Assistive Technology
Cathy Bodine
HISTORICAL BACKGROUND AND PERSPECTIVE ON ASSISTIVE TECHNOLOGY
Humans have used tools to accomplish everyday tasks in many cultures throughout history (and prehistory), but the perception remains that the use of technology as a tool for persons with disabilities is a fairly recent phenomenon. In fact, James and Thorpe describe any number of assistive devices used as early as the 6th or 7th century B.C. (1). Their descriptions include partial dentures, artificial legs and hands, and drinking tubes or straws. The earliest documented account of optical and lens technologies, or eyeglasses, came from Venice around A.D. 1300 (2). The term assistive technology (AT) to describe devices used to facilitate the accomplishment of everyday tasks by persons with disabilities is actually the more recent development (3).
In 1988, Public law 100-407 defined AT as “Any item, piece of equipment or product system whether acquired commercially off the shelf, modified, or customized that is used to increase or improve functional capabilities of individuals with disabilities.” This definition also included a second component defining AT services as any service that directly assists an individual with a disability in the selection, acquisition, or use of an AT device. This includes
The evaluation of the needs of an individual with a disability, including a functional evaluation of the individual in his or her customary environment;
Purchasing, leasing, or otherwise providing for the acquisition of AT by persons with disabilities;
Selecting, designing, fitting, customizing, adapting, applying, retaining, repairing, or replacing AT devices;
Coordinating and using other therapies, interventions, or services with AT devices, such as those associated with existing education and rehabilitation plans and programs;
Training or technical assistance for the person with a disability or, if appropriate, his or her family;
Training or technical assistance for professionals (including individuals providing education or rehabilitation services), employers, or other individuals who provide services to, employ, or are otherwise substantially involved in the major life functions of children with disabilities (4).
This definition has also been included in other federal legislation authorizing services or supports for persons with disabilities, including the Rehabilitation Act (5) and the Individuals with Disabilities Act (6).
So what is AT? In short, AT is a tool used by someone with a disability to perform everyday tasks such as getting dressed, moving around, or controlling his or her environment, learning, working, or engaging in recreational activities. As a tool, AT is no different than using a hammer to drive a nail. Fewer than 30 years ago, there were fewer than 100 devices commercially available. Today, more than 29,000 assistive devices are listed on the AbleData Web site (www.abledata.com). AT use often begins shortly after birth and continues throughout the life span of individuals with disabilities.
Included within this textbook are chapters on wheelchairs and other mobility aids, recreational therapies, orthotics and prosthetics, and many other rehabilitation devices or tools. The devices described by the authors of these chapters also fall within the definition of AT. This chapter covers basic information on various categories of AT products, evaluation, prescription and funding for AT, use of a team approach, and outcomes measurement in the field of AT devices and services. Readers are referred to the appropriate chapter for more in-depth information on those devices covered elsewhere in the textbook.
AT tends to be divided into two major categories: low technology and high technology. Low-technology or “lowtech” devices tend to be simple, nonelectronic devices. Items such as dressing aids, pencil grips, picture-based communication boards for persons who are nonspeaking, and magnifiers for persons with visual impairments fall within the category of low-tech devices. High-technology or “high-tech” devices are typically described as sophisticated, electronic devices such as power wheelchairs, computers, or augmentative and alternative communication (AAC) devices that provide voice output for persons who are nonspeaking. These devices are usually fairly expensive and often require extensive training to ensure they are used to their fullest potential (7).
There are a number of myths surrounding the provision of AT that tend to reflect common misperceptions about both the technology and individuals with disabilities. These myths include
AT is the “be all and end all.”
AT is complicated and expensive.
Persons with the same disability benefit from the same devices.
Professionals are the best source of information for AT.
AT descriptions are always accurate and helpful.
A user’s AT requirements need to be assessed just once.
AT devices will always be used.
Individuals with disabilities want the latest, most expensive device.
AT is a luxury.
Only people with certain types of disabilities find AT useful.
Although AT does hold a great deal of promise for persons with disabilities who would like to pursue everyday tasks that most of us take for granted, myths such as these have a tendency to cause practitioners and those they serve to disregard the potential utility of assistive devices. Tasks such as navigating freely throughout the community, talking with a loved one, and writing a letter are often out of reach for persons with disabilities. Proper prescription of assistive technologies can enable persons with disabilities to learn, work, and play, just like everyone else. Dispelling these myths can do much to ensure that those who can benefit from assistive devices and services receive appropriate supports.
AT AND ABANDONMENT
It is important to recognize that not everyone with a disability enjoys using technology, however useful it might appear to practitioners. Depending on the type of technology, nonuse or abandonment can be as low as 8% or as high as 75%. On average, one third of more optional ATs are abandoned, most within the first 3 months after acquiring the device. To date, research has not been done to ascertain the number of individuals who must continue to use devices they are not pleased with simply because they cannot abandon the technology without severe consequences (8,9). For example, an individual who has just received a new wheelchair that does not meet expectations simply cannot stop using the chair to navigate independently within his or her community. Rather, he or she must wait until third-party funding becomes available again (often as long as 3 to 6 years) or engage in potentially difficult and unproductive discussions with the vendor who has more than likely provided the chair as it was prescribed by the assessment team.
Research does tell us the number one reason individuals with disabilities choose not to use assistive devices is because practitioners failed to consider their opinions and preferences during the device selection process. In other words, the person with a disability was not included as an active member of the team during the evaluation process (8).
HUMAN FACTORS AND AT
A growing body of research in the field of human factors is being applied to the design and development of AT devices for persons with disabilities. Analysis of human factors in a global sense is concerned with how humans interact with various technologies. When you sit in a new car and notice how comfortable it is—how well the seat contours with your body and how accessible the controls are for the stereo system— you have experienced the growing information derived from human factors research.
Dr. King (10), a professor at the University of Wisconsin-Eau Claire, has expanded key points found in the literature on human factors and applied them to research and development in AT. He tells us that human factors in AT must be concerned with how human beings who have special needs, limitations, or disabilities interact with devices and tools that may support, supplement, or replace some process or ability that has been lost or impaired by illness or injury. We must be concerned not only with how the user interacts with the devices but also with how the family or other close care providers react to the use of tools and devices in their settings. The interaction of the AT user alone with the technology does not tell us the whole story because persons who use assistive technologies must interact closely and frequently with, or depend on others, for daily care and other aspects of their lives. The larger impact on those around the user must also be considered because they are key players in the implementation of any AT in the user’s life. Across all component areas of AT, human factors must be concerned with how the potential user—as well as his or her family, personal care providers, education and therapy aides, teachers, and clinicians—interacts with the assistive devices and technological systems.
Analysis of human factors in AT is concerned with finding out the special needs, capabilities, and limitations of users and then matching devices and controls to each individual user. Heterogeneity and individualization are primary considerations in dealing with persons who have special needs. However, mass-produced technologies (such as computers) must be designed for mass-market users, rather than for unique individuals. Flexibility and adaptability of technology to a wide range of user characteristics are critically important.
Human factors considerations in AT are especially focused on reducing the user’s exertion, stress, and fear of use. We all have a bit of “technophobia” when it comes to use of new tools and devices—especially complex, high-tech devices. The fear and stress, particularly when they relate to devices that may be difficult to set up or require a great deal of exertion to use, can be deleterious to the AT user. Persons relying on AT have some type of limitation or disability. Expecting an individual with a disability to become skilled in additional tools, devices, or technology can be highly stressful to users as well as caregivers because it adds more complexity to their life.
Human factors also focus on reducing the danger caused by the device to the user and persons around them. AT professionals should also strive to reduce the possibility of failure during use, which can lead to rejection or abandonment of the device for future use, even when the system has considerable merit for the person with a disability (10).
AT AND THE INTERNATIONAL CLASSIFICATION OF FUNCTIONING, DISABILITY, AND HEALTH
Disability itself is not precise and quantifiable. The concept of disability is not always agreed on by persons who self-identify as having a disability, persons who study disability, or the general public (11). This lack of agreement creates obstacles for studies focused on disability and to the equitable and effective administration of programs and policies intended for persons with disabilities. To facilitate agreement about the concept of disability, the World Health Organization (WHO) has developed a global common health language—one that is understood to include physical, mental, and social well-being. The WHO first published the International Classification of Impairment, Disabilities, and Handicaps (ICIDH) in 1980 as a tool for classification of the “consequences of disease.”
The newest version, International Classification of Functioning, Disability and Health, known as ICF (2001), moves away from a “consequences of diseases” classification (1980 version) to a “components of health” classification. This latest model is designed to provide a common framework and language for the description of health domains and health-related domains. Using the common language of the ICF can help health care professionals to communicate the need for health care and related services, such as the provision of AT for persons with disabilities (12).
In the context of health, the following language is used:
Body functions are the physiologic and psychological functions of body systems.
Body structures are anatomic parts of the body, such as organs, limbs, and their components.
Impairments are problems in body function or structure, such as significant deviation or loss.
Activity is the execution of a task or action by an individual.
Participation is involvement in a life situation.
Activity limitations are difficulties an individual may have in executing activities.
Participation restrictions are problems an individual may experience in involvement in life situations.
Environmental factors make up the physical, social, and attitudinal environments in which people live and conduct their lives (12).
Application of the WHO global common health language makes possible the definition of the need for health care and related services; defines health outcomes in terms of body, person, and social functioning; provides a common framework for research, clinical work, and social policy; ensures the cost-effective provision and management of health care and related services; and characterizes physical, mental, social, economic, or environmental interventions that will improve lives and levels of functioning. Provision of AT for persons with disabilities is an intervention that has the potential to diminish activity limitations and participation restrictions and in turn, improve the quality of life of individuals with disabilities. Throughout this chapter, the use of the WHO common health language is used to discuss the potential impact of AT.
AT FOR MOBILITY IMPAIRMENTS
Individuals with mobility impairments often present with unique needs and abilities. Some may demonstrate only lower-body impairment, such as a spinal cord injury or spina bifida, with no other complications. AT solutions might include crutches, a scooter, or a wheelchair. Simple modifications or adaptations to the environment, such as removing physical barriers to access (wide doorway or a ramp instead of stairs), may be all that is needed. For others, automobile hand controls, adapted saddles for horseback riding, sit skis for downhill skiing, or even placing bricks under a desk or table to allow the wheelchair user to work comfortably at a workstation may be necessary accommodations.
Other adaptive equipment for persons with mobility impairments might include a van with an attached lift. Many individuals who use wheelchairs drive a wide range of motor vehicles as well as bicycles using specially customized hand controls for turning and braking (Fig. 73-1). Chapter 78, Wheelchairs, and Chapter 76, Lower Extremity Orthotics, Shoes and Gait Aids, provide in-depth discussions of a wide range of assistive technologies for persons with mobility impairments that interfere with ambulation and other activities of daily living (ADLs).
For someone with upper-body mobility impairment, such as poor hand control or paralysis, assistive devices might include alternate keyboards or other input methods to access a computer. Alternate keyboards come in many shapes and sizes. There are expanded keyboards, such as the Intellikeys (Fig. 73-2), which provides a larger surface area than a standard keyboard, larger letters with a contrasting yellow background, and options such as a delayed response of the activated key for individuals who have difficulty either initiating touch or removing their finger after they have activated the key. For individuals who have never used a standard QWERTY keyboard layout, letters on the keyboard can be arranged alphabetically. This key arrangement is often helpful for young children who are developing literacy skills, as well as for adults who have cognitive or visual impairments that necessitate additional supports for reading and writing.
 FIGURE 73-1. AT for mobility impairments. (Courtesy of Marlin Cohrs, Assistive Technology Partners, Department of Rehabilitation Medicine, University of Colorado Health Sciences Center.) |
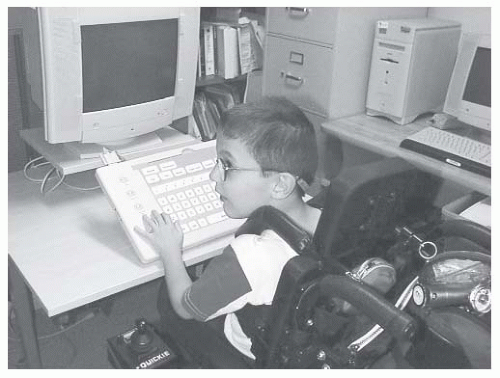 FIGURE 73-2. Intellikeys keyboard. (Courtesy of Jim Sandstrum, Assistive Technology Partners, Department of Rehabilitation Medicine, University of Colorado Health Sciences Center.) |
There are also small keyboards, such as the Tash Mini Keyboard (Fig. 73-3), that are designed in what is called a “frequency of occurrence” layout. Individuals who are one-handed typists, or who use a head stick or mouth stick to type, frequently prefer a smaller-sized keyboard. The home row (middle row) consists of the most frequently occurring letters in the English alphabet, with the letters a, e, and the space bar placed in the center of the keyboard for easy access. Characters, numbers, and functions (including mouse control) keys fan out from the center of the keyboard depending on how frequently they are used by the average typist.
 FIGURE 73-3. Tash Mini keyboard. (Courtesy of Marlin Cohrs, Assistive Technology Partners, Department of Rehabilitation Medicine, University of Colorado Health Sciences Center.) |
For individuals who are unable to use any type of keyboard or other device that requires hand mobility or finger pointing, there are a wide range of switches available that provide access not only to the computer but also to battery-operated electric toys and home-based or work appliances. These switches may be as simple as a “rocking lever” switch (Fig. 73-4) designed to be activated through a gross motor movement that involves touching or hitting the switch with the head, hand, arm, leg, or knee. Other switches can be activated by tongue touch, sipping and puffing on a straw, or through very fine movements, such as an eye blink or a single muscle twitch.
Fairly recent developments include eye gaze switches that calibrate intentional eye movement patterns and select targets such as individual keys on an on-screen keyboard, and also brain wave technology (Eye and Muscle Operated Switch or EMOS) that responds to the excitation of alpha waves to trigger the selection. Other input methods for the computer include devices such as the Head Mouse and Tracker 2000. These devices also rely on an on-screen keyboard visible on the computer monitor. The user wears a reflective dot on his or her forehead or other head-mounted signaling device to tell the computer what key or command he or she wishes to activate. With these and many other high-tech control devices, individuals with disabilities, even those with the most severe motor impairments, can monitor and control an unlimited array of home, work, and school activities.
There are thousands of lower-tech assistive devices available for persons with motor impairments. Commonly referred to as aids for daily living, these devices include such things as weighted spoons, scoop plates, and other devices used to
facilitate eating (Fig. 73-5); aids for personal hygiene, such as bath chairs and long-handled hairbrushes; adapted toys for play; built-up pencil grips for writing and drawing tasks; items for dressing, such as sock aids and one-handed buttoners; and many others. Prices and availability cover a wide range for items such as these. Many low-tech mobility aids can be handmade for just a few dollars, whereas others, such as an adult bath chair, may cost several hundred dollars. All share the common goal or utility of reducing activity limitations and increasing participation in daily life activities.
facilitate eating (Fig. 73-5); aids for personal hygiene, such as bath chairs and long-handled hairbrushes; adapted toys for play; built-up pencil grips for writing and drawing tasks; items for dressing, such as sock aids and one-handed buttoners; and many others. Prices and availability cover a wide range for items such as these. Many low-tech mobility aids can be handmade for just a few dollars, whereas others, such as an adult bath chair, may cost several hundred dollars. All share the common goal or utility of reducing activity limitations and increasing participation in daily life activities.
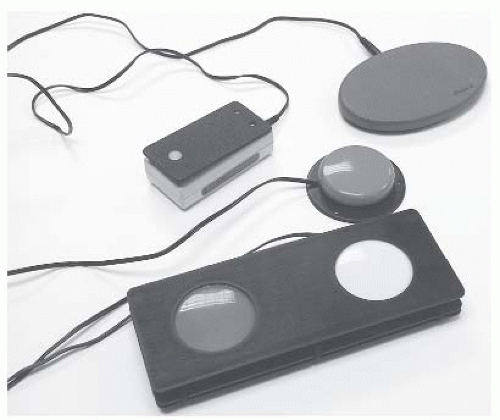 FIGURE 73-4. Switches. (Courtesy of Marlin Cohrs, Assistive Technology Partners, Department of Rehabilitation Medicine, University of Colorado Health Sciences Center.) |
AT FOR COMMUNICATION DISORDERS
For individuals with severe expressive communication impairments, there is a wide range of AT devices available. For persons who have reduced phonation or breath support and speak very quietly, there are a number of portable amplification systems available that work much like a sound system in a large lecture hall. There is also a device available that clarifies speech for individuals with dysarthria. Called the Speech Enhancer, it consists of a headset attached to a portable device and is worn much like a shoulder bag (Fig. 73-6). The individual using this system speaks into the microphone, and the sound is processed and then projected by speakers attached to the unit. Although not for everyone, this device has proven effective for a number of individuals struggling to be understood when communicating with medical personnel, family members, and others in the community.
For individuals who are unable to talk at all or who have such severe expressive communication difficulties that only their most intimate associates understand them, there are a wide range of AAC systems available. These devices range from very simple picture books to high-end sophisticated electronic communication devices with digitally recorded or synthetic speech output. Children and adults with severe expressive communication impairments can benefit academically, vocationally, emotionally, and socially from the provision of a device that allows them to communicate their thoughts, learn and share information and ideas, and otherwise participate in life activities.
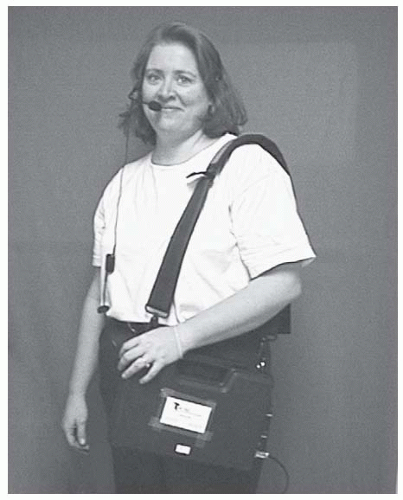 FIGURE 73-6. Speech enhancer. (Courtesy of Marlin Cohrs, Assistive Technology Partners, Department of Rehabilitation Medicine, University of Colorado Health Sciences Center.) |
It is important to note these AAC devices, although extremely useful and important to the lifestyles of many individuals who are nonspeaking, do not replace natural speech. Instead they augment or provide an alternate form of communication. Other communicative modalities, such as vocalizations, gestures, sign language systems, eye gaze, etc., remain valid and acceptable forms of communication and should be encouraged to develop along with the facility to communicate out loud using an AAC device.
Congenital conditions such as autism, cerebral palsy, mental retardation, developmental verbal apraxia, and developmental language disorders can result in severe expressive communication impairments, necessitating the need for AAC interventions (13). Acquired disorders for which AAC is often used include traumatic brain injury, stroke, amyotrophic lateral sclerosis (ALS), tetraplegia, multiple sclerosis (MS), and laryngectomy that is due to cancer (7,14). Augmentative communication systems (Fig. 73-7) have also been used successfully for individuals who are temporarily nonspeaking as a result of ventilator dependence (15).
There are two common myths surrounding the use of AAC. The first is that individuals who are nonspeaking must demonstrate certain developmental prerequisites before the
prescription of an AAC device. On the contrary, there are no strict sets of cognitive or physical prerequisites to the use of AAC devices. Specific AAC techniques that match the individual’s needs and abilities are chosen on the basis of a comprehensive evaluation by a qualified team of clinicians, family members, teachers, and others. The second myth is that the use of an AAC device will stifle or preclude the development or return of natural speech. However, the research tells us that use of an AAC device can actually support improved speech production and it in no way creates barriers to the development or return of natural speech (16).
prescription of an AAC device. On the contrary, there are no strict sets of cognitive or physical prerequisites to the use of AAC devices. Specific AAC techniques that match the individual’s needs and abilities are chosen on the basis of a comprehensive evaluation by a qualified team of clinicians, family members, teachers, and others. The second myth is that the use of an AAC device will stifle or preclude the development or return of natural speech. However, the research tells us that use of an AAC device can actually support improved speech production and it in no way creates barriers to the development or return of natural speech (16).
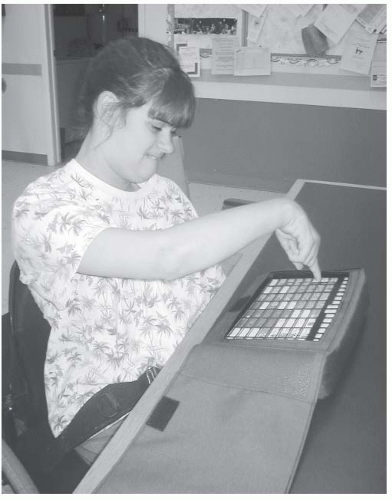 FIGURE 73-7. Using an AAC device. (Courtesy of Jim Sandstrum, Assistive Technology Partners, Department of Rehabilitation Medicine, University of Colorado Health Sciences Center.) |
Low-tech picture and alphabet boards are often used as either a preliminary step before purchasing an electronic voice output system, or as backup systems, should an electronic device break or its use not be convenient (e.g., during swim lessons). These low-tech systems (Fig. 73-8) can be made from picture library software available through commercial vendors (BoardMaker, PCS Symbols) or can be handmade using digital photographs, pictures from catalogs or books, or by simply using a marker to write or draw letters, words, phrases, or pictures. Adults with progressive diseases such as ALS or MS frequently use low-tech picture or alphabet boards to clarify their meaning as communication abilities decrease or as they fatigue during the day.
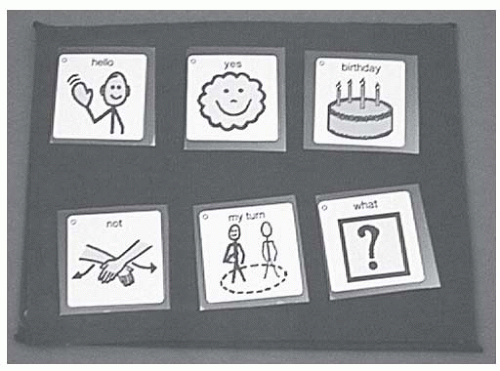 FIGURE 73-8. Low-tech AAC device. (Courtesy of Marlin Cohrs, Assistive Technology Partners, Department of Rehabilitation Medicine, University of Colorado Health Sciences Center.) |
There are a number of low-tech voice output AAC devices available that are simple to program and use. The Talking Symbol Notepad, GoTalk, and TechTalk8 communication devices all use digital speech output (Fig. 73-9). Digital speech devices work much like a tape recorder. The person
setting up the device simply holds down a button and records live voice into the microphone. The speech is digitized or recorded within the device. When the end user chooses to speak, he or she simply presses to activate the device. It then speaks the prerecorded message. The good news is these devices are simple and fairly inexpensive to purchase. It is important to bear in mind, however, that they are intentionally designed to communicate quick, simple messages, such as “hi,” “let’s play,” or “leave me alone.” These devices are not appropriate for individuals who have more than a few things to say or who have the ability to generate complex thoughts and feelings.
setting up the device simply holds down a button and records live voice into the microphone. The speech is digitized or recorded within the device. When the end user chooses to speak, he or she simply presses to activate the device. It then speaks the prerecorded message. The good news is these devices are simple and fairly inexpensive to purchase. It is important to bear in mind, however, that they are intentionally designed to communicate quick, simple messages, such as “hi,” “let’s play,” or “leave me alone.” These devices are not appropriate for individuals who have more than a few things to say or who have the ability to generate complex thoughts and feelings.
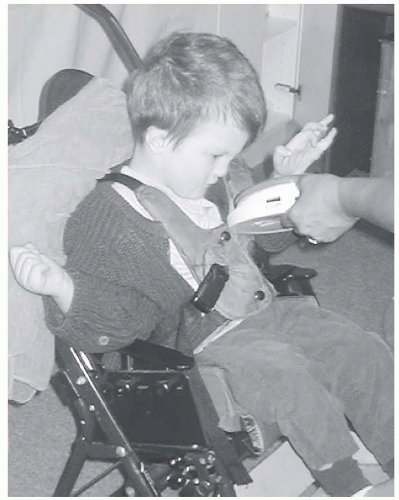 FIGURE 73-9. Using the Big Mac. (Courtesy of Diane Brians, Assistive Technology Partners, Department of Rehabilitation Medicine, University of Colorado Health Sciences Center.) |
There are a number of more sophisticated digital devices available as well. These include the DynavoxM3, Chatbox40 (Fig. 73-10), Springboard, and others. These devices have the capacity to encode several minutes of live voice and are often used by individuals who are not yet literate, have developmental disabilities, or simply wish to have a simpler device to use when going to the store or out to eat.
At the high end of AAC systems are the synthesized speech devices (Fig. 73-11). These voice output systems use built-in speech synthesis to speak messages that have been typed and previously stored into the device. They are capable of encoding several thousand words, phrases, and sentences. AAC devices such as these are frequently designed to provide an alternate access to the computer and control appliances such as TVs, door openers, and other electrical items found in many environments. Four popular text-to-speech devices are the ECO-14, LightWriter (Fig. 73-12), Tango, and the VMax. It is important to note that these AAC systems can cost thousands of dollars. But more importantly, they also form a critical link to the world for individuals with severe expressive communication impairments.
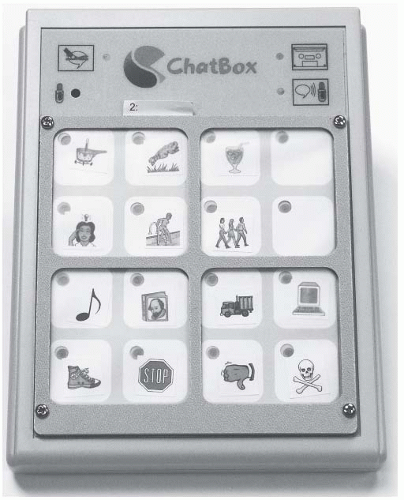 FIGURE 73-10. The Chatbox. (Courtesy of David Hershberger, Saltillo Corporation, Millersburg, Ohio.) |
 FIGURE 73-11. The Vantage Communication Device. (Courtesy of Barry Romich, Prentke Romich Company, Wooster, Ohio.) |
All of the AAC devices on the market can be activated through direct selection using either a finger or other pointing device, such as a head or mouth stick. A large number of the digital and text-to-speech devices can be activated using either direct selection or an alternate input mode. Alternate input includes all of the switches described above, as well as other additional infrared and wireless switches currently on the market. When an individual with a severe motor impairment and severe expressive communication impairment chooses to
use a switch to access the AAC device, the device can be preset to scan.
use a switch to access the AAC device, the device can be preset to scan.
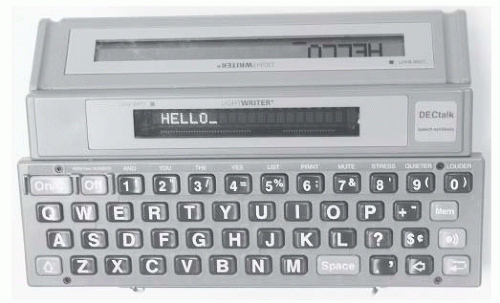 FIGURE 73-12. Using the LightWriter. (Courtesy of Marlin Cohrs, Assistive Technology Partners, Department of Rehabilitation Medicine, University of Colorado Health Sciences Center.) |
The most commonly used switch access method is called row column scanning. In this method, the end user starts by activating a switch to begin the scan. When the correct row is highlighted, he/she hits the switch again to start the lights scanning across the row (hence column). When the correct button is highlighted, the user hits the switch again to activate the chosen button. As can be surmised, using a scanning system to activate an AAC device can be a slow and tedious process. For many individuals, however, this method provides the only available access to spoken and written communication, and for those select persons it is highly prized as a window to the world.
One of the more vigorous debates within the field of AAC centers around the encoding or mapping strategies used to represent language on a communication device. Currently available systems vary greatly in vocabulary storage and retrieval methods, but all systems are based on communication symbols, whether orthographic or pictographic. Symbols vary in their transparency (guessability) and translucency (learnability). In order to select a set of symbols for an individual’s communication system, it is important to match these factors with the individual’s cognitive and perceptual abilities.
Additionally, the world of technology moves at a very rapid pace. AAC devices currently on the market have been designed using today’s technologies. As more and more innovations become available, such as cell phones, text messaging, and wireless global positioning systems (GPS), the capabilities and flexibility of these devices will change. As with all technologies, it is important that clinicians and practitioners remain current on these and future technology developments.
AT FOR VISUAL IMPAIRMENTS, INCLUDING BLINDNESS
The term visual impairment




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








