Athlete with Shoulder Pain during Throwing/Overhead Motion
Lee A. Mancini
INTRODUCTION
Shoulder pain is a common complaint found in the athlete involved in throwing/overhead motions. The throwing motion seen in baseball, softball, and football is an unusual action that places tremendous stress on the shoulder joint complex. This overhead motion is also seen in swimmers, volleyball players, javelin throwers, and tennis players and in a repetitive nature can result in overuse shoulder pain and injury. The spectrum of pathology may range from shoulder multidirectional instability (MDI) with secondary impingement to rotator cuff and/or labral tears. While acute shoulder dislocations, subluxations, and labral tears can occur in the throwing/overhead athlete, the approach is reviewed in Chapter 10 Athlete with Shoulder Dislocation and Instability. The approach to overuse shoulder pain in the general or older athlete is reviewed in Chapter 12 Athlete with Overuse Shoulder Pain. The focus of this chapter is on the evaluation and management of shoulder pain in the throwing or overhead athlete, with center of attention being chronic shoulder instability and superior labral (SLAP) tears.
FUNCTIONAL ANATOMY
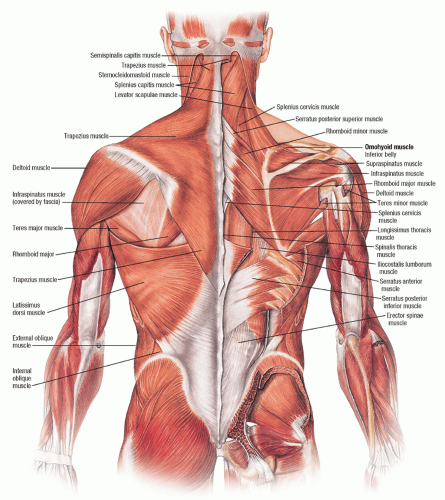
The shoulder joint is actually a complex of four articulations: the sternoclavicular joint, the acromioclavicular joint, the glenohumeral (GH) joint, and the scapulothoracic joint (Figs 11.1 and 11.2).
The GH joint has the widest range of motion of any joint in the body. It is a product of the incongruous nature of the GH joint and surrounding soft tissue envelope. This provides dynamic stability as well as varying degrees of passive stability with minimal restriction of motion (Fig. 11.3).
The static constraints of the GH joint include the labrum, the shoulder capsule, the coracohumeral ligament (CHL), the superior glenohumeral ligament (SGHL), the middle glenohumeral ligament (MGHL), and the inferior glenohumeral ligament (IGHL). The shoulder capsule has twice the surface area as the humeral head. All sides of the capsule, except the inferior portion, are reinforced by the rotator cuff.1 The CHL is a thin capsular fold that stretches from the base of the coracoid process to the transverse humeral ligament. It works together with the SGHL. The SGHL extends from the supraglenoid tubercle to the lesser tuberosity of the humerus. It works with the CHL to prevent inferior instability of the shoulder when the arm is adducted. A secondary role is to assist the shoulder capsule in resisting posterior instability when the shoulder is in the flexed, adducted, and internally rotated position. The MGHL goes from the mid anterior labrum to the lesser tuberosity. It functions as a secondary restraint to anterior translation of the humeral head. The IGHL is the major stabilizer of the GH joint. It is composed of anterior and posterior bands with an interposed axillary pouch. When the shoulder is abducted and externally rotated, the anterior band of the IGHL prevents anterior translation. When the shoulder is internally rotated, the posterior band prevents posterior translation. Which static constraint serves to prevent anterior dislocation depends on the degree of abduction in the shoulder. At 90° abduction it is the IGHL, at 45° it is primarily the MGHL with assistance from the subscapularis and the IGHL, and at 0° it is the subscapularis. The IGHL is the primary anterior stabilizer in throwing athletes.
In the GH joint, the humeral head has a surface area two to four times greater than that of the glenoid and a diameter two times greater than that of the glenoid. The glenoid labrum is a cartilage ring that appears triangular when seen in cross-sectional area. The labrum doubles the anterior-posterior (AP) depth of the glenoid from 2.5 to 5 mm2 and deepens the concavity of the glenoid. This increase in depth enhances the stability of the GH joint by increasing the contact surface area for the humeral head. A torn labrum results in a 20% loss in resistance to translation from a compressive load. The inferior labrum is a rounded fibrous structure which is firmly attached to the glenoid and is also continuous with the articular cartilage.2 The superior labrum can have a meniscal appearance and is attached loosely and is mobile. It is also the attachment site of the MGHL and SGHL. The long head of the biceps tendon originates from
the superior labrum and the supraglenoid tubercle. The Bufford complex, first described by Williams and Snyder in 1994, is a rare anatomic finding where a cord-like MGHL originates directly from the superior labrum at the base of the biceps tendon. The vascular supply of the labrum is better peripherally than centrally. The anterior, anterosuperior, and superior portion of the labrum have a decreased blood supply relative to other parts of the labrum.3
the superior labrum and the supraglenoid tubercle. The Bufford complex, first described by Williams and Snyder in 1994, is a rare anatomic finding where a cord-like MGHL originates directly from the superior labrum at the base of the biceps tendon. The vascular supply of the labrum is better peripherally than centrally. The anterior, anterosuperior, and superior portion of the labrum have a decreased blood supply relative to other parts of the labrum.3
Detachment of the superior labrum (superior labrum anterior to posterior) SLAP lesion rarely causes frank instability.
SLAP lesions often occur in association with an anterior labral lesion known as a Bankart lesion. SLAP lesions are classified as type I, II, III, and IV primarily.4 This classification system is based on Snyder’s classification system described in 1990 (Table 11.1). A type I SLAP lesion has fraying of the edge of the superior labrum. Type II is the most common type of SLAP lesion. In a type II lesion, there is fraying of the edge of the superior labrum as well as a detached biceps tendon anchor from the superior glenoid tubercle. Type III lesions consist of a bucket-handle tear of a meniscoid superior labrum with an otherwise normal biceps tendon attachment. Type IV lesions also contain the bucket-handle tear as well as an extension of this tear into the biceps tendon. Combined lesions have also been described usually as type II and III or type II and IV. These are cases where there is a significantly detached biceps tendon anchor, a type II lesion, in addition to either a type III or a type IV lesion3 (Fig. 11.4).
SLAP lesions often occur in association with an anterior labral lesion known as a Bankart lesion. SLAP lesions are classified as type I, II, III, and IV primarily.4 This classification system is based on Snyder’s classification system described in 1990 (Table 11.1). A type I SLAP lesion has fraying of the edge of the superior labrum. Type II is the most common type of SLAP lesion. In a type II lesion, there is fraying of the edge of the superior labrum as well as a detached biceps tendon anchor from the superior glenoid tubercle. Type III lesions consist of a bucket-handle tear of a meniscoid superior labrum with an otherwise normal biceps tendon attachment. Type IV lesions also contain the bucket-handle tear as well as an extension of this tear into the biceps tendon. Combined lesions have also been described usually as type II and III or type II and IV. These are cases where there is a significantly detached biceps tendon anchor, a type II lesion, in addition to either a type III or a type IV lesion3 (Fig. 11.4).
The dynamic constraints of the shoulder include the rotator cuff, the long head of the biceps tendon, and the scapular rotators. The rotator cuff and long head of the biceps are the most important stabilizers of the GH joint. The GH ligaments serve as passive stabilizers at extremes of motion.
TABLE 11.1 Types of SLAP Tears: Snyder’s SLAP Lesion Classification System | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
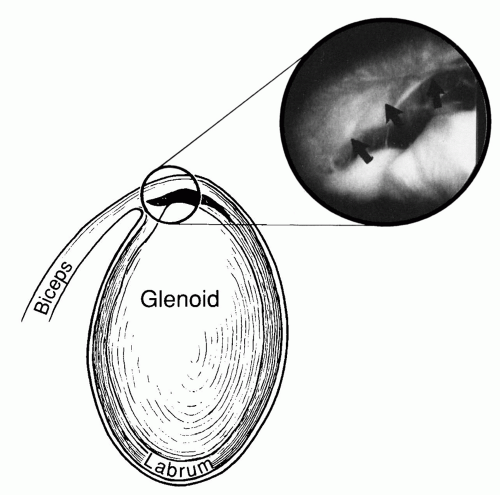 FIG. 11.4. Labral tear, SLAP lesion picture. Reprinted with permission from Bucholz RW, Heckman JD. Rockwood & Green’s Fractures in Adults. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2001. |
The rotator cuff consists of four muscles: the subscapularis, the supraspinatus, the infraspinatus, and the teres minor. The subscapularis arises from the anterior aspect of the scapula and attaches over the lesser tuberosity. It is innervated by the upper and lower subscapular nerves (C5, C6). Its function is internal rotation. The supraspinatus arises from the supraspinatus fossa of the posterior scapula, under the acromion, and attaches to the superior aspect of the greater tuberosity. It is innervated by the suprascapular nerve (C5, C6). The function of the supraspinatus is humeral head depression. The infraspinatus originates from the infraspinatus fossa of the posterior scapula and inserts on the posterior lateral aspect of the greater tuberosity. It is innervated by the suprascapular nerve (C5, C6). The function of the infraspinatus is external rotation. The teres minor arises from the lower aspect of the scapula and attaches to the lower aspect of the greater tuberosity. It is innervated by the axillary nerve (C5, C6) and its function is external rotation. Six different arteries supply the rotator cuff: the posterior humeral circumflex, the suprascapular, the anterior humeral circumflex, the acromial branch of the thoracoacromial, the subscapular branch of the axillary artery, and the suprahumeral branch of the axillary artery (Fig. 11.5).
The long head of the biceps tendon adds to the anterior stability of the shoulder by resisting excessive external rotation forces when the shoulder is abducted and externally rotated. The long head of the biceps tendon helps to decrease the stress on the IGHL. The scapula rotators are a collection of muscles that serve to manipulate the scapula in different directions. The middle division of the trapezius and the rhomboids major and minor promote scapular retraction. The trapezius and the serratus anterior create upward rotation of the scapula. Protraction of the scapula is caused by the serratus anterior. Depression of the scapula is caused by the lower division of the trapezius and the inferior serratus anterior. The levator scapulae and the upper division of the trapezius provide postural support.
Scapulohumeral rhythm is the 2:1 ratio between GH and scapulothoracic motion at the shoulder joint. For every two degrees of motion at the GH joint, there is one degree of motion at the scapulothoracic joint. In the pitching motion, the angular velocity of the shoulder reaches 6,100 degrees/sec. Internal rotation torque is 14,000 inch-pounds prior to the release of the baseball. The kinetic energy generated is 27,000 inch-pounds. The pitching motion is divided into six phases: wind-up, early cocking, late cocking, acceleration, deceleration, and follow through. The first three phases make up 80% of the pitching motion and in these phases the ball does not move forward. In the early cocking phase, the shoulder is flexed and abducted. In the late cocking phase, the shoulder is abducted 90°, extended 30°, and externally rotated 90° up to even 160°. In the acceleration phase, there is derotation of the shoulder (Fig. 11.6).
EPIDEMIOLOGY
Problems with the shoulder joint, specifically impingement and tearing of the rotator cuff tendon, tend to increase with patient age. A study done in 1995 found that only 4% of asymptomatic patients between the ages of 19 and 39 had a partial-thickness tear of the rotator cuff and there were no full-thickness tears. This is in comparison to 28% incidence of full-thickness tears and 26% incidence of partial-thickness tears in asymptomatic patients over the age of 60.5
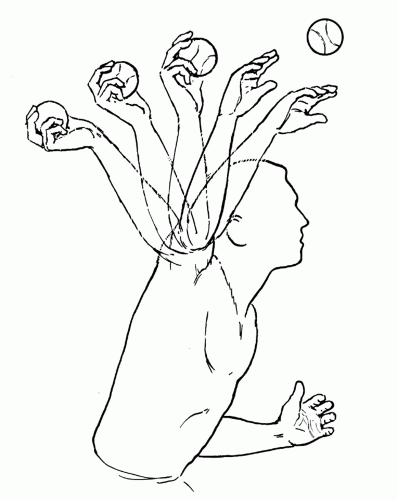 FIG. 11.6. Side view of throwing motion. MediClip image copyright © 2003 Lippincott Williams & Wilkins. All rights reserved. |
Any sport that involves overhead activity, including tennis, volleyball, baseball, golf, football (quarterbacks), and swimming, is at increased risk of tendinopathy or rotator cuff tear. Over 50% of elite tennis players have had shoulder pain from rotator cuff or biceps tendon injuries. Nearly 80% of swimmers have reported shoulder pain. Fifty-seven percent of pitchers suffer some form of shoulder injury during a season.6
NARROWING THE DIFFERENTIAL DIAGNOSIS
The challenge in evaluating the throwing or overhead athlete with shoulder pain is differentiating pain coming from functional weakness and chronic instability seen in MDI from structural injury including SLAP tears or rotator cuff tears (generally undersurface tears). Primary external impingement causing rotator cuff tendinosis (RCT) and tears are more frequent in older athletes. Secondary external impingement is the most frequent cause of pain in overhead athletes. Microinstability is the term used when overhead athletes have no perceptible instability of the GH joint. In athletes with microinstability, it is an overuse injury caused by weakness in rotator cuff and periscapular musculature. Microinstability can lead to injuries of the anterosuperior labrum.
History
Shoulder pain is a common complaint in the throwing athlete. Often the athlete will have minimal to no pain when not involved in his or her sport. The patient may complain of vague shoulder pain made worse by the overhead or throwing motion. Pain is typically distributed in the deltoid region but may also involve the anterior or posterior aspects of the shoulder joint.
In overhead throwing athletes, the throwing motion can be divided into several stages: wind-up, cocking, acceleration, deceleration, and follow through. Sometimes the cocking phase may be divided into early and late phases. The wind-up is the first part of the pitching motion; it has the most variability from pitcher to pitcher and the there is minimal stress on the shoulder. The early cocking phase starts when the pitcher’s hands break and the arm is abducted. The late cocking phase starts when the pitcher’s stride leg is planted on the ground and the arm is maximally abducted and externally rotated. In the late cocking phase, there is increased stress on the supraspinatus, infraspinatus, and teres minor. In the acceleration phase, the arm rotates at speeds greater than 7,000 degrees/sec in an explosive action. The late cocking and acceleration phases are the parts of the pitching motion where athletes tend to complain of pain the most. The deceleration phase begins when the ball is released and is the most violent phase of the throwing cycle, with maximal forces on the shoulder joint. The final phase is the follow through where the body moves forward until the arm motion stops.6 GH joint microinstability causing secondary external impingement occurs during the late cocking and early acceleration phases.
Important Questions
What sport of sports does the athlete play? Participating in any overhead sport such as volleyball, tennis, swimming, javelin, baseball, or softball increases the risk of shoulder pain and rotator cuff pathology. Overhead athletes are more prone to repetitive overuse injuries such as MDI, impingement syndromes, and subluxations. Is your dominant or nondominant shoulder affected? If the athlete is a baseball player, which position does he play? Pitchers are at greater risk than other players, with catchers and shortstops the next most likely positions to develop pain. For pitchers, their age, pitch selection, and arm angle are important. Skeletally immature pitchers throwing breaking pitches such as curveballs and sliders are at increased risk of injury. Pitchers throwing with a three-quarter arm angle instead of straight over the top have an increased risk for shoulder injuries. Previous treatments such as physical therapy, corticosteroid injections, and operative treatments will dictate how best to proceed in this situation.
Evidence-based Physical Examination
The challenge for most providers in evaluation of the shoulder is the large number of examination maneuvers available. Additionally, the overall sensitivity and specificity of each maneuver is generally low. Most maneuvers are better at ruling out a specific condition than ruling it in. Of note, most tests gain greater significance when several tests point toward a specific condition rather than a single isolated test.
The shoulder examination should progress in an organized and coordinated fashion as detailed below to minimize the above issues and arrive at an accurate diagnosis. A thorough neck and neurologic examination should be performed to rule out any potential referred or neurologic source of pain.
The shoulder examination should progress in an organized and coordinated fashion as detailed below to minimize the above issues and arrive at an accurate diagnosis. A thorough neck and neurologic examination should be performed to rule out any potential referred or neurologic source of pain.
Inspection
The first part of the shoulder examination should be inspection of the injured athlete. This should take place with the male athlete’s shirt removed or the female athlete in a tank top or sports bra. Inspect the deltoid for lateral flattening which is a sign of atrophy. Inspect the athlete from behind to look for atrophy of the rotator cuff muscles and atrophy of the periscapular muscles. Also look for asymmetry of scapular alignment.
Palpation
Palpate the acromioclavicular joint, subacromial space, biceps tendon, and the shoulder joint capsule for any tenderness.
Range of Motion (ROM)
Normal ROM of forward flexion of the shoulder is from 0° to 170-180°. Normal ROM for shoulder abduction is from 0° to 170-180°. External and internal rotation is evaluated in neutral position. From the posterior view of the patient, observe scapulohumeral rhythm and symmetry of scapular movement (Fig. 11.7).
Strength Testing
The empty can test is a test for supraspinatus weakness. The athlete forward flexes his or her shoulder to 90°, then abducts 30° to the plane of the scaula, and finally internally rotates until his or her thumbs are pointing at the ground. Weakness in the infraspinatus and teres minor is tested in external rotation in neutral against resistance. Internal rotation in neutral against resistance tests for weakness in the subscapularis. Other tests for subscapularis injury/pathology include the lift-off or belly-press tests.
Laxity Tests
Load and Shift Test
The load and shift test is used to confirm anterior and posterior shoulder laxity as well as the amount of translation of the humeral head on the glenoid. This test can be performed with the athletes in the seated or supine position. In the seated position, the athlete places his or her arm on the examiner’s hip. The examiner places one hand on the posterior shoulder GH joint and provides an AP force on the humeral head. The examiner’s other hand is placed on the athlete’s axilla. In the supine position, the patient is placed on the examining table with his or her scapula on the edge of the bed. The humeral head is off the bed to facilitate GH rather than scapulothoracic translation. In either position, the examiner grabs the athlete’s arm with both hands—one near the humeral head and one on the forearm near the elbow. The distal hand loads the humeral head. The proximal hand applies an AP force to shift the humeral head. Athletes are given a grade based on the amount of humeral head movement. The modified Hawkins grading is the most common grading method.7 Grade 0 means there is little or no humeral head movement. Grade 1 is when the humeral head rides up onto the glenoid rim. Grade 2 is when the humeral head can be dislocated but spontaneously relocates. Grade 3 is when the humeral head does not relocate when pressure is removed. It is rare for athletes with stable shoulders to have a positive result of Grade 2 or higher. It is the only test that has been validated to assess anterior and posterior laxity.7 The load and shift test has a specificity of 100% and a sensitivity of 8% to 50%.7 It has poor sensitivity in clinical setting, only 41% with unidirectional instability and 26% with bilateral multidirectional instability.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree