CHAPTER 15 Assessment of the sports patient
Introduction
With increasing numbers of people undertaking regular exercise there has been a corresponding rise in the number of sports injuries. In 1991 it was estimated that there were 5 million cases of exercise-related morbidity in the UK (Nicholl et al 1991). This equates to 1 in 10 people sustaining one injury each year. With the profile of sport in society increasing, and the incentive of high salaries for professional sports men and women, it is likely that the incidence of injury is now even greater among the general population. Podiatry has a significant part to play in the management of sports injuries, as the majority of these injuries occur in the lower limb. The commonest acute injury is the ankle sprain (Colville 1998, Ferran & Maffulli 2006); the commonest tendon injury is to the Achilles tendon (Jarvinen et al 2005, Marks 1999) and the most frequently seen joint pathology is patellofemoral syndrome (Tallay et al 2004, Walsh 1994). Podiatric intervention is often an integral component in the successful management of these and other lower-limb injuries.
Guiding principles
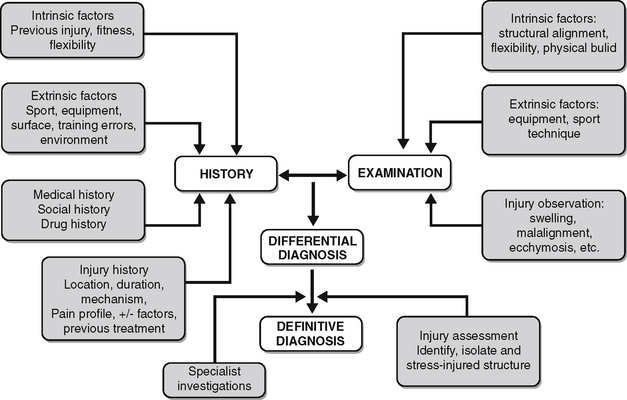
The history and examination should be aimed at both diagnosing the injury and determining the presence or absence of intrinsic (personal) and extrinsic (environmental) risk factors associated with the injury. The identification of intrinsic and extrinsic risk factors can assist in making the diagnosis and guiding the management plan. It is important to gain as much information as possible about the injury. Information on the duration, nature, frequency and intensity of symptoms must be gained along with details of the injury mechanism, aggravating factors and previous treatment.
Clinical examination of the patient, which should include the whole musculoskeletal system, with a specific focus on the lower limbs and the injury site, should follow the standard examination protocol of observation, palpation and movement (see Ch. 10). When turning to the injury site it is imperative to know the anatomical structures of the region to make an accurate diagnosis. After observing the area for inflammation, erythema, ecchymosis, structural defects and malalignment the practitioner should physically examine the area. The purpose of the physical examination is to identify, isolate and then stress individual anatomical structures to try to reproduce the patient’s symptoms. This should help enable the practitioner to identify whether the pathology is isolated to a specific tendon, ligament, bone, joint, muscle or nerve. A summary of the assessment process is given in Figure 15.1.
Role of the sports podiatrist
The podiatrist may be part of an interdisciplinary sports medicine team, a multidisciplinary sports medicine team or working as a sole practitioner. Central members of a sports medicine team are likely to include a sports physician, orthopaedic surgeon, physiotherapist and podiatrist. Other members of the team may include a general practitioner (GP), radiologist, osteopath, chiropractor, podiatric surgeon, masseur and professionals from the sports science disciplines such as an exercise physiologist, sports psychologist and nutritionist. Working in such a team is of obvious benefit to both practitioner and patient. The patient is likely to be treated more holistically, with appropriate intervention more readily available. For the practitioner there should be assistance in making an accurate diagnosis and being able to treat more of the aetiological factors of the injury (Case history 15.1).
15.1 Case history
A 19-year-old female, elite cross-country runner with pain in her medial longitudinal arch was referred, by her coach, to a multidisciplinary sports medicine team. The pain had been present for 4 weeks and was gradually getting worse. The pain was centred around the navicular and the insertion of the posterior tibialis tendon was both prominent and painful. Base line X-rays were negative for a navicular stress fracture but demonstrated a type 2 os tibialis externum. A magnetic resonance imaging (MRI) scan was requested to examine the health of the tibialis posterior tendon and determine the presence of a stress fracture. The scan confirmed a navicular stress fracture and healthy tendon. She was treated with a short leg cast for 6 weeks followed by prophylactic orthoses to reduce pronatory compression forces on the navicular. She was also identified as being oligomenorrhoeic with only four menstrual cycles per year. This is known to be a risk factor for stress fractures (Tomten et al 1998). She was subsequently referred for dual energy X-ray absorptiometry (DEXA) scanning of her pelvis, spine and foot, which demonstrated reduced bone mineral density. She was therefore referred to a gynaecologist and sports nutritionist to address these imbalances. Three years on she is still competing at an elite level and has had no further stress fractures.
Working as a sole practitioner is often more challenging. Assistance in making an accurate diagnosis through interdisciplinary discussion or access to specialist investigations such as magnetic resonance imaging (MRI), bone scans and intracompartmental pressure tests may not be available. It is important to develop a referral network with other healthcare practitioners to overcome these potential shortcomings and to be able to offer the patient more beneficial treatment plans. If such a network does not exist the practitioner may be required to provide treatment and advice using mechanical, physical and pharmacological modalities as well as giving advice on appropriate training schedules. Although this may not affect the treatment outcome, a practitioner must be aware of their limitations and refer to other practitioners where necessary.
Assessment environment
Gait analysis equipment can be of great benefit in assessing the sports patient. The most commonly used equipment is a treadmill, with or without the use of a video camera. More specialist equipment such as force platforms, in-shoe pressure systems and digitised video gait analysis are discussed in detail in Chapter 11. Specialist equipment can be useful when assessing more complex sports injury cases or when treating professional athletes. These systems can:
Injury risk factors
The aetiology of both acute and chronic injuries is undoubtedly multifactorial. To simplify this process, risk factors are divided into intrinsic and extrinsic causes. Intrinsic risk factors are those that are personal and are either biological or psychosocial characteristics that predispose the individual to injury. Intrinsic risk factors account for up to 40–60% of all running injuries (Cavanagh & Kram 1990, James et al 1978). Extrinsic risk factors are independent of the person and are related to the type of sporting activity and the sporting environment. Extrinsic risk factors account for up to 80% of running injuries (McKenzie et al 1985). In the vast majority of chronic overuse injuries it is a combination of both intrinsic and extrinsic risk factors that have led to the condition (Kannus 1997). Of all risk factors for overuse injuries training errors are the most common and may be the decisive factor in 60% of the cases (Hreljac et al 2000). Table 15.1 lists the intrinsic and extrinsic risk factors for injury.
Table 15.1 Intrinsic and extrinsic risk factors associated with sports injuries
| Intrinsic risk factors | Extrinsic risk factors |
|---|---|
| Age | Sporting equipment |
| Gender | Exercise surface |
| Previous injury | Sporting activity |
| Structural alignment | Sport position |
| Flexibility | Training errors |
| Physical fitness | Warm up and stretching |
| Physical build | Environmental factors |
| Psychological factors | |
| Systemic disease |
Intrinsic risk factors
Age
The age of an athlete can affect both the type of injury that may occur and the healing mechanisms that follow. Younger and older athletes tend to be more injury prone for a variety of reasons. There is generally less muscle mass and muscle strength in both of these groups compared with older adolescents and young adults. This can result in greater injury risk both in contact and endurance sports. Less protective sports equipment is available for children than adults, which can lead to greater injury risk from ground reaction forces and physical contact. The quality of coaches in children’s teams is often lower than their adult counterparts, which may cause injury due to improper training and coaching supervision (Dalton 1992). Some studies have found that 70% of all sports injuries occur in children under 18 years (Hergenroeder 1998).
In children of all ages fractures are more common than ligamentous disruptions. Even the location of fractures varies with the age of the child. Adolescents tend to have fractures in the physeal areas, whereas preadolescents have more fractures in the diaphysis (Cantu & Micheli 1991). Certain bony injuries, such as the osteochondritides, can only occur in the young athlete. Also traction apophysitis of the calcaneus (Sever’s disease), the fifth metatarsal (Iselin’s disease), and of the tibial tubercle (Osgood–Schlatter’s disease) only occur in children and adolescents, although rarely the symptoms may persist into adulthood in the case of Osgood–Schlatter’s disease. Both traction apophysitis in the young athlete and musculotendinous injuries in the older athlete have been linked with reduced flexibility. It is known that reduced flexibility is more common in both groups (Anderson & Burke 1994, Gerrard 1993). Assessment of flexibility is therefore a key area when examining both children and older athletes with sports injuries.
Musculotendinous injuries are the commonest injury in the older athlete (over 40 years). This is due to a number of cellular changes which occur with increasing age. Changes in collagen cross-linking cause an increase in tendon stiffness and reduce the elasticity of the tendon. Similar change have also been seen in ligaments. This can result in a muscle being subject to earlier and prolonged loading in a movement cycle and being unable to undergo normal stretching, resulting in damage to the musculotendinous unit. The diameter, density and cellularity of the collagen fibrils are also diminished with advancing age, which results in reduced muscle mass and strength. Finally, the blood supply to tendons reduces with age, resulting in an increased risk of tendonitis, tendinosis or rupture (Sassmannshausen 2006, Strocchi et al 1991).
Overuse injuries in the older athlete may also develop due to a delayed physiological response to exercise. When a person starts an exercise programme there are gradual positive changes to the cardiovascular, neurological, endocrine and musculoskeletal systems. As a person becomes fitter the muscles become stronger and there is an increase in bone density. These normal adaptive changes are delayed in the older athlete and may cause musculotendinous injuries if the athlete increases their training volume too quickly. Older males are almost twice as likely to develop a sports injury as older females (Gerson & Stevens 2004).
Gender
Physiological differences between the sexes result in differences in athletic performance. For comparative body sizes women have a reduced cardiac output, blood volume, vital capacity and mean muscle mass when compared with males. Whether this increases the risk of injury in female athletes is uncertain. Studies involving civilian populations have not shown significant differences in injury rates between the sexes (Hootman et al 2002, Knowles et al 2006), except in children, where boys are twice as likely to be injured as girls (Bruns & Maffulli 2000). McQuillan & Campbell (2006) attributed this to football and found that if football was excluded from the analysis the rates of injury were the same for boys and girls. This is in contrast to studies involving military personnel in which injury rates among female recruits are between two and four times higher than among their male counterparts (Jones et al 1988, Ross & Woodward 1994, Yates & White 2004).
The incidence of stress fractures has also been reported to be higher in females. Early studies showed the female incidence to be 10 times greater than men (Protzman & Griffis 1977). Although more recent studies have not shown such a significant difference between the sexes it is generally accepted that female athletes are more prone to stress fracture than males, especially in the military. There are three common aetiological factors which may be responsible for this greater relative risk of stress fracture. These interlinking factors are known as the female athlete triad or unhappy triad and usually present as a combination of:
• amenorrhoea or menstrual irregularities (less than five menses per year)
• osteoporosis (due to menstrual abnormalities, hormonal imbalance, calcium deficiency or malnutrition)
• eating disorders (anorexia nervosa, bulimia nervosa, binge-eating disorders, anorexia athletica).
Although any of these factors can be present in the non-athletic female population, both amenorrhoea and eating disorders are more common among athletes. Some prospective studies have also demonstrated that stress fractures occurred more frequently in female athletes with low bone density (Bennell et al 1996) and also those with menstrual irregularities (Brukner & Bennell 2001, Rauh et al 2006).
It is generally agreed that females are more flexible than males. Whether this should affect injury rates between the sexes is unclear, but it has been reported that greater flexibility may predispose ligament injuries whereas inflexibility may predispose musculotendinous injuries. This would result in females being more prone to ligament injuries and males to musculotendinous injuries. Some evidence would appear to support this theory, as both anterior cruciate knee ligament injuries and lateral collateral ankle ligament injuries have been reported to be higher in females than in males undertaking the same activity (Almeida et al 1999, Griffin 1994) while Achilles tendon injuries are more common in males (Kannus & Jozsa 1991).
Previous injury
The subsequent injury does not necessarily occur at the same location as the previous injury. This may suggest compensatory changes have occurred due to the injury or its treatment. These changes may be in proprioception or neuromuscular coordination resulting in excessive strain on adjacent or distant structures (Case history 15.2).
Structural alignment
Structural alignment should be assessed with the patient non-weightbearing, weightbearing and dynamically. A thorough examination in all three components is essential if the practitioner is to gain a complete picture of the athlete’s structure and function as it relates to the injury. This assessment should include examination of the joints, muscles and osseous alignment (Ch. 10, section A). The majority of podiatric interventions in sports injuries are related to the assessment and treatment of structural alignment and function that has caused or contributed to the injury.
• Normal structure and function but inadequate preparation or excessive demands placed on the tissues
• Abnormal structure and function with relatively normal demands placed on the tissues.
• running 160 km/week will often result in injury
• a running volume of 160 km/week in just 6 months has not allowed the tissues to undergo the normal adaptive processes required to meet these demands
• running every day does not allow adequate recovery time for the tissues, resulting in injury.
• muscle inflexibility (hamstrings, iliotibial band, quadriceps, lateral retinacula of the knee and calf muscles)
• muscle weakness (vastus medialis, gluteus medius, medial retinacula of the knee)
• patella malalignment or hypermobility (in frontal, transverse or sagittal plane)
• patella maltracking (during flexion and extension)
• excessive subtalar joint pronation
The presence or absence of these factors should assist the practitioner in identifying the aetiological factors and planning the most effective treatment (Witvrouw et al 2000).
Asymmetries between limbs may represent the obvious cause of a unilateral overuse injury. However, it is important to consider the role of other factors such as the type of activity, exercise surface, unilateral trauma and injury history. Any of these factors may cause a unilateral injury. If structural asymmetry is identified, then the practitioner must determine a biomechanical mechanism by which the asymmetry could have caused the overuse injury. If we consider stress fractures as an example, there is a strong association between stress fractures and limb-length inequality (Brukner et al 1999). Stress fractures tend to occur in the longer limb, and the greater the inequality the greater the incidence (Friberg 1982). The reasons for this are thought to be due to the biomechanical consequences of the limb-length difference, which results in a longer stance phase, skeletal realignment, greater osseous torsion and increased muscle activity of the longer limb. However, other studies have not shown any increase in injury risk when a limb-length inequality of >5 mm is present (Goss et al 2006).
Flexibility
Hypermobility due to increased muscle flexibility and ligamentous laxity has been associated with a greater risk of injury. Hypermobility is often determined by the Beighton score, which is based on a nine-point test designed to measure excessive joint movement (Ch. 14). This test has been used in a number of studies on flexibility and injury, which have generally shown that hypermobility is associated with a greater incidence of ligamentous injury. Rossiter & Galbraith (1996) found that hypermobility was present in 34% of military recruits with ankle and knee ligament injuries compared with 19% of control subjects. Increased flexibility, measured by the sit and reach test, in the absence of ligamentous laxity has not been shown to be a significant factor in injury prediction.
Generalised inflexibility due to muscle tightness has been linked to musculotendinous injury: while this is likely to be true, it has only been proved in one long-term prospective study to date (Witvrouw et al 2003). However, if a theoretical causal link can be made between the muscle inflexibility and the injury, then stretching of those muscles should be included in the treatment programme. Likewise, if hypermobility is present, then stretching should be avoided and athletes encouraged to perform specific stabilising exercises.
Stretching prior to activity in an attempt to reduce the risk of lower limb injury is contentious. Some large randomised controlled trials involving military recruits (Pope et al 1998, 2000) have shown no benefit in stretching while others have (Amako et al 2003). In two large systematic reviews of the literature neither set of authors could conclude on any significant benefit of stretching prior to sports participation (Fradkin et al 2006, Thacker et al 2004). This does not mean that injured athletes with muscle inflexibility should not be instructed to stretch, as this is an effective treatment modality. However, athletes are often questioned as to whether they stretch before and after activity and encouraged to do so if they do not. There seems little evidence to support this premise and failure to stretch before exercise should not necessarily be viewed as a risk factor to injury.
Physical fitness
Physical fitness is known to lower the risk of injury, as shown in a number of studies based on military and civilian populations (Neely 1998). This protective mechanism not only applies to practising a known sport but also to learning a new sport or athletic skill. The level of reduced risk varies among the studies, and is dependent upon the activity being undertaken and the fitness test used. Pope et al (2000) were able to demonstrate that the least-fittest group of their army recruits were 14 times more likely to sustain a lower limb injury than the fittest group. The fitness method used was the progressive 20 m shuttle run test, also known as the bleep test. This test is one of the most popular fitness tests used today.
When assessing injured athletes it is important to gauge their fitness level, as you may need to offer advice on a more appropriate training regimen. This is often the case for the novice athlete who enthusiastically embarks on an over-ambitious fitness programme. This will result in injury, as the musculoskeletal system is not prepared for such strenuous exercise. When an injury occurs, the athlete should be advised to modify their exercise regimen to prevent recurrence or further injury to other structures. This advice may include changing the method of exercise or reducing the intensity, frequency or duration of the exercise.
Physical build
The relationship of physical strength to injury is unknown. To avoid injury the musculoskeletal system must be able to cope with the physical demand of the sporting activity. Some evidence suggests that stronger athletes are more injury prone (Knapik et al 1992). The reasons for this are unclear, but it may be that the muscular forces generated by stronger athletes damage their joint structures and even the muscles themselves. It may also be that stronger athletes exercise at greater intensity or duration than weaker athletes, resulting in higher injury rates.
There is a correlation between strength imbalance and injury that is most frequently seen in the knee joint, where differences between hamstring and quadriceps strengths have been associated with cruciate ligament injuries. The role of strength differences between limbs has also shown a greater injury incidence on the weaker side. There is general agreement that strength differences greater than 10% can increase the injury risk to the weaker limb. These injuries may be acute, as with cruciate ligament injuries, or chronic, due to fatigue, for example tendinopathy, muscle strains and stress fractures. The role of limb dominance in injury incidence is less certain. Limb dominance in racket or ball sports is associated with different injury patterns. However, in sports that require equal stresses through both limbs there is no evidence to suggest limb dominance is a risk factor. Herring (1993) did not find any difference in injury incidence based on limb dominance in elite runners.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree