CHAPTER 14 Assessment of the paediatric patient
Normal development
Normal development covers a wide spectrum of values and, although it is age related, there is variation within this as well. Even between healthy siblings there may be what appear significant differences. However, with time it is probable that such differences will have equalised out. The skill for the practitioner lies in deciding whether a presentation is pathological or likely to cause pathology in later life, or it is normal. In order for the practitioner to make objective decisions it is important that they has a good understanding of normal development and the approximate age by which certain milestones should be reached (Table 14.1). The developmental stage of the child, as measured by neurological maturation, will influence both their posture and gait.
Table 14.1 Developmental milestones
| Age | Milestone |
|---|---|
| Birth | Head control absent. Flexion to upper and lower limbs. |
| 2/12 | Can rise up onto forearms and can extend head to look up. |
| 5/12 | May take major proportion of weight when supported in standing. |
| 6/12 | Rolling from prone to supine |
| 7/12 | Can sit unsupported |
| 9/12 | Begins to crawl and can stand momentarily holding on to furniture |
| 1 year | Can walk supported by one hand. Can squat with wide base of support |
| 15/12 | |
| 2 years | Climbs stairs two feet per stair. Can run and jump |
| 3 years | Can run and hop and falls less frequently |
| 4 years | Can walk downstairs one foot per step |
| 5 years | Can skip with both feet |
Abridged from Thomson & Volpe (2001).
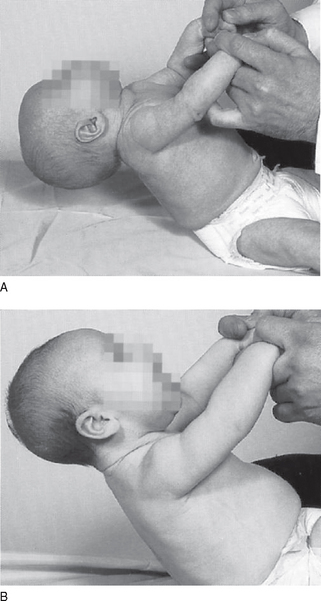
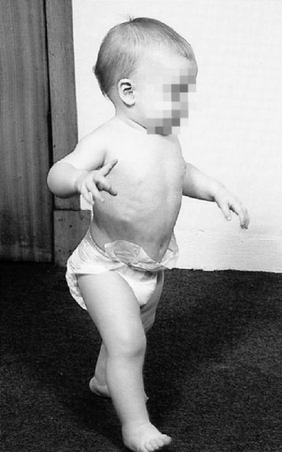
Early posture
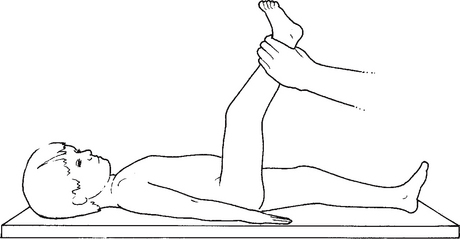
Neurological maturation is cephalic to caudal in direction. Hence, strength is first seen in the neck muscles (Fig. 14.1). At 6–7 months most babies will sit unassisted and attempt to crawl by 9–12 months. They will start to pull themselves up into a standing position and stand holding on to furniture (cruising) at 9–12 months, but they frequently fall backwards into a sitting position. By 12 months the child should be able to stand alone briefly and may possibly walk alone; 97% of children start to walk between 9 and 18 months. Of the remainder only 6% are neurologically compromised (Luder 1988). The early walker has an immature spinal curvature, that is ‘C’ shaped (in the sagittal plane) as opposed to ‘S’ shaped in the adult. The child will have a wide base of gait for stability, with the arms flexed and held high for balance and no arm swing (Fig. 14.2). The base of gait will become narrower as the child gains confidence and develops a heel-to-toe gait from 3 years of age.
Determinants of gait
Gait is closely associated with maturation of the central nervous system (CNS) and encompasses the essential developmental milestones, based on six components affecting walking. The various components (see Ch. 10, section B) commence from the time the child first starts to walk and continue to the age of 6+. Learning skills, balance and physiological changes all contribute to the process of maturity, assisting the young child to eventually walk in an adult fashion. If all these develop normally, by the sixth year there is little to differentiate the child’s gait from that of the adult.
Early gait
On average a child will start to walk independently at about 1 year of age, although some will be later than this. If a child has shown no desire to walk by 18 months, investigation is required. At this stage the base on which the child balances will be wide. Cadence is relatively high (approximately 180 strides/min) (Volpe 2001) and single leg support and stride length short. There is no reciprocal arm swing/contralateral footstep. There is weakness of the ankle dorsiflexors causing a foot drop and a slapping flatfoot strike. The foot neither supinates nor pronates. There is little frontal or sagittal plane movement at the pelvis. The child thrusts their head, the heaviest single component of the body, downwards to increase speed and upwards and backwards to reduce velocity.
Six+ years of age
Cadence has now reduced to approximately 140 strides/min and gait is now indistinguishable to that of an adult. According to Volpe (2001) walking velocity, reduction base of gait (determined by pelvic span divided by ankle spread), duration of single leg support and cadence are the major factors distinguishing the immature gait of the toddler from that of the adult.
Growth and development
At birth many of the bones of the foot are still cartilaginous and therefore not visible on X-ray. Only bone cells with a calcium and phosphate mineral composition are readily identified on X-ray film. As the diaphyses are apparent before birth, metatarsals and phalanges can be seen on plain X-ray, albeit as rather poorly defined areas. The calcaneus and talus are clearly visible on X-ray. The short bones of the midtarsus are also already formed at birth, although the navicular and cuneiforms are rather imprecise (lateral appears first at 3–6 months) and can take another 2–3 years to have a functional calcific appearance. The sesamoids of the first metatarsal appear around 8–10 years of age (Ch. 12).
Most books on anatomy will have a useful and comprehensive timetable of ossification for the bones of the lower limb, therefore these will not be considered here. When reading X-rays, knowledge of the position of the epiphyses is desirable to avoid misinterpretation, for example, the first metatarsal base is the site of the epiphysis, whereas the epiphysis of the other metatarsals is located at the metatarsal head. However, of special interest is the epiphysis of the styloid process at the base of the fifth metatarsal. The epiphysis runs parallel with the longitudinal axis of the bone and is often misdiagnosed as a fracture. Fractures in this area tend to lie at 90° to the axis (Fig. 14.3). Knowledge of ossification is also important for providing effective treatment at the most appropriate time (e.g. metatarsals ossify around 14–16 years in females and 16–18 years in males). It is also useful to remember that in children some bones may appear to be oriented differently from those of the adult foot. The lower limb continues to grow in length and girth until the age of 19–20 years in males. Females tend to mature earlier and therefore growth usually ceases around 15–17 years.
The assessment process
Assessment can be divided into two areas: history taking and examination.
General considerations
A child needs time to settle and questions should always precede ‘hands-on’ examination. Watching, listening and adopting an ‘open’ posture all convey the impression that the practitioner is interested and caring (Thomson 2001). A casual approach to the practitioner’s dress may also be desirable as children who have suffered discomfort at a previous medical consultation may associate a white coat with a bad experience. Research suggests that doctors who dress more casually are perceived to be more friendly (Brandt 2003). To a frightened child such perceptions may make the difference between a consultation that has gone well and one that has been fraught for all parties concerned. When children can relate to the practitioner, they may be more willing to cooperate.
It must also be remembered that children between the ages of 6 months and 3 years undergo ‘stranger anxiety’ and a child might become distressed when approached by a stranger. It may be that under these circumstances the consultation process needs to be prolonged until the child feels comfortable enough to cooperate with the examination. At the other end of the age spectrum adolescents may be more cooperative but less communicative. They may also be embarrassed about the changes that are happening to them physically. Therefore great sensitivity may be required when requesting articles of clothing be removed for the examination (Thomson 2001). Time may also be a great restraint. However, a little time spent getting to know the child is never time wasted. The use of toys and other distracters may also be helpful.
Interviewing
It may be easier to interview the parent while the child is playing. Watching the child at play allows evaluation of motor coordination and posture. It is important that during any assessment the child is chaperoned, as any misinterpretation of the physical exam cannot be permitted. The presence of another person, preferably another professional, e.g. nurse or care assistant, but at the very least the parent, will allow a third party to bear witness to events. During the examination it is also reassuring for the patient if the practitioner explains that they are about to touch a limb or hip and gives a reason why, in language appropriate for the child’s age. In young children, it is preferable that the parent undress the child in order to aid the process and to lower any anxiety for the child. The parents should be requested, prior to attending, to dress the child in easy-to-remove clothing.
A flexible approach to questioning may be necessary in cases of difficult children. If the child is uncooperative, do not hesitate to temporarily abandon the examination or reschedule the appointment for a time when the child is less tired or irritable. Bereavement or a seriously ill sibling may be the reason for inappropriate behaviour especially in young children who are unable to express their fears or emotions any other way (John 2001). The practitioner may have to alter their approach in order to get the best from such consultations.
One aspect of paediatric management is an ability to reassure the parents (Meadow 1992). Importantly, the practitioner should always address the parents’ concerns. Cause and treatment should be explained using plain language and any existing parental anxiety should not be exacerbated by giving a list of all possible complications. Similarly, the use of terms such as chronic, progressive, delay or tumour should be avoided unless the diagnosis is to have a fundamental impact on the life of the child and of the family and support is available. While it is wise to avoid raising expectations of treatment, always try to end the consultation on a positive note.
History taking
Perinatal history
Pregnancy
It is important to determine whether the pregnancy was normal. Once again it is obligatory to be fastidious in obtaining a full relevant history. There is a 2% increase in postural problems among first-born children born to young women with tight abdominals (Dunn 1974). Widhe (1997) reported an incidence of 4% foot deformities among 2400 newborns examined. Therefore it is important to record the child’s position in the family. Similarly the mother’s medicine history during this period needs to be investigated. For example, methotrexate or phenytoin (an anti-epileptic drug), and high doses of vitamin A, are known to be teratogenic during the first trimester of pregnancy. This trimester is a period of organogenesis where organs and systems are developing. Any insult at this stage may have major consequences for the still-developing fetus. Certain questions will be easy to get answers to. Some questions, especially regarding non-prescribable or social drugs, may be reserved for cases in which visible signs of abnormality are evident. Smoking by the mother has been reported to cause intra-uterine growth retardation (IUGR) and excessive alcohol intake can delay intellectual development. In the worst cases, the child may be born with fetal alcohol syndrome. The practitioner must elicit such information without creating anxiety or appearing to be judgemental. However, such an avenue of exploration requires considerable tact. History of complications such as threatened miscarriage, antepartum haemorrhage or toxaemia need to be recorded as does known exposure to infections that have been proven to cause abnormality in the child (e.g. measles, chicken pox). It is important not to alarm the parent as incidental findings are rarely conclusive. The majority of babies encountered are healthy.
Delivery
The mother should be asked about the nature and duration of her labour. Was the delivery uneventful, full term (40 weeks) or premature (gestational age less than 37 weeks)? Muscle tone is diminished in premature babies compared with those who reach full term and they also have an increased predisposition to developmental dysplasia of the hip (DDH). Incidence of hip dislocation is higher among malpositioned fetuses (breech position) or when there are twins. In a recent study of children born with congenital postural deformities (Mikov et al 2005) foot deformities were the most common deformity (78%), and in this study group over 17% were breech presentations (compared with 0.7% in the control). A caesarean section is often indicated in cases of malposition, large fetal size or fetal distress. Therefore, although having a caesarean delivery may lessen the trauma and potential injury for the child that is inherent via the vaginal route, the practitioner must be alert to the reasons why this was procedure was chosen, i.e. was it elective or an emergency. Non-elective surgery may have been necessary because the child was anoxic in utero and this knowledge may be significant in cases where there is evidence of poor posture, poor coordination or other example of impaired motor function.
Neonatal history
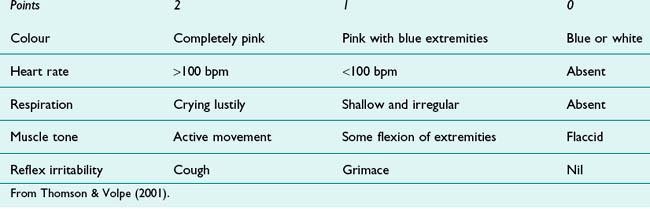
At birth, babies undergo several tests to determine their APGAR score (Apgar 1953). This routine procedure is performed at the first (index of asphyxia) and fifth (index of neurological residua or death) minute after birth. It is used to evaluate the cardiovascular, respiratory and neurological status of the neonate:
• Pulse – indication of heart rate
• Grimace – plantar aspect of the foot is stimulated to provoke the child to cry
A baby’s response to each test is rated on a scale of 0–2. A score of 10 is the maximum and is rarely achieved; a low score below 6 especially at the second test is a reason for concern and may indicate some form of long-term neurological deficit (Table 14.2).
Developmental milestones
Knowledge of the normal developmental milestones (see Table 14.1) is important for the recognition of suspected neurodevelopmental disorders. When neurodevelopmental delay is suspected, detailed questions on the following are indicated:
• Ability to hop on one foot, tandem walk
• Ability to walk up and down stairs
• Result of 8-month hearing test
Family history
A family history of the presenting condition may provide vital information about the cause and the prognosis of the complaint. Information concerning siblings with similar problems and what the success (or otherwise) of any interventions should be noted. It is helpful to ascertain if any family traits exist, and these may be usefully represented by constructing a pedigree chart (Ch. 5). In genetically determined conditions, e.g. immune-deficiency states, neurodegenerative disease or muscular dystrophy, enquiries about second-degree and third-degree relatives may be worthwhile.
Examination
Neurological assessment
Neurological assessment implies motor and sensory evaluation. In the UK all neonates are examined by a paediatrician after delivery; midwives and health visitors undertake follow-up tests during the early years of development. Most neurological abnormalities will be detected during this stage. Reflexes are an important method for determining normal muscle development and innervation in the neonate. Certain involuntary (primitive) reflexes disappear after 1 year of age. Reflexes present during the first year of life are summarised in Table 14.3. The formal neurological examination of an infant will include an evaluation of the primitive reflexes, muscle tone/power, coordination (hand/eye) and posture in relation to development. Neurological examination of the older child should emphasise evaluation of superficial/deep reflexes, muscle tone/power (stand on tiptoes/heels) and coordination (heel-to-toe walking, balancing on one leg, hopping). This is one area where a working knowledge of the developmental milestones is essential as it makes a nonsense of the examination to ask a 3-year-old to skip with both feet when they do not have the neurological maturity to be able to carry out the instruction.
Table 14.3 Reflexes associated with development
| Reflex | Description |
|---|---|
| Oral reflex | If a finger is placed in a baby’s mouth, the baby will automatically suck and swallow. Failure to suck may indicate a cerebral problem later leading to motor dysfunction in the lower limb |
| Moro reflex | This reflex (startle reflex) disappears by 5 months. The infant is held in a supine position with one hand supporting the head and neck. By sudden slight dropping of the examiner’s hand supporting the head a response is elicited. The normal response is for babies to spread their arms away from their chest with hands open and fingers spread apart followed by a movement of the arms towards the centre of their chest as if in an embrace. The legs are flexed. Failure to respond suggests weakness. Asymmetry may indicate lower spinal lesion if one leg affected. Hyperactivity suggests CNS infection and reverse Moro. Where the baby extends limbs with external rotation, this indicates basal ganglia disease |
| Grasp reflex | Palmar or plantar response up to 9 months. An object is placed in the palm and the fingers automatically flex to grip the object. The foot would be similarly stimulated in the area behind the toes. Failure to respond suggests CNS weakness, depending on symmetry of reflex |
| Plantar reflex | This is achieved by firmly stroking the lateral sole of the baby’s foot and extending the movement across the ball of the foot. A normal response in a child under 1 year is extension of the hallux. An abnormal response indicates dysfunction of the upper motor neurones |
| Placing and stepping/walking reflex | If you touch the anterior aspect of either upper or lower limb (anterior tibia) against the edge of an examination couch the child will lift the limb to place the foot/hand onto the surface of the couch. Alternatively, place the dorsum of the foot beneath the table top to attain the same response. This occurs in the newborn up to about 4 weeks of age. If the baby is gently held above a surface with the soles lightly contacting the surface this will elicit a stepping/walking motion. This response is present until 8 weeks of age. Absence may indicate brain damage |
| Tonic neck reflex | When the baby is supine and not crying, the head will be turned to one side and the arm on the same side will be extended. The other knee will often be flexed. In normal babies, passive rotation of the head will increase upper body muscle tone on the side to which the head is turned. This reflex present up to 3 months |
| Patellar and ankle | Results should be similar to normal adult tendon reflex |
All practitioners should be mindful of skeletal and gait abnormalities which indicate a neuromuscular disorder, e.g. Charcot–Marie–Tooth disease (Case history 14.1), Duchenne’s muscular dystrophy and Friedreich’s ataxia. In some cases late walking may be due to neurological dysfunction undetected at birth or to DDH. Neurological tests should be carried out if an abnormality is suspected in such cases (Ch. 7).
Musculoskeletal assessment
Musculoskeletal assessment can be subdivided into three parts:
The examination process outlined in Chapter 10 can be used with children as well as adults; however, the following specific points should be noted.
Gait analysis
The principles of gait analysis in the paediatric examination are the same as those for an examination of an adult patient (see Chs 10, 11). However differences do exist and these are fundamentally due to the child’s changing gait as they mature. The examiner must familiarise themselves with the changes in order to identify a pathology when it exists. Gait analysis starts from the walk from the waiting room to the surgery and this initial contact enables the practitioner to gain a general impression of lower-limb function. Capturing the child unawares may reveal many clues to the problem which may be hidden when under the glare of the formal examination. It is also an opportunity to observe the child wearing shoes in order to evaluate the effect of the footwear on lower limb mechanics. Formal gait analysis should be done with the child barefoot and in shorts. This allows the position of the lower limb, especially the knees to be assessed. An evaluation should be made as to whether the child’s gait is appropriate for their age. As with all patients it is important to observe the child from head to toe, taking note of any signs of asymmetry of posture. The head should be level in the frontal plane. In very young children the head is positioned slightly ahead of the body and may tilt downwards in the sagittal plane to improve forward momentum as the child chases their centre of gravity. Symmetry of facial features and head size should also be evaluated. The shoulders should be aligned and a child over 6 years should have symmetry of arm position (same distance from the body) and symmetrical arm swing. In static stance the arms should hang level; if they appear uneven when fingers are straightened this may suggest a corresponding shoulder drop. If shoulders are level and there is no evidence of scoliosis then anisomelia of the arms may be present. When one arm is held close to the body in a flexed position a neurological assessment is indicated in order to rule out an upper motor neurone lesion, e.g. as in hemiparesis or cerebral palsy (Fig. 14.4).
Weightbearing assessment
Spine
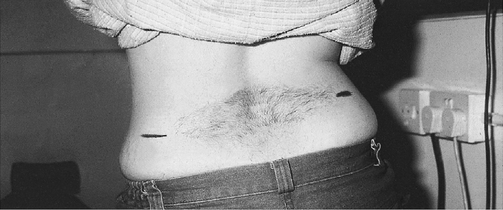
It is important to check the spine for shape, deformity and movement. Check for normal skin covering and absence of dimpling at the base of the spine over lumbar vertebrae 3/4. Dimpling, or the presence of a tuft of hair at the base of the spine may indicate spina bifida occulta (Figs 14.5, 14.6). Note whether scoliosis, kyphosis or lordosis is present and whether it is a functional or fixed deformity. A fixed deformity is usually due to bony abnormality (structural), whereas a flexible (functional) deformity is due to soft-tissue contracture. Fixed spinal curvatures are retained when sitting and flexing the spine, especially scoliosis. Scoliosis is a frontal plane deformity but there may be signs of vertebral rotation, causing a kyphotic or humped appearance in the sagittal plane. Progressive thoracolumbar problems can impair pulmonary function and in time may lead to strain on respiration.
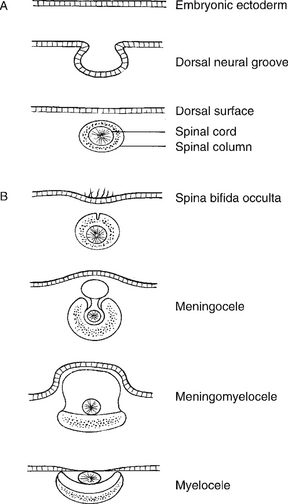
Figure 14.5 A Normal development of the neural tube and spine. B Classification of spinal dysfunction.
Non-weightbearing assessment
Pelvis and hips
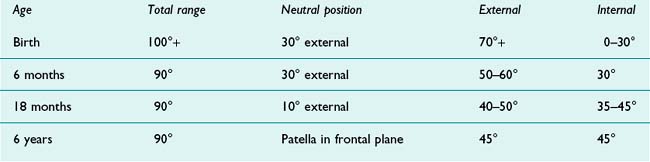
Altered function of the gluteal muscles due to hip dysplasia will cause a change in the shape of the buttocks. As a result the gluteal fat folds will not appear level. This is the so-called ‘anchor sign’ in which the central crease forms the shaft of the anchor and the two gluteal folds at the inferior edge of the buttocks form the arms the anchor. If the arms of the ‘anchor’ are not level this implies asymmetry (Fig. 14.7). When performing tests on the hips of children, the practitioner must avoid damaging the blood supply to the femoral head. At birth the head of the femur lies superficially in the acetabulum, which gives the appearance that the thigh is externally rotated on the pelvis. As the child develops, the head of the femur goes deeper into the acetabulum, which in turn allows the limb to internally rotate. In a normal neonate there is a ratio of 2 : 1 external to internal hip rotation. With development, the amount of external rotation reduces as the amount of internal rotation increases to the point where a normal adult value shows equal internal and external rotation of 45° in each direction (Table 14.4). When undertaking formal hip examination it is important to evaluate flexion/extension, abduction/adduction and internal/external rotation in both hip-flexed and hip-extended positions (see Ch. 10, section A). This should be followed by assessment of hamstring tightness (Fig. 14.8). The lengths of the tibiae and femurs can be compared using the Allis/skyline test (see Fig. 10A.28). A limb-length discrepancy in an infant may be indicative of hip dislocation. However, the examiner must be vigilant to the possibility of bilateral dislocation, where there will be symmetry.
In the neonate, ligamentous laxity may be present, together with instability of the hip. This is associated with circulating maternal hormones, in particular, relaxin, a polypeptide produced by the corpus luteum. Correct technique in hip examination is paramount in order to prevent iatrogenic dislocation or avascular necrosis of the femoral head. Nerves lying posterior to the hip joint, particularly the sciatic nerve, are subject to trauma in posterior hip dislocation. Damage to the nerve may lead to motor and sensory loss.
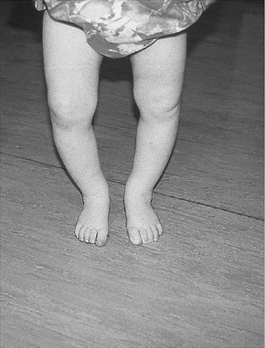
Knees
During childhood the knee undergoes a swing in the frontal plane from varus to valgus and then back towards neutral as shown in Table 14.5 (Beeson 1999). Bow legs (genu varum) occur normally between birth and 2 years of age (Fig. 14.9). Physiological genu valgum (knock knees) is commonly seen between the ages of 3 and 6 years (Salenius & Vankka 1975). At 4 years of age girls tend to be more knock-kneed than boys (Heath & Staheli 1993). Children usually outgrow physiological genu valgum by the age of 8 years (Beeson 1999). Some authors have suggested that a second episode of genu valgum may occur between 12 and 14 years of age (Laporta 1973); this is mainly seen in girls due to the pubertal effects of growth (Cahuzac et al 1995).
Table 14.5 Frontal plane alignment of the knee
| Birth | Genu varum 15–20° |
|---|---|
| 2–5 years | Straight |
| 4–6 years | Genu valgum 5–15° |
| 6–12 years | Straight |
| 12–14 years | Genu valgum 5–10° |
| 14–16 years | Straight |
Knee position can be assessed with the child either lying supine or standing. In the supine position the child’s knees or ankles are placed together with the legs parallel to the examination couch. The distance between the medial femoral condyles of the knees and medial malleoli of the ankles can then be measured with a tape measure.
The child should be observed from the side for genu recurvatum (hyperextension). This deformity occurs in the sagittal plane. In very early childhood, genu recurvatum may be present but should reduce with development as the knee ligaments tighten. If reduction does not occur the patient should be tested for ligamentous laxity (Harris & Beeson 1998).
The range of transverse plane motion in the knee should be equal in both directions and be minimal by the age of 4 years. In the newborn 20–30° of total motion may be available (Kilmartin 1988). The amount of rotation of the tibia on the femur should reduce by 10° at 3 years of age and at 6 years of age should show minimal movement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree