a sports medicine perspective in this chapter. Despite efforts to the contrary, sports participation begets injury (Fig. 30-1). The following discussions review both traditional and new techniques in the diagnosis and treatment of athletic injuries to the soft tissues of the foot and ankle. Prevailing trends are the expansion of diagnostic imaging, including use of diagnostic ultrasound and a lower threshold for use of magnetic resonance imaging (MRI), and cautiously aggressive rehabilitation. Herodotus of Halicarnassus records the first ankle sprain in sports in his historical writings from the time of the Greek and Persian empires when King Darius I of Persia twisted his ankle while hunting.42 Herodotus also documents the first use of exercise as a treatment in Western medicine. This is not surprising, since track and field events were an integral part of the early religious festivals held at Olympia, Delphi, Nemea, and Corinth, and the first date recorded on a Western calendar was a sports event, the Olympiad of 776 BC.17,108,206 Paré was the first to point out that exercise of the limbs was essential to recovery after treatment of a fracture. For the physician treating an athlete, this approach reflects the essence of sports medicine. Sports participation has become a fundamental characteristic of American society. A survey of a few of the more popular sports reveals that about 17.7 million people play football, 14.5 million play soccer, 15.6 million play baseball, 28.9 million play basketball, and 13.6 million play softball.194 Injuries to the lower extremities constitute the majority of injuries for most sports (Fig. 30-2). This is particularly true for the running, jumping, and kicking sports. Table 30-1 provides a look at injury rates calculated for the foot and ankle from studies done for various sports. As of 2006, yearly sports participation at the high school level had increased each year for the previous 17 years, reaching 53.5% in 2006.195 Table 30-1 Calculated Foot and Ankle Injury Rates in Various Sports: Literature Review B, both sexes; F, female; M, male; Rec, recreational. †References 103, 171, 269, 271, 284, and 288. ††References 38, 55, 56, 65, 66, 72, 76, 77, 84, 134, 154, 155, 165, 249, 266, 281, and 290. †††References 4, 52, 55, 56, 66, 87, 111, 130, 143, 154, 155, 164, 166, 219, 220, 281, and 290. All sports and recreational activities carry an inherent risk of injury. It is a natural consequence of pushing against the body’s physical limitations and being involved in challenging competition. Nevertheless, one of the goals of sports medicine is to reduce the health risks of athletic participation by recognizing and controlling the risk factors. From the vantage point of careful epidemiologic study, it is possible to identify and quantify risk along with the incidence and prevalence of injury for a given set of conditions.228 To analyze epidemiologic data properly, it is critical that the population being analyzed is assiduously defined. Many studies of athletic injuries that have engendered prejudicial thinking about the causes for injuries are flawed because of their methodology. Contemporary medicine favors evidence-based health care and outcomes-based research. Unfortunately, the literature in sports medicine, orthopaedics, and even medicine in general is overwhelmingly derived from reports and retrospective case series where the level of evidence is less than ideal. Many of these case series report an injury rate, but they often fail to accurately define the population at risk for injury. A good example is the prevalent idea that runners who pronate (or more precisely, overpronate) are at a greater risk for a running injury. The 1978 article by James et al126 fostered this idea by noting that 58% of their 180 patients had a pronated foot configuration. This study does not take into consideration the total number of people in the running population from whom this select group was derived who also pronate but do not have an injury problem. Another problem with many studies is failure to provide an accurate definition of the factor being analyzed. In sports injury studies this is often related to variations in the definition of what constitutes an injury from one study to the next. For example, it is difficult to compare ankle injury studies such as Rowe’s,238 where an injury is defined as anything that causes an athlete to require medical attention and lose time from participation, with studies with much stricter definitions and classifications, such as Torg and Quedenfeld’s.274 The comparison difficulties are magnified when the comparison extends across sports and across levels of participation, because an injury to a peewee football participant might have no relationship to what a professional rugby player considers an injury. With these factors in mind, one can appreciate the differences between studies and the number of variables involved.59 The risk factors for injury can be divided into intrinsic and extrinsic varieties. The athlete’s physical and personality traits constitute the intrinsic factors, and the training techniques, playing environment, and equipment are among the extrinsic risk factors. In this regard, several studies have demonstrated that weekly running mileage is the most critical factor in the risk of injury in the running population.39,163,171,222,288 When weekly mileage surpasses 64 km (40 miles), the risk of injury increases logarithmically. Other significant risk factors in runners include a history of injury in the recent past, having run for 3 years or less, and a recent major change in the training regimen or environment. Intrinsic and extrinsic factors have a potential role in the cause of injury to the athlete.59 Analysis of these factors sometimes allows intervention that can reduce or eliminate the risk factor and thereby lower the risk of injury. This is the heart of preventive sports medicine. Examples of such intervention include rule changes in football to eliminate the “crack-back block,” “spearing,” and “head-to-head” contact, as well as improved generations of synthetic grass and underpadding brought about by research into the relationship between artificial turf and injury.158,213–215,253 Janda et al127,129 found that 70% of softball injuries were related to stationary bases, and 56% of these injuries were to the foot and ankle. By substituting breakaway bases, they demonstrated a reduction in injuries from 1 in 14 games to 1 in 317 games (Fig. 30-3). Bahr and Bahr have similarly demonstrated the possibility of reducing ankle injuries in volleyball through an injury awareness program and training with a balance board.20 These types of studies can clearly affect the health of athletes, and particularly their feet and ankles. Certain underlying anatomic conditions are often related to athletic injuries. Many runners and coaches place abnormal foot biomechanics in this category in the belief that the runner with excessive pronation has an innately higher risk for sustaining a running-related injury.58 A prospective cohort study of collegiate cross-country runners found almost seven times increased risk for medial exercise-related leg pain in those with significant pronation.28 Two other studies of runners found little correlation between anthropometric measurements (femoral neck anteversion, pelvic obliquity, knee and patella alignment, rearfoot valgus, pes cavus/planus) and risk for injury.280,288 Only pelvic obliquity was a positive predictor of injury, and only in one study. Dancers, like runners, are another population often studied for an association between biomechanical abnormalities and injury risk. Although dance medicine specialists often relate lower extremity injury to poor technique and misalignment,112,122,170 two independent studies failed to confirm such an association.176,263 Studies of military recruits have provided much useful epidemiologic information because of the controlled nature of the population and their training regimen. A common injury among military trainees is the stress fracture. Although flat feet have been a disqualifying factor for military service in the past, some studies have shown that recruits with flat or pronated feet had no greater incidence of stress fracture than the remaining population.29,71,98 A study of the relationship between arch height and stress fractures in Israeli military recruits showed an increased incidence of metatarsal stress fractures in recruits with a low arch but fewer tibial and femoral stress fractures.252 A study done on Navy SEAL trainees showed an increased risk of stress fractures of the lower extremity in recruits with either pes planus or pes cavus. It also showed that there was an increased risk of femoral stress fractures in trainees who had restricted hindfoot inversion and an increased risk of tarsal or metatarsal stress fractures in trainees with increased hindfoot inversion.139 A study that attempted to correlate arch height with injury in runners found that transfer of foot eversion movement to internal leg rotation—a factor often related to knee pain—increased significantly with increasing arch height.203 However, arch height only contributed 27% to 34% of the variation in the transfer of movement between subjects. This indicates that other undelineated factors also influence kinematic coupling at the ankle–hindfoot joint complex, including the variation in plantar pressure pattern noted in runners with differing foot types.255 Theoretically, both the high-arched and the low-arched foot can cause impairment of subtalar and transverse tarsal joint function and thereby cause overuse injury.139 Pre-exercise or pre-participation stretching has long been thought to help prevent injury. A systematic review of the literature looking at neuromuscular warm-up strategies and injury prevention found a trend toward reduction in ankle sprains with practical neuromuscular warm up strategies which included stretching and proprioception training, including the use of a balance board. Results improved when exercise was maintained for more than 3 months and performed on a regular basis in each training section.115 Lack of flexibility has often been cited as the factor responsible for various sports-related complaints, although prior in-depth reviews of the literature have failed to show a correlation between stretching and the rate of injury. Thacker et al272 and Krivickas and Feinberg148 prospectively studied two components of flexibility—muscle tightness and ligamentous laxity—in college athletes. They found a significant association between lower extremity injury and both tight ligaments and overall muscle tightness scores in men but not women. Owing to their small numbers for individual sports, the data could not be analyzed for specific sports. Because a discussion of flexibility and stretching can evolve into an expansive section of its own, the present discussion is confined to relevant comments specific to the foot and ankle. Lack of flexibility about the ankle and foot or limitation in motion of certain joints can be seen in association with certain disease processes or conditions, but the more common situation in the sports setting is single joint involvement, as seen in tarsal coalition. Athletes may have reached highly competitive levels of participation before the coalition limits them to the extent that they seek medical attention. They typically have a history of frequent ankle sprains, and the limitation in subtalar motion in these patients with talocalcaneal coalition may have been overlooked in the past.151 Restricted ankle motion in dorsiflexion is a factor in the anterior ankle pain seen in skiers and in runners who do hill work. This is often associated with anterior tibial and dorsal talar neck osteophytes at the ankle joint. Limited dorsiflexion of the ankle has been blamed for a multitude of other problems around the foot and ankle, including bunions,169 turf toe,235 midfoot strain and plantar fasciitis,141,153,262 ankle sprains,287,268 Achilles tendinitis,59 calf strains,80,188 and excessive pronation (including all the problems that it can allegedly produce).42–44,60,139,167 All these conditions have been related to a tight Achilles tendon and its effect in limiting ankle dorsiflexion, but no studies have unequivocally documented this relationship. Limited motion in the toes rarely receives much attention as an etiologic factor in injury or symptoms. However, a lack of flexibility is one of the critical components in the diagnosis of certain conditions such as hallux rigidus, which involves a characteristic loss of dorsiflexion in the first metatarsophalangeal (MTP) joint (Fig. 30-4).168 In dancers with acquired hallux rigidus, restriction in great toe dorsiflexion to less than 90 to 100 degrees can produce compensatory positions that predispose the dancer to ankle inversion sprains and misalignment syndromes.122,225 Limitation of motion in the other MTP joints is seen in patients with Freiberg’s infraction. When the interphalangeal (IP) joints of the toes are involved in loss of motion, a problem seldom exists unless an associated deformity is present, such as a hammer toe or mallet toe. These conditions in athletes can produce sufficient symptoms to require surgical treatment. At the opposite end of the mobility spectrum, hypermobility is infrequently mentioned as the source of problems in the foot and ankle in athletes.9 Pathologic laxity is common to certain connective tissue disorders, including Ehlers-Danlos syndrome, Marfan syndrome, Larsen syndrome, Down syndrome, hyperlysinemia, homocystinuria, and osteogenesis imperfecta.106,118,264 A hypermobility syndrome unassociated with known connective tissue disease has also been described as a potential source of musculoskeletal symptoms and signs, including ankle joint effusions.59 In certain sports such as ballet and gymnastics, there is selectivity bias for the more flexible performer. Ballet dancers are particularly noted for the tremendous mobility in their feet and ankles. The same could be said for divers and gymnasts, who are awarded for having greater ability in achieving maximum plantar flexion so the foot assumes a pleasing line with the leg. Although this increased flexibility has obvious advantages, it may also have a negative side. Klemp et al144,145 have found an increased incidence of injury in ballet dancers who have greater mobility; others295 have failed to find such a relationship, however. While attempting to achieve the desired flexibility in ankle plantar flexion, the ballet student may develop posterior ankle pain from impingement with a large posterior talar process, calcaneal osteophyte, or os trigonum.260 A pathologic increase in joint laxity is termed instability.60 Many studies have shown that a history of previous ankle injuries predisposes athletes to future ankle sprains.79,295,305 Chronic instability of the ankle joint, a dynamic interrelationship between mechanical and functional factors, is a major factor in recurrent injuries to the ankle, whether it is due to a proprioceptive deficit, loss of ligamentous integrity, or some other condition.116 A study by Willems et al300 has shown that patients with chronic ankle instability have decreased proprioception at the extremes of inversion as well as decreased evertor strength when compared to normal counterparts. On the other hand, physiologic laxity has shown no similar trend.33 Clinically the difficulty is in differentiating between these two conditions. This is clarified further in the ankle ligament section. It is a commonly held belief that weak musculature predisposes a person to injury in sports. It is often stated that weak peroneal muscles are a factor in inversion sprains of the ankle, and one of the goals of rehabilitation after an ankle sprain is to strengthen these muscles. Fully activated strong ankle evertors exceed three-quarter-top shoes, taping, and orthoses in the protection they offer to the inverted ankle at foot strike.16 Several studies have shown that improving strength can reduce the risk for reinjury.* Most work in this area is related to strength in the thigh musculature about the knee. Similarly, muscle strength imbalances, which are viewed as creating a propensity for injury, have primarily been studied with reference to the quadriceps-to-hamstring ratio (ideally around 5 : 4 depending on the test method and test speed).12,146,198,263,303 Other studies have concluded that strength differences of more than 10% between the right and left legs increase the injury risk.27,48 Ekstrand et al81 used this figure in their prospective study on the prevention of soccer injuries. They discovered a 75% reduction in injuries with a prophylactic program that included rehabilitation, to the point that 90% of muscle strength had been regained. No similar ratios are found for the ankle and its proximal musculature to guide rehabilitation or expose a greater potential for injury to the leg, ankle, or foot. Silver et al250 performed the baseline work on strength of the leg muscles. They reported the ratio of plantar flexors to dorsiflexors as 6 : 1, or stated conversely, the dorsiflexors are normally only 17% of the plantar flexors in terms of strength. The peroneals have only 8.1% mean strength in comparison to the dorsiflexors at 9.4% and the plantar flexors at 54.5%. The peroneus brevis muscle has a mean strength of 2.6% and the peroneus longus a mean strength 5.5% in comparison to the strongest muscle, the soleus, at 29.9%. Strength imbalance in the leg is a clear risk factor for injury to the ankle. Baumhauer et al25 showed that athletes with a lower dorsiflexion-to-plantar flexion ratio had greater risk of injury. With a higher eversion-to-inversion ratio, the athletes had a higher incidence of inversion ankle sprains. This work was corroborated in a second isokinetic strength test study that showed invertor muscle strength deficiency was more important than evertor deficits in lateral ankle ligamentous injuries. A cohort study of professional soccer players in Greece showed an increased propensity for ankle sprains when athletes had preexisting functional strength asymmetries about the ankle.89 Another prospective study failed to find a relationship between ankle strength and muscle reaction time with the risk of ankle injury.33 Nevertheless, rehabilitation designed to restore the normal strength ratio through an isotonic and isokinetic strengthening program should reduce the risk of ankle injury. The relationship between weakness and potential for injury in sports has been further corroborated by studies of soccer players. Backous et al18 performed a prospective study of boys attending a summer soccer camp, with the ankle being the most frequent site of injury. The highest incidence occurred in boys who were tall and had weak grip strength, which led the authors to conclude that skeletally mature but muscularly weak boys were at increased risk for injury compared with their peers. Ekstrand and Gillquist found that soccer players who sustained a minor injury during the preceding 2-month period had a 20% increase in their risk of developing a more serious subsequent injury.78,79 Similarly, Bahr and Bahr19 noted a 42% increase in risk of reinjury in volleyball players who had suffered an ankle sprain within the preceding 6 months. This reinjury risk is attributed to inadequate rehabilitation and poor muscle strength and is supported by several studies.19,20,25,299,305 Rotational forces generated by the body at the shoe/surface interface are an important factor in sports injuries, but other factors are just as important. One of the most neglected but commonplace causes is improper fit of the athletic shoe. Just as this has been shown to be a prime cause of foot complaints in the general population, it is likewise a common source of relatively minor, although annoying, problems for athletes.59,60 When the athletic shoe is improperly fitted, the overly tight shoe causes pressure-related pain at the site of bunions and bunionettes, or it can cause metatarsalgia. When the athletic shoe is too loose, it allows the foot to slide, and blisters result. When the shoe is too short, the toes jam into the end. This can result in nail problems or the black toes of long-distance runners (Fig. 30-5). A more novel fitting-related problem occurs with tightly fitting ski boots, where excessive pressure at the ankle causes a neurapraxia of the posterior tibial nerve or the superficial peroneal nerve. Similarly, posterior tibial tendinitis or aggravation of an accessory navicular can occur from an ice-skating boot. Irritation of the Achilles tendon and production of a retrocalcaneal bursitis can occur from a variety of footwear, especially when there is a rigid heel counter. Careful fitting of the athlete can generally avoid or alleviate these types of problems rather than having to resort to surgical intervention (Fig. 30-6). The shoe can be a source of problems in other ways as well, such as a lack of cushioning or lack of support. Load on the human body has been implicated as a specific etiologic factor in sports injuries.200–202,204 Because a significant component of this load is the vertical impact force or ground reaction force, cushioning, or shock absorption, by the shoe is an important property. The ability of shoes to prevent injury through improved cushioning properties has had mixed reviews in the studies of this subject. Greaney et al107 showed a reduction in calcaneal stress fractures in military recruits by switching to tennis shoes. A study of South African military recruits reported a reduction in overuse injuries by incorporating a neoprene insole into the shoes used in training.246 A report on aerobic dance injuries included a mention of the beneficial effects of cushioned shoes in reducing injuries.229 However, a study of the U.S. Army Marching Band, whose members were switched to more cushioned shoes, showed no significant decrease in injuries.109 Other studies have also shown no benefit from increased shock absorption in either shoes or insoles.90,135,185,186 An interesting counterproposal to the idea that improved cushioning in the shoe is protective to the body is the Robbins and Hanna hypothesis.234 They have proposed that increased cushioning can actually be an etiologic factor in injury by dampening the body’s own sensory feedback mechanism coming from the plantar surface of the foot, thereby producing a “pseudo-neuropathic” condition.232,233 This is a thought-provoking concept, and barefoot exercise or performance does appear to have some benefits. It has even spawned a new trend in running shoes—the “minimalist” running shoe (Fig. 30-7). Such shoes with little padding and arch support (with or without individual toe compartments) have become part of mainstream running. The traditional modern running shoe with increased cushioning and support allows more forceful heel strike and longer stride length while the minimalist shoe forces a shorter stride and better dispersion of forces across the entire foot. Improved dispersion of impact forces has been verified by biomechanical studies.231 Future research will be needed to compare injury rates between cushioned and minimalist shoes. Traction between the shoe and the surface can be separated into two categories: rotational (or torque) and linear (or shear). As traction increases, the forces on the knee and ankle increase as well, resulting in greater propensity for injury in these areas.289 One study proposed that two thirds of all non-contact soccer injuries were related to excessive shoe surface traction.82 Load on the body related to traction has been studied with reference to both rotational and linear forces.10,63,205,243,283 Several components contribute to traction in footwear design analysis. These include the outsole material, sole pattern, and the presence of cleats as well as their number, length, and pattern. Torg et al274,275 studied football shoes and demonstrated precariously high torque when the shoes had ¾-inch-long cleats. Other shoe surface combinations were also considered potentially unsafe.274–277 Softer outsole materials are also associated with increasing torque when used on artificial or clean hardwood court surfaces, but the presence of dust on the floor can alter this effect.227 Research has clearly documented the relationship between cleating of the athletic shoe and sports injuries.59 In one study of high school football injuries, the number of ankle injuries was halved by changing from the traditional seven-cleated grass shoe to a soccer-style shoe.238 Further support for this came from Torg and Quedenfeld,274 who found a reduction in ankle injuries from 0.45 per team per game while using conventional cleats to 0.23 injuries in soccer-style shoes. Similar reductions have been reported in other studies evaluating other cleating patterns and surfaces.41 From the opposite standpoint, a lack of traction can potentially cause injury by increasing the frequency of slips and falls. Biener and Caluori35 reported that slipping on wet tennis surfaces was a factor in 21% of injuries. Clearly, problems can occur from either too much or too little traction. Athletes and coaches demand maximum traction for superior performance, but there comes a point where this can exceed the body’s ability to handle the load. A study of two shoes with treaded versus smooth sole design found increased traction with the treaded design, resulting in increased forces on the knee and ankle. Despite this, there was no difference in performance noted between the two shoes.289 An ongoing debate in the shoe equation as it relates to injury is high-top versus low-top shoes. Relatively few studies have scientifically investigated the value of different shoe heights in reducing ankle sprains. High-top shoes can be at least 50% stiffer than low-cut models and are affected by both the material and the geometry of the shoe.133 This stiffness reduces the load carried by the collateral ligaments of the ankle. Conversely, when mobility necessitates use of a low-cut athletic shoe, the same mathematical model predicts the need for a low-stiffness shoe to allow maximum subtalar motion.133 Theoretically the high-top shoe should stimulate the proprioceptive feedback mechanism, resulting in greater sensitivity of the peroneal muscles and improved stability for the ankle.100 Garrick and Requa96 found a reduced frequency of recurrent ankle sprains in college intramural basketball players who used prophylactic taping and high-top shoes. In another clinical study, Milgrom et al187 found no evidence that high-top boots lowered the incidence of ankle injuries among Israeli military recruits when compared with three-quarter-top basketball shoes. A prospective randomized study of high-top versus low-top shoes reached a similar conclusion related to the prevention of ankle sprains.24 Ottaviani et al207 have shown that basketball shoe height increases the maximum resistance to an inversion moment but does not affect the athlete’s ability to resist an eversion moment. According to one study, active ankle evertor muscles provide greater protection to inversion stress than three-quarter-top shoes, athletic taping, or orthoses.16 In recent years there has been extensive research into the biomechanics of ankle taping and bracing, which have shown differences in a variety of different biomechanical and neuromuscular measurements, including restriction of maximum ankle motion and improvements in peroneal muscle response during inversion movements.298 Ankle taping does improve proprioception, which is generally accepted to reduce the risk of injury to the ankle.616 Nevertheless, there continues to be debate over the best method for preventing ankle sprains related to taping, bracing, and high-top shoewear. Load on the athlete as a factor in injury has led to a critical analysis of playing surfaces since 1980. This has primarily been stimulated by the introduction of artificial playing surfaces and particularly by the allegations that artificial grass causes increasing injury rates. Although substantial attention has been given to this subject in both the lay and the medical communities, there is still substantial debate over the degree and manner by which playing surface differences (particularly artificial turf vs. natural turf) increase risk of injury in sports.59,73,184,247,297 It does appear that third- and fourth-generation artificial turf have only minimal differences in injury rates compared to natural turf except perhaps for ankle injuries occurring more frequently on artificial turf.297 Although artificial surfaces have received the most attention, evidence also indicates that natural grass is a factor in injuries as well. This is particularly true when the field is not maintained properly. The classic 1974 study of high school injuries by Mueller and Blyth193 reported a 30% reduction in the injury rate by resurfacing and maintaining the grass practice and game fields. Several studies of soccer, dance, and even ice hockey injuries have also indicated the playing surface as a factor.* One of the most important studies on the relationship between injuries and playing surfaces is that of Janda et al,128 who found 70% of recreational softball injuries to be related to sliding into fixed bases. The follow-up to this study showed a 98% reduction in serious injuries with the use of breakaway bases (see Fig. 30-3).127,129In running, hard surfaces and hills are seen as important factors in injuries, but few confirmatory studies have been done. The Ontario Cohort Study, one of the better epidemiologic studies of running injuries, found no relationship between surface and injury.288 A simultaneously reported 1989 study from South Carolina noted the only significant relationship between injuries and training surface to be in female runners running on concrete (Fig. 30-8).163 Powell et al222 examined the multiple etiologic factors involved in running injuries, including the running surface, and found little correlation. These studies have primarily examined injury from the standpoint of surface hardness. An alternate viewpoint is found in the European literature, where “eigen-frequencies,” or vibrational forces, from synthetic tracks are seen as a major factor in overuse problems in track athletes.11 Haberl and Prokop110 have described this as “tartan syndrome,” a surface-related problem from “long-term non-physiologic stress, resulting in acute, chronic or periodical irritant states.” There is no conclusive evidence to confirm the exact importance of vibrational forces in running injuries. Many conditions must be considered when evaluating chronic leg pain in athletes, including but not limited to exertional compartment syndrome, medial tibial stress syndrome, stress fractures, gastrocnemius and other muscle strains, nerve entrapment syndromes, venous disease, arterial occlusion, fascial herniations, tendinitis, and radiculopathies (Table 30-2). From these many potential etiologies, the clinician must narrow the diagnosis through focused history taking and physical examination coupled with appropriate diagnostic tests. As in most circumstances in orthopaedics, knowledge of anatomy and physiology forms the background for understanding these diverse causes for leg pain in the athlete. Table 30-2 Differential Diagnosis of Chronic Leg Pain in Athletes From Yates B, Allen MJ, Barnes MR: Outcome of surgical treatment of medial tibial stress syndrome. J Bone Joint Surg Am 85:1974–1980, 2003. Although it is difficult to assess the relative incidence of the various conditions that produce leg pain in the athletic population, it seems that about 25% relate to exertional compartment syndromes, 25% to stress fractures, and 25% to medial tibial stress syndrome or periostitis. This leaves a final 25% composed of an assortment of the less common causes, from radiculopathies to venous problems.329,420 Reviewing the literature on this subject leads to the conclusion that an accurate diagnosis is not always a certainty and coexisting pathologic entities may be more the rule than the exception. Up to 60% of patients with exertional leg pain have associated periostitis.403,426 This periostitis corresponds most closely to the commonly used lay description for nonspecific exertional leg pain: shin splints. This has been used for the diagnosis in up to 15% of all running injuries in some studies.373,387 Clearly, exertional leg pain is the source of many symptoms in the athletic population, and there is still ample opportunity for improving the accuracy of the diagnosis. Chronic exertional compartment syndrome (CECS) is defined as elevated compartment pressure in one or more of the fascial compartments of the lower leg caused by exercise that produces leg pain. In theory this pain has been attributed to local ischemia in the muscles and nerves due to impaired tissue perfusion.323,329,423,432 The firm boundaries of the fascial compartments in the leg (Fig. 30-9), when coupled with increased muscle bulk secondary to muscle contraction, intracellular and extracellular fluid accumulation, and muscle microtears, are responsible for the increasing pressures (Fig. 30-10). Arterial inflow remains normal, and venous and lymphatic compromise contribute to the vicious cycle of increasing tissue pressure, resulting in vascular compromise at the capillary level.399,434 This theory has been challenged by others who have not found signs of ischemia and propose that the pain is due to increased oxygen demand versus supply, fascial stretch, and/or stimulation of sensory nerves that respond to pressure or stretch.309,323,430,431 The absence of ischemia was confirmed in a well-designed MRI study by Andreisek et al, who found no difference in T2* relaxation times or arterial spin labeling signal between patients diagnosed with CECS and control subjects.310 Although the actual incidence of CECS is unclear, an approximation may be derived from one center that diagnosed three cases per year out of a university population of 40,000 students.339 In this study of 100 patients treated surgically, about 70% were runners. Ball and puck sports accounted for 20%, followed by racquet sports, skiing, golf, crew, gymnastics, boxing, fencing, and figure skating. There has been no documented difference in the incidence between men and women, and the median age of occurrence is 20 years of age.423 Athletes with CECS complain of pain during exercise that begins after a certain distance, duration, or speed. The condition may be either acute or chronic. The acute condition occurs after an unusual amount of exercise; the chronic form is more common and has an insidious onset. Eventually CECS progresses to a point where it restricts performance. In the early stages of involvement, pain completely or partially resolves with rest after a few minutes to several hours. Aching, cramping, or stabbing pain and a sensation of tightness in the involved compartment are characteristic. At times, associated neurologic symptoms occur, such as radiating pain, numbness, tingling, or burning along the course of the nerves that traverse the involved compartment. Simultaneous bilateral involvement is common, although usually not to the same degree. Several compartments may be affected simultaneously, most often the anterior and lateral compartments (Table 30-3). Deep and superficial posterior compartments are much less commonly involved.339,387,415 A history of previous or concurrent stress fracture has been noted in up to 17% of patients.339 Table 30-3 Number of Patients with Compartment Involvement From Martens MA, Moeyersoons JP: Acute and recurrent effort-related compartment syndrome in sports. Sports Med 9:62–68, 1990. Physical examination performed with the patient at rest is typically unremarkable. Usually some tenderness is noted over the affected compartment and over the middle to lower third of the tibia (from associated periostitis). Examination immediately after a period of exercise is often required to provoke the symptoms and expose the signs to the examiner. In this situation, tenderness over the affected muscle compartment and palpable firmness are more common. Muscle herniations through fascial defects are often discovered, but there is significant divergence of opinion on both their significance and incidence.317,399,404,409 Radiologic evaluation is warranted in all cases because stress fractures can mimic these symptoms and an occult tumor can be found even in an unlikely setting (Fig. 30-11). Lack of specific localized uptake on the technetium bone scan or no increase in signal on T2-weighted MRI images of the painful area effectively rules out a stress fracture.339,354 MRI has gained increasing acceptance in the evaluation of chronic leg pain and compartment syndromes, with some advocating its use as a reliable, reproducible, and noninvasive diagnostic tool with no radiation exposure.309,351,411 In general, the diagnosis of CECS can be made on clinical grounds. The syndrome can be confirmed with compartment pressure measurement.404,414,415 Although one would expect to have a certain agreed-on method and a specific pressure measurement for diagnosing compartment syndrome, this has not been the case. The suggested methods and the timing of the measurement have varied considerably.407,415,421,428 Box 30-1 lists the criteria we use. The test for exertional compartment syndrome can be performed quickly with a digital pressure monitor, but the physician should always be certain that the numbers are consistent with the clinical picture before deciding the treatment option (Fig. 30-12).
Athletic Injuries to the Soft Tissues of the Foot and Ankle
![]() Video Clips 94 and 98-100)
Video Clips 94 and 98-100)
Section 1 Etiology of Injury in Sports
Historical Perspective
Epidemiology
Etiologic Factors
Biomechanical Abnormalities
Flexibility
Strength
Footwear and Orthoses
Playing Surfaces
Section 2 Chronic Leg Pain in Athletes
Differential Diagnosis
Origin
Differential Diagnosis
Nerve
Saphenous or superficial peroneal nerve entrapment, radiculopathy
Vascular
Popliteal artery entrapment syndrome, arterial endofibrosis, DVT
Muscle
Strain or tear, muscle hernia, tendinitis, tendinosis
Fascia
Chronic exertional compartment syndrome, interosseous membrane strain or tear
Osseous
Medial tibial stress syndrome, periostitis, stress fracture
Incidence
Chronic Exertional Compartment Syndrome
Definition
Incidence
Clinical Features
Diagnosis
Clinical Evaluation
Radiologic Evaluation
Pressure Measurements