Athlete with Shoulder Dislocation and Instability
Amy Abbot
INTRODUCTION
The shoulder is the least constrained joint in the body, which affords it an incredible range of motion but also leaves it vulnerable to instability. Shoulder stability is dependent both on static stabilizers, including the glenohumeral articulation, the glenoid labrum, the capsule, and its associated glenohumeral ligaments, and on dynamic stabilizers consisting of the rotator cuff and the periscapular musculature. Instability itself should be thought of as a continuum of abnormal motion ranging from joint laxity to subluxation to frank dislocation. It is important to remember that just because a shoulder demonstrates excess motion does not mean that this motion is pathologic; on the contrary, it may be requisite for performance in certain sports.
Clinical presentation can be highly variable from complaints of vague shoulder pain to acute dislocation, and it is imperative to perform an in-depth history and physical examination to rule out other sources of shoulder pain. If instability is present, these will also be essential in guiding the choice of treatment options.
FUNCTIONAL ANATOMY
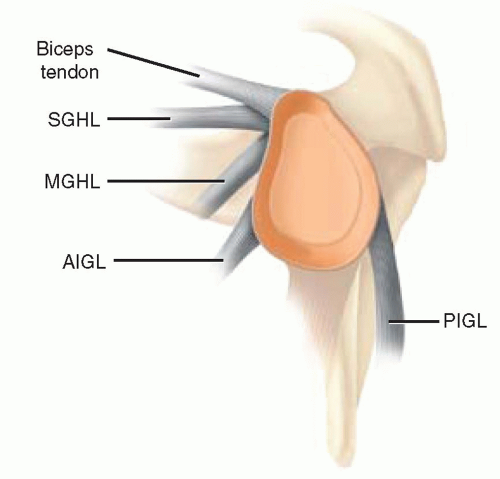
Static stabilizers in the shoulder consist of bony articulations, labrum, and capsuloligamentous structures (Fig. 10.1). The bony conformity of the glenohumeral joint alone generally does not play a large role in gross shoulder stability but rather works in concert with other static and dynamic stabilizers to keep the humeral head centered and compressed into the glenoid (adhesion-cohesion, concavity-compression, finite joint volume). The exception to this is when bone deficiency (either traumatic or dysplastic) of the glenoid or humeral head exceeds 20%, which can result in decreased force required for dislocation and lead to primary and recurrent subluxation and dislocation1, 2, 3, 4 (Fig. 10.2).
The importance of soft-tissue restraints for recurrent shoulder instability was first described in the early 1900s, with Bankart describing detachment of the anteroinferior labrum as the “essential lesion.”5, 6, 7 More recently, in-depth biomechanical studies have further elucidated the synergistic roles of the labrum, capsule, and the associated glenohumeral ligaments in maintaining shoulder stability.
The labrum is a fibrocartilaginous ring that is attached to the glenoid rim and to which the glenohumeral ligaments insert. The labrum assists in stability by adding up to 50% to the glenoid depth and to the conformity of the glenohumeral articulation. This allows the labrum to act as a bumper to glenohumeral translation, resisting translational forces by as much as 60%.3 It is important to remember that there is considerable natural variability to the labral attachment, particularly superior where it is attached much more loosely versus inferiorly where it is nearly confluent with the glenoid cartilage surface. Inability to recognize normal variants such as a sublabral foramen or Buford complex can result in inappropriate treatment. Labral lesions in isolation, though, have not been demonstrated to be sufficient to cause dislocation without a concomitant injury to the shoulder capsule and/or glenohumeral ligaments.1,8,9
The stabilizing action of the capsule and the associated glenohumeral ligaments is dependent on the position of the humerus in space and the force going through the glenohumeral joint. The superior glenohumeral ligament in concert with the coracohumeral ligament and rotator interval is the primary restraint to inferior translation when the arm is adducted and externally rotated. The middle glenohumeral ligament becomes the major anterior stabilizer as the arm is moved into increasing abduction and elevated to 45 degrees. The inferior glenohumeral ligament serves a wide variety of functions as a stabilizer since it spans like a hammock from the anteroinferior glenoid through the axillary pouch to the posteroinferior glenoid. As the humerus is abducted to 90 degrees, the inferior glenohumeral ligament becomes the major restraint to inferior translation. The anterior band tightens as the arm is placed in abduction and external rotation, resisting anterior translation, while the posterior band tightens with abduction and internal rotation, providing posterior instability.1,9
Dynamic stability is primarily provided by the rotator cuff, which compresses the humeral head into the glenoid and through coordinated contraction assists in keeping the humeral head well located on the glenoid face.8 The biceps also contribute to shoulder stability by resisting excessive rotatory forces, tending to stabilize anteriorly with the arm in external rotation and posteriorly in internal rotation.8,10,11 The other periscapular muscles that cross the glenohumeral
joint may also play a significant role in the maintenance of stability, but this has yet to be demonstrated scientifically. What has been demonstrated is that shoulder laxity and instability are associated with rotator cuff weakness and fatigue, and this may put the capsulolabral complex at risk.8,12
joint may also play a significant role in the maintenance of stability, but this has yet to be demonstrated scientifically. What has been demonstrated is that shoulder laxity and instability are associated with rotator cuff weakness and fatigue, and this may put the capsulolabral complex at risk.8,12
When the circumferential capsulolabral complex is disrupted and the delicate balance between static and dynamic restraints is altered, instability can result. The classic Bankart lesion is an anteroinferior capsulolabral injury, while a reverse Bankart is similarly located in the posteroinferior glenoid. If there is capsulolabral detachment without rupture of the periosteum of the glenoid, the complex can displace medially and scar down, resulting in an ALPSA (anterior labral periosteal sleeve avulsion) lesion.8,13 More recently, injuries superiorly on the glenoid known as SLAP (superior labral anterior to posterior) lesions have been implicated in shoulder instability, but before considering such lesions as pathologic, it is important to remember that there is significant natural variability of the labral anatomy in this area.8,14 Recent biomechanical studies have demonstrated that lesions in the 1 to 3 o’clock region typically showed no increase in instability, but when the lesion extended across the entire superior rim (10 to 3 o’clock), there was significant translation.8,14 Even without actual labral detachment, the capsule and ligaments can become elongated and attenuated and result in functional instability. Finally, the function of the capsuloligamentous complex can be compromised in a much less common avulsion of the ligaments from the humeral attachment site known as a HAGL (humeral avulsion of glenoid labrum) lesion.
EPIDEMIOLOGY
The vast majority (96%) of shoulder dislocations are the result of acute traumatic events such as a fall on an outstretched hand/arm (FOOSH), a forceful wrenching of the arm, or a direct collision. Only 4% are atraumatic in origin, typically secondary to genetically increased capsular laxity or to recurrent traumatic dislocation.9,15 Patients with capsular laxity secondary to genetic factors are much more likely to have multidirectional instability (MDI) and may experience more microinstability or subluxation versus frank dislocation. This distinction can be very useful in deciding on a treatment plan and determining the likelihood of recurrence. In fact, this has led to the TUBS (traumatic unidirectional Bankart surgery) versus AMBRI (atraumatic multidirectional
bilateral rehabilitation inferior capsular shift) classification, which combines diagnosis and treatment.
bilateral rehabilitation inferior capsular shift) classification, which combines diagnosis and treatment.
Age is also a critical factor in both the type of injury sustained during primary dislocation and the development of recurrent dislocation with nonsurgical management. A study by Rowe demonstrated that shoulder dislocations occur with a bimodal distribution with peaks in the 20s and 60s.15 In patients under age 40 years with primary dislocation, the most common injury is to the capsulolabral attachments (intracapsular), while in those above 40 years the most common injury is a tear of the rotator cuff (extracapsular).9,15 The development of recurrent dislocation has been widely demonstrated to be highly age dependent. In patients 20 years or younger with primary dislocation, the recurrence rate approaches 90%; in those between 20 and 40 years, this drops to around 60%; and in those over 40 years, this drops even further to 10% to 16%. This is a very important factor when deciding on options for management.9,15,16
NARROWING THE DIFFERENTIAL DIAGNOSIS
The differential diagnosis of an athlete presenting with shoulder instability may include traumatic dislocation, voluntary dislocation, glenohumeral subluxation, MDI, glenoid or humeral bone loss, HAGL lesion, and ALPSA lesion.
History
A thorough history is crucial to defining the etiology of instability and planning treatment. The history can often be directed by using a simple classification that divides instability into four major categories: (1) degree of instability—microinstability, subluxation, or dislocation; (2) frequency of instability—primary versus chronic; (3) etiology—traumatic, atraumatic, or acquired; and (4) direction of instability—unidirectional, bidirectional, or multidirectional.17
It is important to assess whether there is a history of a specific traumatic event or is the description more consistent with generalized laxity and repetitive microtrauma resulting in instability. The patient may complain of a “dead-arm syndrome,” the sensation that the arm went “dead” during an episode of contact, abduction, and external rotation or during throwing secondary to stretch of the brachial plexus as the humeral head subluxes. Determining the position of the extremity during instability events and location of pain about the shoulder can also provide important information about the direction of instability and the probability of associated pathology.
Important questions include the following: (1) What was the magnitude of trauma? (2) Was a reduction required? (3) How long was the disability after the event? (4) What activity or arm positions does the patient avoid? (5) How many episodes has the patient had? These questions will assist the surgeon in determining the direction of instability, whether the patient had a true traumatic episode with capsulolabral disruption, whether bone deficiency is likely, or whether the patient has generalized laxity as the primary etiology for the instability.18
The patient’s age, activity level, and arm dominance as well as direction and frequency of dislocation should be assessed. Younger age (<25 years) has consistently been demonstrated to be a risk factor for developing recurrent dislocation with conservative management alone. High rates of recurrence have been observed in collision and contact sports, but the exact correlation has not been defined. It is also important to ascertain whether the patient has previously tried a rehabilitation protocol and how successful this conservative management was in controlling instability events.19,20
Evidence-based Physical Examination
As with all shoulder complaints, physical examination should begin with a complete general shoulder examination, including assessment of the cervical spine, inspection of the shoulder to identify altered contour or muscular atrophy, location of tenderness (e.g., glenohumeral joint, acromioclavicular joint), neurologic evaluation, and assessment of shoulder motion (passive and active) and strength compared to the opposite shoulder. In acute dislocation, the normal shoulder contour can be lost. Anterior dislocations tend to exhibit a hollow in the deltoid, with the humeral head medially and inferiorly displaced. The arm is held in an abducted and externally rotated position. Posterior dislocations can be more difficult but may show posterior prominence with the humerus held in adduction and internal rotation. After reduction, neurologic deficit may be present, particularly of the axillary nerve. This can manifest acutely as weakness and decreased sensation in the axillary distribution and chronically with muscular wasting and weakness. Weakness, loss of motion, or dyskinesis can also indicate disruption of the rotator cuff.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree