Athlete with Neck Pain
Vasilios Chrisostomidis
Jake D. Veigel
INTRODUCTION
Acute and overuse neck injuries are common conditions encountered among athletes. Approximately 8.7% of all new cases of spinal cord injuries in the United States result from sports.1 It is important for medical providers who care for an athletic population to be familiar with the various causes of neck pain, which may range from mild cervical strains to catastrophic spinal cord injuries. This is accomplished by an understanding of the anatomy of neck, a working knowledge of the common causes of neck pain, and an understanding of the signs and symptoms of a serious cervical injury.
When dealing with a possible cervical emergency during an athletic event, basic cardiopulmonary resuscitation and trauma management guidelines should be followed. It is important to keep the injured athlete immobilized until cervical spine injury is ruled out. Unconscious athletes should always be assumed to have a cervical spine injury until proven otherwise. Shoulder pads and helmets should always be left on in evaluation of football and hockey athletes. The facemask may be cut away if needed for airway management, and jaw thrust maneuver applied if necessary. The helmet should only be removed if the airway cannot be maintained or if the helmet prevents cervical immobilization. Patient should be log rolled on a backboard and transported to the nearest hospital. If one functions as a team physician, it may be prudent to practice this type of drill with your athletic training staff so that everyone is aware of his or her role.
FUNCTIONAL ANATOMY
The function of the vertebral column is to protect the spinal cord. The vertebrae of the cervical spine are smaller and more delicate than those of the thoracic and lumbar spine. Despite this, they are often required to dissipate a significant amount of force, especially in collision sports.
The atlas and axis (C1 and C2) work together as a unit to permit 50% of cervical spine motion. The atlanto-occipital joint permits flexion and extension, while the atlantoaxial joint permits the majority of rotation.2 Varying amounts of flexion, extension, lateral bending, and rotation occur from C3 to C7.
The vertebral bodies form the anterior aspect of the spinal column. A bony lip on the lower surface of the vertebral body forms the uncovertebral joint with the adjacent vertebrae. There are intervertebral discs below C2 to provide shock absorption and cushioning for the vertebral column.
The anterior and posterior longitudinal ligaments provide stabilization for the vertebral bodies. The posterior column is made up of the pedicles, laminae, facets, and spinous processes. The facet joints are the posterior articulations of the vertebrae. The posterior column is stabilized by the nuchal ligament complex, which is made up of the supraspinous, interspinous, and infraspinous ligaments, in addition to the ligamentum flavum and capsular ligaments. Damage to these may result in cervical spine instability.
The spinal cord originates from the medulla oblongata and travels caudally through the vertebral foramina until it terminates in the lumbar region. The spinal cord is composed of three tracts, whose function and location may help to determine the site of an injury. The posterior columns carry fine touch, vibration sense, proprioception, and pressure from the ipsilateral side. The corticospinal tract is located in the posterolateral spinal cord and carries motor fibers to the ipsilateral side. The spinothalamic tract is located in the anterolateral spinal cord and carries pain and temperature fibers from the contralateral side.
Paired spinal nerve roots containing motor and sensory neurons exit from the spinal cord at each vertebral level via the intervertebral foramina. There are eight pairs of cervical spinal nerves named for the vertebral body above which they exit. Spinal nerves are subject to pressure phenomena from disc herniation or foraminal narrowing. The sensory cervical dermatomes are listed (Fig. 9.1).
The biceps and brachioradialis reflexes are mediated by the C5-6 roots and the triceps reflexes are mediated by the C6-7 nerves roots (Table 9.1).
The muscles of the neck may be subdivided into anterior and posterior divisions. The anterior aspect includes the platysma, sternocleidomastoid, anterior vertebral muscles
(longus colli, longus capitis, rectus capitis anterior, and rectus capitis lateralis), and the lateral vertebral muscles (scalene muscles).
(longus colli, longus capitis, rectus capitis anterior, and rectus capitis lateralis), and the lateral vertebral muscles (scalene muscles).
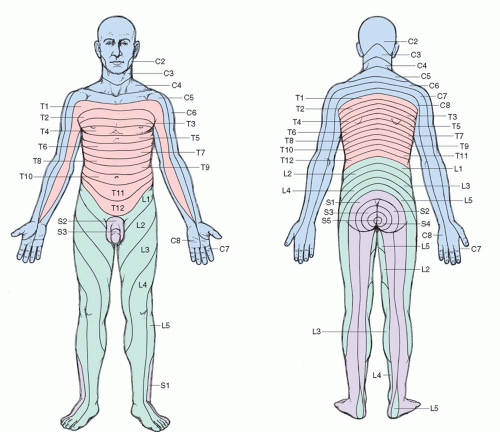 FIG. 9.1. Distribution of dermatomes on the skin. Reprinted with permission from Stedman’s Medical Dictionary. 27th ed. Baltimore: Lippincott Williams & Wilkins; 2000. |
TABLE 9.1 Peripheral Motor Nerve Innervation | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The sternocleidomastoid muscle allows for flexion, lateral bending, and neck rotation. The anterior vertebral muscles assist in neck flexion, rotation, and lateral bending.
The posterior division includes the trapezius, splenius capitis, semispinalis capitis, and levator scapulae. The posterior group is stronger than the anterior group and is important in maintaining posture as well as providing neck stabilization.
The important vessels in the neck include the common carotid arteries, vertebral arteries, jugular veins, and vertebral veins. The common carotid further separates into the external and internal carotids. The vertebral arteries join together to form the basilar artery of the brain. Damage to the vertebral arteries associated with cervical spine or neck trauma can result in death.3
EPIDEMIOLOGY
It is estimated that 10% to 15% of football players experience an injury to the cervical spine; fortunately, a majority of these are self-limited stingers/burners. The overall incidence of spinal cord injury in the high school and college population is around 1 in 100,000.4 Most are incomplete with preservation of varying degrees of neurologic function. In an analysis of football players from 1977 to 1989, catastrophic spinal cord injuries were secondary to fracture/dislocations or burst fractures in 33% and 22% of the cases, respectively.2 Cervical spine injuries are also seen in ice hockey, rugby, wrestling, gymnastics, and water sports (e.g., diving).5
The prevalence of degenerative disc disease is about 10% in the second decade of life and progresses linearly to 95% to 100% by age 70 years.6
NARROWING THE DIFFERENTIAL DIAGNOSES
History
This should include the full characterization of the neck pain as well as its duration and distribution. Any significant past medical history should be reviewed, especially any previous neck pain or neck surgery. Important questions include the following factors:
Location of pain
Onset/duration of pain
Radiation of pain
Numbness/tingling in extremities
Decreased motor strength
Exacerbating/alleviating factors
Previous examination/treatment/diagnostic tests
Mechanism of injury
Flexion injuries (including spearing) compress the anterior elements and disrupt the posterior elements, causing vertebral body fractures, dislocations, and rupture of the posterior ligaments or posterior discs.
Extension injuries compress the posterior elements and disrupt the anterior elements, causing damage to the spinous process, facets, and anterior ligaments or discs.
Cervical spine in neutral results in dissipation of energy into the cervical muscles—if the force is great enough, compression fractures may result.
Evidence-based Physical Examination
The physical examination plays a crucial role in narrowing your differential diagnosis by assessing for structural as well as neurologic deficits. A thorough and organized examination as outlined in the following sections is very important and will help in consistency.
Inspection
Perform from anterior, posterior, and lateral views. Note posture as well as muscle atrophy or deformity. Check for normal cervical lordosis—its absence may be consistent with cervical spasm. Inspection may reveal ecchymosis or swelling at the level of injury.
Palpation
One should evaluate for point tenderness over the spinous processes and lateral processes. Note any hypertonicity of the musculature on examination consistent with muscle spasm. Note for any step off if there was a history of trauma.
Range of Motion
Perform active range of motion (ROM) prior to passive ROM.
Evaluate flexion and extension by asking the patient to touch his or her chin to the chest and then look up at the ceiling.
Evaluate lateral bending of the neck, with normal being 45 degrees.
Evaluate lateral rotation, with normal being from 60 to 80 degrees.
Strength Testing
Strength should be tested in all planes (flexion, extension, lateral bending, and rotation).
Special Tests
Spurling Maneuver
Patient’s neck is extended and rotated toward the involved side as axial compression is applied. If there is pathology at the root or foramen, symptoms are recreated because this position narrows the intervertebral foramen on the affected side. Early studies have shown the sensitivity to be 40% to 60% with a specificity of 92% to 100%.7 More recent studies have shown Spurling test to have a sensitivity of 92% and specificity of 95% with positive predictive value of 96.4% and negative predictive value of 90.9%.8
Distraction Test
Manual vertical cervical traction is applied to confirm the diagnosis of radiculopathy. This maneuver temporarily relieves pressure at the level of the disc and facet joints, which may in turn temporarily relieve the patient’s symptoms. This test is reported to have a sensitivity of 40% to 43% and sensitivity of 100%.7
Neurologic
Neurologic symptoms may suggest a central lesion, radiculopathy, or peripheral nerve entrapment. A detailed neurologic
examination includes upper extremity strength testing, deep tendon reflexes at the triceps, brachialis and brachioradialis, sensation testing, and cranial nerve evaluation. Sensation should be evaluated and any deficits correlated with appropriate peripheral nerve distribution or dermatome.
examination includes upper extremity strength testing, deep tendon reflexes at the triceps, brachialis and brachioradialis, sensation testing, and cranial nerve evaluation. Sensation should be evaluated and any deficits correlated with appropriate peripheral nerve distribution or dermatome.
Diagnostic Testing
Laboratory
Routine laboratory studies are generally not required with acute or overuse neck pain or injuries. If suspected autoimmune etiology for overuse neck pain exists, sedimentation rate along with rheumatoid factor, antinuclear antibody test, and human leukocyte antigen B27 may be considered based on pretest probability and clinical scenario.
Imaging
Athletes with suspected cervical spine injury often require radiologic evaluation. Three views, including anteroposterior (AP), open-mouth odontoid, and cross-table lateral, are usually recommended. In addition, one may consider flexion and extension radiographs of the spine if instability is suspected and acute fracture excluded. Oblique views may be included to assess for facet degenerative joint disease in the appropriate setting/age of athlete.
Computed tomography (CT) may be indicated when suspicion of cervical fracture exits despite negative radiographs. It may also play a role when area of the cervical and upper thoracic spine may not be visualized with plain radiographs.
Magnetic resonance imaging (MRI) may be helpful in evaluation for nerve or disc injury and should be considered in any athlete that has spinal cord symptoms (transient quadriplegia, burning hands syndrome, or other bilateral sensory or motor deficits).
Other Testing
Electrodiagnostic testing may be indicated for evaluation of peripheral nerve injury. Complete details are outlined in Chapter 23, “Athlete with Peripheral Nerve Injuries.”
APPROACH TO THE ATHLETE WITH CERVICAL STRAIN
Cervical strains are the most common type of cervical injury in athletes and may occur from both acute and overuse mechanisms. Common mechanisms in athletics include whiplash force secondary to a fall or being tackled. Cervical strains can also occur from weight lifting or repetitive strain to the cervical and trapezius muscle groups. Primary goal is differentiating simple cervical strain from more serious etiologies including cervical disc or cord conditions as well as occult fractures.
HISTORY AND PHYSICAL EXAMINATON
Pain is usually localized with some stiffness and decreased ROM. There are no radicular symptoms and no neurologic deficits by history or physical examination.
DIAGNOSTIC TESTING
Radiologic studies are usually not indicated in the acute management unless pain is secondary to trauma. They may play a role ruling out underlying degenerative changes as well as occult fractures or instability in the appropriate clinical setting. MRI or electrodiagnostic studies are rarely needed unless radicular symptoms are present or symptoms persist despite conservative management.
TREATMENT
Nonoperative
Management is usually conservative and includes ice, heat, nonsteroidal anti-inflammatory drugs (NSAIDs), and relative rest.
Manual manipulation and physical therapy are helpful in resolving symptoms.
Operative
Operative intervention plays no role for cervical strains.
Prognosis/Return to Play
Prognosis is generally excellent. The athlete may return to play when examination reveals painless full ROM and full strength.
Complications/Indications for Referral
If symptoms persist, consider further evaluation with radiographs, MRI, and specialist referral.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








