Athlete with a Head or Facial Injury
Peter Hoth
Zachary A. Geidel
INTRODUCTION
Head and facial injuries in athletes often create anxiety in the provider caring for the athlete, as these injuries can be a source of significant morbidity, disability, disfigurement, or even death. Types of head injury encountered during sports activities include concussion, also known as mild traumatic brain injury (MTBI), second-impact syndrome, postconcussion syndrome, and intracranial hemorrhage. Facial injuries include dental injury, facial fractures, nasal fractures, epistaxis, and ocular injuries.
Concussion is the most common head injury encountered in sport, with as many as 300,000 concussions occurring annually in the United States due to sports participation.1 Approximately 90% or more of concussions do not involve loss of consciousness.2,3 Thankfully, the rates of head and facial injuries are decreasing in sport due to the implementation of helmets and facial protectors. Levy et al. (2004) showed a 74% decrease in fatalities and an 86% decrease in serious head injury since 1976 due to the implementation of the National Operating Committee on Standards for Athletic Equipment (NOCSAE) helmet standards as well as the implementation of new tackling laws to prevent spearing in football.4
PATHOPHYSIOLOGY
The mechanism of concussion can be a direct blow to the head, indirect trauma suffered during a fall, or a whiplash-type injury (Fig. 2.4). The underlying pathophysiology is an area of active research, with current data drawn largely from animal models and more severe forms of brain trauma in humans. The current theory proposes that a concussion results in a neurometabolic cascade that creates an increased glucose demand to restore normal cell membrane ionic homeostasis with a concomitant decrease in cerebral perfusion at the cellular level.5 This can lead to axonal injury and potential cell death. While the acute onset of ionic changes occurs over hours, late onset effects can take days to weeks to resolve with normalization of brain function.5
Other etiologies of altered cognition due to a head injury other than concussion or intracranial bleed include second-impact syndrome and postconcussion syndrome. Second-impact syndrome is defined as a repeat head insult that occurs prior to the complete resolution of initial concussion, which may not have been recognized or evaluated. There is currently much debate regarding the prevalence and etiology of second-impact syndrome, but the most widely held position is that the brain loses its autoregulatory ability due to the first concussion, and with onset of the second injury, there is rapid onset of cerebral edema, often leading to significant morbidity and mortality, despite aggressive and rapid treatment.3 Although second-impact syndrome is not seen in all athletes that return to play with ongoing concussive symptoms, the severe and devastating nature of this condition is one of the reasons why it is critical that athletes are asymptomatic prior to returning to play.
FUNCTIONAL ANATOMY
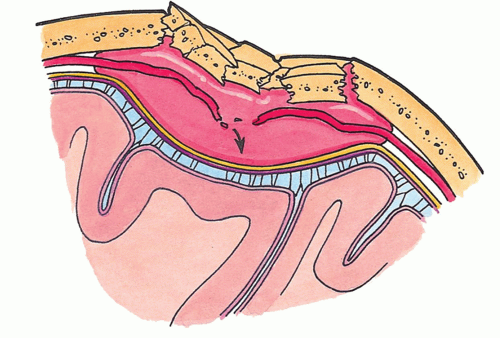
Given that concussion is the most common traumatic head injury, it is important to understand the anatomy of the brain (Fig. 2.2). The brain is a soft tissue structure floating in and surrounded by cerebrospinal fluid inside a thick, bony skull. If there is a direct or an indirect injury to the skull, the brain will move within the skull, colliding with the inner lining of the skull and causing a soft tissue injury or a concussion. If there is a severe impact to the skull, often in the temporoparietal region, with sheer forces that transect the middle meningeal artery, there can be an epidural hematoma, which can be a life-threatening emergency (Fig. 2.3).
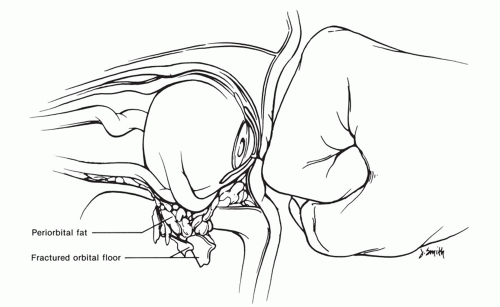
The facial bones are anatomically situated to support the functions of vision, breathing, eating, and smell. Any damage to the facial structures therefore, by definition, can result in loss of functionality and impairment of these sensory modalities. Most notably, the inferior bony wall of the ocular cavity is extremely thin, and direct ocular trauma can result in a “blow out” fracture (Fig. 2.4). This is actually a protective mechanism that can spare the actual globe and helps to prevent blindness. An important anatomic factor regarding the mandible is that it is a U-shaped structure. Given this anatomy, any injuries to the mandible often result in fractures in more than one location.
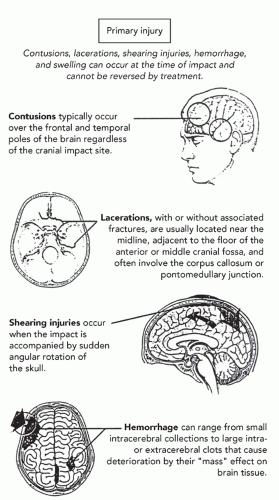 FIG. 2.1. Mechanisms of concussions. Reprinted with permission from McKeag DB, Moller JL. ACSM’s Primary Care Sports Medicine. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2007. |
One important consideration regarding nasal anatomy is that the nasal septum is covered by a vascular web, Kiesselbach’s plexus. Any fractures to the nasal septum can cause disruption of the vascular anatomy and a septal hematoma, which is an urgent condition requiring intervention to avoid nasal septal perforation.
The functional anatomy regarding sports-related ocular trauma is that the eye is a fluid-filled globe sitting in a thinwalled, bony socket. The medial border of the orbital socket is the lacrimal bone and the orbital plate of the ethmoid bone. Superiorly lies the orbital surface of the frontal bone. Laterally is the orbital surface of the zygomatic arch, and inferiorly is the orbital surface of the maxilla as well as a portion of the zygomatic arch. The main structure of this bony architecture is the orbital surface of the maxilla, which is the thinnest of all the surrounding osseous structures and is most likely to fracture during an episode of blunt trauma to the globe. This anatomy is protective in that it allows for a blow-out fracture rather than resulting in globe rupture, which could cause blindness.
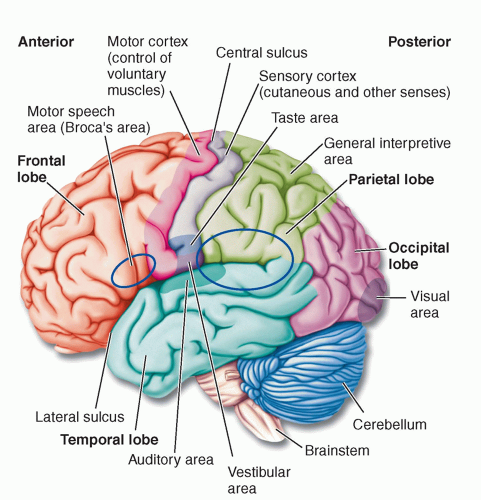 FIG. 2.2. Neuroanatomy and functional anatomy. Reprinted with permission from Bear M, Conner B, Paradiso M. Neuroscience: Exploring the Brain. 2nd ed. Baltimore: Lippincott Williams & Wilkins; 2000. |
The most relevant ocular structures are the eyelids and the cornea. The lids are protective structures, which also have a role in tear production and tear removal through the lacrimal ducts. The lacrimal ducts exit the eye through
the medial portion of both upper and lower eyelids; thus, any resulting injury or laceration to the region of the medial canthus should be thoroughly evaluated to ensure that lacrimal duct injury has not occurred. Injury to the lacrimal ducts that is not properly and promptly repaired by ophthalmology could result in a tear duct problem, eye watering, or dry eyes.
the medial portion of both upper and lower eyelids; thus, any resulting injury or laceration to the region of the medial canthus should be thoroughly evaluated to ensure that lacrimal duct injury has not occurred. Injury to the lacrimal ducts that is not properly and promptly repaired by ophthalmology could result in a tear duct problem, eye watering, or dry eyes.
The cornea is the clear covering over the pupil and iris. It is an important structure in sport as it is commonly injured, usually due to a scratch or an abrasion. It usually heals well, but often needs a protective patch. The deeper structures include the anterior chamber, between the cornea and the lens; the posterior chamber, between the lens and the retina; and the retina itself. The remainder of the structures are all necessary for adequate visual acuity.
EPIDEMIOLOGY
Concussions are most often seen in the 12- to 24-year age range and are more frequently seen in male rather than female athletes. Current incidence data shows that there are 0.14 to 3.66 concussive injuries per 100 player-seasons versus athlete-seasons at the high school level. At the collegiate level, there are 0.5 to 3.0 injuries per 1,000 athlete exposures.6 Approximately 90% or more of concussions do not involve loss of consciousness.2,3
Eye injuries related to sports or recreational activities account for 40,000 to 100,000 injuries annually in the United States, most of which may be preventable.7,8 The highest risk of ocular injuries occurs in sports with sticks, balls, or racquets. In relation to ball sports, smaller balls (e.g., racquetball and handball) present higher risk of ocular injuries. Nonracquet sports that have a higher incidence of ocular trauma include boxing, basketball, and wrestling.
NARROWING THE DIFFERENTIAL DIAGNOSIS
On-field Assessment
The first rule for a head injury is that any athlete who is unconscious after an injury is assumed to have a cervical spine injury, and cervical spine precautions need to be taken with all further evaluation of the athlete until the cervical spine has been evaluated and cleared.
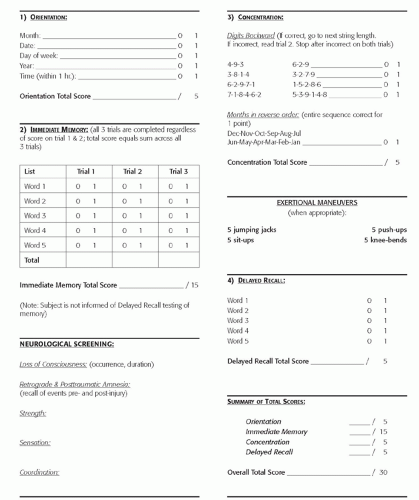
Once an athlete has been determined to be stable, they should be serially evaluated by a trained provider every 10 to 15 minutes. Use of a concussion scale such as the Sideline Assessment of Concussion (SAC) can assist with monitoring subtle changes, either improving or declining performance on any of the cognitive measures (Fig. 2.5).
The safest rule in caring for concussed athletes is that they should not be allowed to return to game play or practice until their symptoms have completely resolved. Additionally, the younger the athlete, the more restrictive the supervising provider should be in allowing them to return to play. Even if symptoms have resolved, it is recommended that athletes at the high school level or younger not return to participation on the day of injury. This recommendation is meant to protect the still-developing brain from further injury or insult.9 If an athlete’s condition is deteriorating rather than improving, especially if their level of consciousness is decreasing or they are starting to have localized neurologic deficits, such as abnormal papillary response, they need to be transported to an emergency medical facility immediately for further evaluation and treatment as they may have an intracranial hemorrhage, specifically an epidural hematoma that would require immediate surgical intervention to avoid increased intracranial pressure, brain stem herniation, and possible death.
Office-based Assessment
Concussed athletes presenting to the office may not realize they sustained a concussion. They may think they just had their “bell rung” or present with headache, dizziness, memory disturbances, or mood changes and not correlate it with head trauma. Furthermore, some symptoms can be delayed in onset and/or worsen as time progresses. The important point is to assess whether these were related to head trauma, and if so, a concussion must be assumed till ruled out. A thorough history of mechanism, symptoms, change in symptoms, as well as any evaluation or treatment done to date is essential. A thorough neurovascular examination with special focus on cognition, memory, and cerebella function is important in the concussed athlete. Any focal neurologic deficit or rapidly progressing symptoms imply potential cranial bleed, and transport to emergency medical facility should occur.
Facial trauma typically presents to the emergency department, but patients may present with minor complaints of double vision (potential orbital blow-out fracture) or tooth malocclusion (occult mandibular fracture) that may indicate more significant facial injuries.
Diagnostic Testing
Laboratory
Appropriate laboratory evaluation depends on the underlying condition but is typically not required with simple concussions or facial injuries.
Imaging
Appropriate imaging can be essential, depending on the suspected underlying condition. Most simple concussions do not require imaging, but complex concussions, presence of focal neurologic deficits, or progression of symptoms may warrant imaging studies. In the emergency department or when there is an acute deterioration of the athlete, emergent computed tomography (CT) is generally the imaging of choice. For postconcussion syndrome, chronic symptoms, or when CT is inconclusive but clinical suspicion remains, a magnetic resonance imaging (MRI) will provide the most accurate imaging of the brain structure for bleeds and cerebral hematomas. An MRI angiogram may be considered if ruling out vascular malformation. Functional MRIs (fMRIs) and positron emission tomography (PET) scans are largely used for research at this time but may prove to be valuable with future research and validation.
X-rays are the initial imaging modality for facial injuries, with CT scan utilized for better visualization when clinically indicated. The extent of many facial fractures may not be evident until CT imaging is performed.
Other Testing
Neuropsychologic testing (traditional or computer based) has been advocated by some for the evaluation of the concussed athlete. Unfortunately, at this time, due to lack of independent validation, expense, and no outcome studies showing improved management of concussions, its use should largely be reserved for complex cases and research. This is the conclusion reached by the most recent 2nd International Conference on Concussion in Sport. Its future role may increase with better independent and outcome-based research, but currently, inappropriate use of neuropsychologic testing has the potential to give a false sense of security to athletes, parents, and medical providers. The gold standard remains management of concussed athletes by a trained physician.
APPROACH TO THE ATHLETE WITH CONCUSSION
The most frequent head injury encountered within athletics is a concussion or MTBI. There have been multiple definitions of concussion, but overall, a concussion is a complex pathophysiologic process affecting the brain and induced by traumatic biomechanical forces.9 As previously discussed, the mechanism of concussion can be due to direct or indirect trauma, or from a whiplash-type injury (Fig. 2.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree