Athlete with Overuse Shoulder Pain
Michael Brown
INTRODUCTION
Shoulder pain is one of the most common complaints encountered in a sports medicine clinic. Subacromial or internal impingement and tears of the rotator cuff are the most common causes for shoulder pain. Isolated acromioclavicular (AC) joint degeneration may also cause shoulder pain similar to that of impingement syndrome or rotator cuff tendonopathy. There are many factors that may be related to the development of shoulder pain in the athlete, including anatomy, repetitive motion, fatigue, or altered mechanics of the shoulder.
FUNCTIONAL ANATOMY
At the most basic level, the shoulder is composed of the humerus, the clavicle, and the scapula, which is further divided into the acromion, the coracoid, and the glenoid. The shoulder consists of four different articulations: the sternoclavicular (SC), the AC, the glenohumeral, and the scapulothoracic. The combination of motion at these articulations allows for the greatest range of motion of any joint in the body, with the majority of the stability of the joints coming from the surrounding soft-tissue elements.
The clavicle serves to connect the upper extremity with the axial skeleton. The SC joint is the only true synovial joint in the shoulder complex and lacks bony stability. The AC joint also has a combination of capsular and ligamentous stabilizers, consisting of the joint capsule to prevent anterior/posterior translation, with the named AC ligaments being thickenings of this capsule. The trapezoid coracoclavicular ligament prevents posterior translation and contributes to superior stability with the conoid coracoclavicular ligament.1
The scapula has many muscular attachments that secure its position on the thorax and is otherwise only held in position by the AC and coracoclavicular ligaments. The muscles involved include the trapezius, levator scapulae, serratus anterior, pectoralis minor, and the rhomboids. The motion achieved by these muscles allows the scapula to be positioned for maximal stability of the glenohumeral joint during upper extremity motion, namely maintaining the glenoid under the humeral head. The scapulothoracic rhythm is defined as the relative motion between the scapulothoracic articulation and the glenohumeral joint during abduction of the arm. Over the entire arc of abduction, the glenohumeral joint moves more, but the difference is far greater at the beginning of abduction than at the end.2
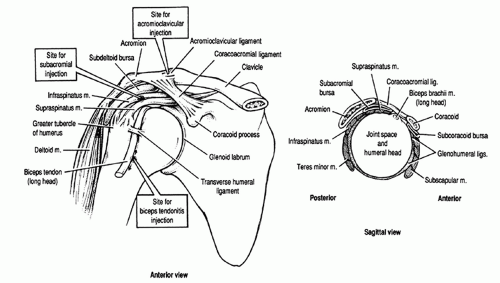
The glenohumeral joint is surrounded by the rotator cuff muscles, which are the primary dynamic stabilizers of this joint (Fig. 12.1). The supraspinatus originates in the posterior-superior scapula, just superior to the scapular spine, and runs under the acromion to insert onto the greater tuberosity of the humerus.
It is active throughout scapular-plane abduction of the arm, and loss of innervation by the suprascapular nerve will lead to a 50% loss in abduction torque.3 The infraspinatus and teres minor run together from their origination on the posterior scapula, just inferior to the scapular spine, to their insertion on the posterior aspect of the greater tuberosity. They work together during external rotation and extension of the humerus. The infraspinatus is primarily involved when the arm is at the side, and the teres minor is the major muscle for external rotation when the shoulder is elevated 90 degrees.4 The tendinous insertions of these three muscles, the supraspinatus, infraspinatus, and teres minor, are not separate at the level of the greater tuberosity. The subscapularis is the fourth rotator cuff muscle. It originates on the anterior surface of the scapula and inserts on the lesser tuberosity of the humerus. Contraction leads to internal rotation and flexion of the humerus.
The deltoid is the largest of the glenohumeral muscles. It has a tripennate origin from the clavicle, acromion, and scapular spine and inserts midway down the lateral humerus on the deltoid tubercle. The anterior portion of the deltoid performs forward flexion and contributes to abduction. The posterior portion extends and adducts the humerus, while the middle portion abducts the arm. It is possible for the deltoid to fully abduct the arm without supraspinatus involvement. Loss of the deltoid through paralysis of the axillary nerve results in a 50% loss of abduction torque.3
The biceps brachii originate from the scapula, with the long head originating from the superior articular margin of the glenoid, where it joins with the labrum within the
synovial sheath; the short head originates from the coracoid, where it joins with the tendon of the coracobrachialis to form the conjoined tendon. Because the muscle extends from the scapula to the elbow, it traverses both the shoulder and the elbow and can therefore have effects at both joints. At the elbow, the biceps are the primary supinators and have a large role in flexion as well. The long head of the biceps serves as an active stabilizer of the glenohumeral joint as it passes along the bicipital groove on the humeral head and onto the glenoid.5 This position allows it to act as a restraint to superior migration of the humeral head as well as anterior migration of the head.6 This action becomes extremely important in the presence of a massive rotator cuff tear.
synovial sheath; the short head originates from the coracoid, where it joins with the tendon of the coracobrachialis to form the conjoined tendon. Because the muscle extends from the scapula to the elbow, it traverses both the shoulder and the elbow and can therefore have effects at both joints. At the elbow, the biceps are the primary supinators and have a large role in flexion as well. The long head of the biceps serves as an active stabilizer of the glenohumeral joint as it passes along the bicipital groove on the humeral head and onto the glenoid.5 This position allows it to act as a restraint to superior migration of the humeral head as well as anterior migration of the head.6 This action becomes extremely important in the presence of a massive rotator cuff tear.
The bony anatomy of the glenohumeral joint itself is what allows for such a large range of motion, but it provides only minimal stability. The humeral head is slightly elliptical and is larger in the vertical dimension. The articular surface typically forms a 150- to 160-degree arc; it is 45 degrees from the shaft and is retroverted 30 degrees relative to the transcondylar axis of the distal humerus.7, 8, 9 The glenoid is also larger in the vertical dimension and is angled slightly superiorly and posteriorly to the plane of the scapula.
The glenohumeral capsular and ligamentous structures provide the majority of the static stability for the glenohumeral joint. The joint capsule has nearly twice the surface area of the humeral head, which allows for a large range of motion.10 Depending on the position of the arm, selective portions of the capsule become taut to provide support for the humeral head; when the arm is by the side, the superior capsule is tight and the inferior capsule is loose. There are three anterior glenohumeral ligaments (GHLs), which provide reinforcement for the anterior capsule; they are named for their humeral insertions: superior, middle, and inferior. The superior GHL prevents inferior subluxation when the arm is at the side.11 The middle GHL resists anterior translation with the arm in 45 degrees of abduction and external rotation.12 The inferior GHL acts as a sling for the humeral head; with the arm abducted and externally rotated, the anterior band limits anterior translation as well as inferior subluxation; the posterior band becomes helpful in limiting inferior subluxation when the arm is abducted more than 45 degrees.11,13
The labrum is the final soft-tissue structure important for glenohumeral joint stability through its wide range of motion. It is positioned on the periphery of the glenoid and is the insertion point for the capsuloligamentous structures discussed earlier.14 Through its position, it increases the surface area of the glenoid and deepens the socket by 50%.15
EPIDEMIOLOGY
Problems with the shoulder joint, specifically impingement and tearing of the rotator cuff tendon, tend to increase with patient age. A study done in 1995 found that only 4% of asymptomatic patients between the age of 19 and 39 had a
partial-thickness tear of the rotator cuff and there were no full-thickness tears. This is in comparison to 28% incidence of full-thickness tears and 26% incidence of partial-thickness tears in asymptomatic patients over the age of 60.16
partial-thickness tear of the rotator cuff and there were no full-thickness tears. This is in comparison to 28% incidence of full-thickness tears and 26% incidence of partial-thickness tears in asymptomatic patients over the age of 60.16
Patients at increased risk of developing impingement syndrome and rotator cuff tendonopathy include both athletes and laborers. Any sport that involves overhead activity will place a player at risk; these include tennis, volleyball, baseball, golf, football (quarterbacks), and swimming. Laborers, such as carpenters, mechanics, or painters, who perform the majority of their work overhead are also at increased risk.
NARROWING THE DIFFERENTIAL DIAGNOSIS
The differential diagnosis of shoulder pain includes rotator cuff disorders (tendonopathy, partial-thickness or full-thickness tears), glenohumeral instability (more common in younger overhead athletes), cervical radiculopathies, calcific tendonitis, adhesive capsulitis, degenerative joint disease of the glenohumeral or AC joints, and peripheral nerve compression.17
History
Common complaints related to the shoulder will include feelings of stiffness, weakness, pain (typically anterolateral or posterolateral), or sleep disturbance. Pain is typically exacerbated by any sort of overhead activity, such as putting things away in overhead cabinets/shelves. Decreased endurance, accuracy, or speed is a common complaint among overhead athletes. Many women will report difficulty styling their hair. Any or all of these symptoms may be found in patients with AC joint arthritis, subacromial impingement, internal impingement, or tears of the rotator cuff tendon.
Patients with isolated AC joint arthritis present with symptoms that are consistent with all of the most common shoulder pathologies: dull ache over the deltoid area and pain with motion of the shoulder. Reaching for something in front of the opposite shoulder (cross-body adduction) is the most irritating to patients with as yet isolated AC joint arthritis.
In subacromial impingement, patients typically complain of pain, generally in the anterior/superior aspect of the shoulder. Depending on the time course, they may also report weakness and/or stiffness of the affected shoulder. Subacromial impingement is typically insidious in onset. However, some patients may report an acute event that led to traumatic bursitis that eventually develops into a chronic impingement syndrome. A complete history will be helpful in the diagnosis: location of pain, timing of pain (day or night), activities that exacerbate/alleviate pain, treatment modes already attempted (therapy, medications, injections, activity modifications, operations). Remember, true subacromial impingement is typical in patients over the age of 40. In younger patients, other diagnoses, such as glenohumeral instability, labral pathology, or internal impingement, should be considered.
Internal impingement is a source of posterior shoulder pain and can mimic both subacromial impingement as well as rotator cuff tears. However, internal impingement most frequently occurs in overhead athletes younger than 40 years of age. Symptoms of internal impingement are similar to those of subacromial impingement, with a slow, insidious onset of shoulder pain eventually leading to subjective weakness and stiffness of the affected shoulder. The major difference, however, is the location of the pain. Internal impingement typically presents with posterior shoulder pain, as opposed to anterior pain associated with subacromial impingement. Pain is usually associated only with the specific activity that brings the shoulder into the offending position of external rotation, abduction, and extension. Pitchers may specifically report an increase in the time required for warm-up or decreased endurance.18
Tears of the rotator cuff may be partial- or full-thickness. Interestingly, a recent study found that 73% of patients with partial-thickness tears reported significant and severe pain at night, as compared to only 50% of patients with full-thickness tears. Comparing preoperative patients’ complaints with intraoperative findings, this same study also found that bursal-sided tears tended to cause more pain than intratendinous or articular-sided tears.19 Patients over the age of 40 who suffer a traumatic dislocation are at high risk for having an acute rupture of the rotator cuff. Typically, however, rotator cuff tears are more indolent and chronic in nature, with a progression from subacromial or internal impingement to partial tears to full-thickness tears. Patients may have waxing and waning symptoms depending on their activity levels, and many patients will have made lifestyle adaptations to avoid the pain associated with the pathology.
Evidence-based Physical Examination
Examination of the shoulder should always include examination of both shoulders and begins with simple inspection. The shoulders should be exposed as much as possible while maintaining patient modesty. Standing behind the patient, inspect the scapula and periscapular muscles. Look for any evidence of scapular winging or muscle atrophy in the supraspinatus or infraspinatus fossa. Obvious muscle atrophy in the rotator cuff muscles can be helpful in the diagnosis of a full-thickness tear of the tendon but may also be linked to peripheral nerve compression syndromes, such as the infraspinatus wasting seen in patients with glenoid notch cysts. In a study of 400 patients, it was found that patients who had supraspinatus weakness, weakness in external rotation, and a positive impingement sign had a 98% probability of having a rotator cuff tear.20
Ask the patient to raise his or her arms over the head and observe the motion of the scapulae in relation to each other as well as in relation to the glenohumeral joint—is it a smooth motion or does the patient have to manipulate his or her shoulder to be able to achieve maximal elevation? Notice if any local muscles, such as the trapezius, have been recruited to help with shoulder motion. During this time you should also examine the skin for any overlying lesions or
changes or any obvious masses. In AC joint arthritis, a painful arc will be noted in a range that is higher in elevation (120 to 180 degrees) compared to the painful arc noted with cuff impingement (60 to 120 degrees).21
changes or any obvious masses. In AC joint arthritis, a painful arc will be noted in a range that is higher in elevation (120 to 180 degrees) compared to the painful arc noted with cuff impingement (60 to 120 degrees).21
Next, palpate potential areas of pain and inflammation to see if this will recreate or elicit the patient’s pain. These areas include the long head of the biceps as it passes along the anterior humeral head in the bicipital groove, the tendinous insertion of the rotator cuff muscles on the greater tuberosity, the AC joint, and the posterior shoulder. Leaving a hand over the shoulder while passively or actively moving the shoulder will allow the examiner to assess for crepitus related to degenerative joint disease, which will often accompany shoulder impingement to some degree. This is again an important time to rule out any underlying masses or abnormalities that would need to be investigated further.
There are multiple tests described to attempt to diagnose shoulder impingement or to highlight weakness in the various rotator cuff muscles. However, they are not all equal in terms of their sensitivity and specificity and, therefore, their clinical usefulness. In 2005, Park et al.22 tested eight different common examination techniques in patients with varying degrees of rotator cuff pathology: bursitis without a tear, partial-thickness cuff tear, and full-thickness cuff tear. There have been a few studies to compare the accuracy of these tests in patients with simple bursitis versus any degree of cuff tear, but Park’s study is the only one that divided the cuff tear group into partial or complete tears based on intraoperative findings. The tests, described in subsequent paragraphs, include the Neer impingement sign, Hawkins impingement sign, painful arc sign, supraspinatus muscle strength test, Speed test, cross-body adduction test, drop-arm sign, and infraspinatus muscle strength test (Fig. 12.2).
The Neer impingement sign (Fig. 12.2A) is defined as pain with passive forward flexion of the arm until either full elevation is reached or the patient expresses pain in the anterior/lateral shoulder. It is considered a positive test if the pain arises during forward flexion of 90 to 140 degrees.23
The Hawkins-Kennedy impingement sign (Fig. 12.2B) starts with the arm at 90 degrees of forward flexion and the elbow bent. The arm is then brought into internal rotation until either the patient describes pain or rotation of the scapula is observed. This test is considered positive when the patient expresses pain during the maneuver.
The painful arc sign asks the patient to actively elevate the arm in the scapular plane until full elevation is achieved and
then lower the arm in the same plane. It is considered positive if the patient notices pain or catching between 60 and 120 degrees of elevation.
then lower the arm in the same plane. It is considered positive if the patient notices pain or catching between 60 and 120 degrees of elevation.
Next, the supraspinatus muscle test (Fig. 12.2C) attempts to isolate this muscle from the other cuff muscles. The patient is asked to elevate his or her arm to 90 degrees and either maintain neutral or slight internal rotation. The examiner then attempts to resist the patient’s active abduction of the arm. This test is positive if the patient is unable to sustain the contraction due to pain/weakness.
The Speed test starts with the patient fully extending his or her elbow and then elevating the arm to 90 degrees of forward flexion. The forearm is maintained in full supination while the examiner applies a downward force. Again, pain, or inability to resist the downward force, is considered positive.
The cross-body adduction test brings the arm to 90 degrees of forward flexion and then adducts the arm across the body. A positive test is defined by pain during this maneuver.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree