Chapter 20 Articular Cartilage
Biology, Biomechanics, and Healing Response
Articular cartilage forms the load-bearing surfaces of all synovial joints. Its highly organized structure provides the biomechanical properties necessary for the tissue to withstand multiple forces created during movement.* Following injury, articular cartilage has limited healing potential because the cells have minimal mitotic activity and the matrix lacks a vascular supply10,35,36 It is important for orthopedic surgeons to understand the basic science of articular cartilage because advances in the treatment of cartilage defects are utilizing tissue engineering repair techniques in an attempt to regenerate and develop tissue with structural and mechanical properties similar to those of normal cartilage.19,31,37 Also, identification of biochemical biomarkers that detect early cartilage degradation may lead to the development of treatments to prevent, halt, or reverse cartilage damage before the onset of severe degeneration.4
Biology and Structure
The main functions of articular cartilage in synovial joints are to provide a low-friction surface for motion and to resist tensile, shear, and compressive forces.2,3,45 Articular cartilage varies in specific composition within the same joint and between different joints, but it consists of the same basic components and structure throughout all joints.2 Grossly, articular cartilage appears as a smooth, homogeneous tissue approximately 2 to 5 mm thick (Fig. 20-1). When probed, healthy cartilage is firm and resists deformation. Diseased cartilage is soft, deforms when probed, and may contain visible surface disruptions.
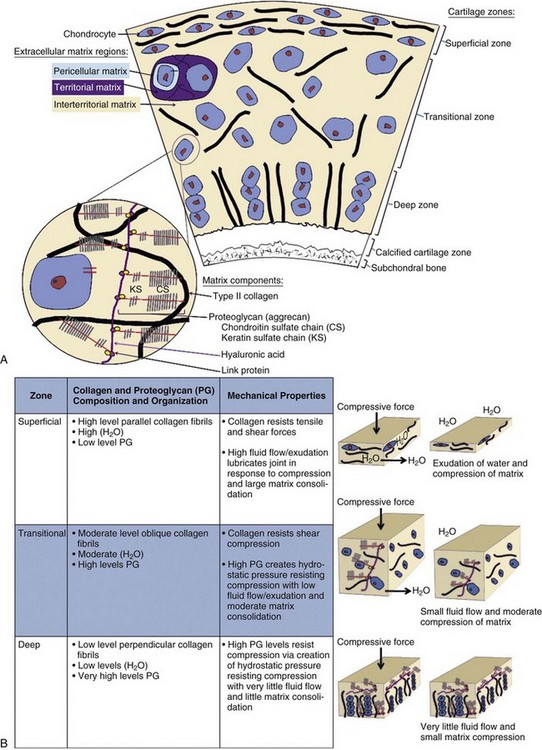
Articular cartilage consists of a sparse population of chondrocytes embedded within a highly hydrated extracellular matrix composed of collagen and proteoglycans. The composition of articular cartilage varies with depth from the surface, and it is divided into four structural zones.3,31 The matrix is also divided into three regions, and its composition varies with distance from the chondrocyte.13 This precise arrangement of the tissue components provides specific mechanical properties for each zone.45 Chondrocytes synthesize matrix components and regulate homeostasis of articular cartilage.17
Chondrocytes
Chondrocytes, the single cell type in articular cartilage, account for a small amount of cartilage tissue (5% of weight, <10% of volume) but perform the vital roles of extracellular matrix synthesis and regulation.29 Chondrocytes are derived from pluripotential mesenchymal stem cells (MSCs) and differentiate into chondroblasts and mature chondrocytes.42 Articular cartilage is avascular, thus chondrocytes must derive nutrition and oxygen from the synovial fluid by diffusion and must meet energy requirements through glycolysis.17 Each chondrocyte is surrounded by extracellular matrix and forms few cell-cell contacts2 (Fig. 20-2A). Despite this isolated arrangement, chondrocytes are able to respond to a variety of mechanical and biochemical factors.42
Chondrocytes differ in size, shape, and metabolic activity in the different structural zones, but all cells contain endoplasmic reticulum and Golgi apparatus for matrix synthesis.17,46 Chondrocytes synthesize the two major articular cartilage macromolecules—type II collagen and aggrecan—and organize the structure of the matrix.2 Specific interactions between chondrocytes and the extracellular matrix are unknown, but detection of a variety of mechanical and biochemical factors by the chondrocyte is vital for matrix synthesis and homeostasis. A few mechanisms have been discovered, including the presence of binding proteins (integrins) and osmotically sensitive ion channels on the cell surface of chondrocytes.29,42
Development and maintenance of the chondrocyte phenotype is an important research topic because current and future treatments for articular cartilage damage include implantation of stem cells and chondrocytes into defects.19,25,39 In vitro study of chondrocytes has shown that proliferation and expansion of chondrocytes in monolayer results in loss of cell phenotype and subsequent synthesis of type I collagen. However, culture conditions that include high cell density, cell-cell contact, and a three-dimensional environment appear to maintain the chondrocyte phenotype and the production of type II collagen.37,47 Growth factors such as transforming growth factor-β (TGF-β), fibroblast growth factor (FGF), and insulin-like growth factor-1 (IGF-1) also appear important for maintenance of the chondrocyte phenotype, with identification of receptors on chondrocytes.42 A range of other molecules such as oxygen and common injectable anesthetics have been shown to have an impact on chondrocytes. In a recent study, sustained hypoxia in vitro increased type II collagen gene expression and proteoglycan synthesis.6 Also, a one-time dose of 0.25% to 0.5% bupivacaine has been reported to be toxic to human chondrocytes in vitro in a dose- and time-dependent manner.5 Further research is required to understand the complex interactions of numerous biochemical factors with chondrocytes.
Extracellular Matrix
Most of the articular cartilage (90%) is composed of the extracellular matrix. The matrix consists of tissue fluid and macromolecules.2 The composition of the zonal structure of the matrix determines its interaction with tissue fluid and thus is responsible for determining the mechanical properties of the cartilage.31 The main functions of the matrix are to resist tensile and shear forces through the arrangement of collagen fibrils, and to resist compressive forces through alteration in hydrostatic pressure.9,18,24
Tissue Fluid
Water is the major component of the extracellular matrix (75% weight) and tissue fluid.2 Tissue fluid also consists of high concentrations of cations, gases, and small proteins. The volume of water present in the cartilage tissue depends on the concentration and organization of the macromolecules, specifically, proteoglycans. The concentration of proteoglycans varies between cartilage zones, contributing to differences in water concentration, porosity, and permeability of the tissue.29,31 Throughout joint movement, water continually moves into and out of the cartilage to aid in distribution of compressive forces and lubrication of the cartilage surface.18
Macromolecules
The macromolecules of the extracellular matrix include collagens (20% of the matrix), proteoglycans (5%), and noncollagenous proteins and glycoproteins (1%).2 Type II collagen fibrils provide structural integrity and tensile and shear strength to the articular cartilage.44 Proteoglycans, mainly aggrecan, attract water, providing resistance to compression.45 The noncollagenous proteins and glycoproteins help to bind chondrocytes to the matrix, stabilize matrix macromolecules, and assist in regulation of matrix homeostasis.29
Collagens
Articular cartilage contains multiple types of collagen, including II, VI, IX, X, and XI.29 Type II collagen accounts for 90% of the collagen in articular cartilage.2 Type II collagen is composed of three alpha chains, which intertwine into a triple helix. These helices covalently cross-link in a lateral array to form collagen fibrils.34 This network of fibrils contributes to maintenance of the volume, shape, and tensile and shear strength of the cartilage. Levels of type II collagen are highest in the superficial zone and decrease in concentration with increasing depth from the surface33 (see Fig. 20-2A and B). The collagen fibril network restrains the proteoglycans in the matrix and prevents swelling of the cartilage to greater than 450 mOsm when water flows into the tissue.33 This allows creation of high tissue pressure, which is vital for resistance of compressive forces.
Under physiologic conditions, type II collagen metabolism is slow and fibrils have a half-life of years. In early stages of cartilage degeneration, degradation of collagen fibrils is observed.26 Enzymes called matrix metalloproteinases (MMPs) are thought to contribute to this degradation, specifically collagenases and aggrecanases. Collagenases mediate cleavage of type II collagen and produce two main fragments.26 Antibodies to specific neoepitopes on these fragments can be detected by synovial fluid, serum, or urine assays and are being studied for use as potential biomarkers of early cartilage degradation.1,4,26
Other collagen types are less prevalent but perform important functions, including stabilization and regulation of type II collagen fibrils. Type IX collagen forms cross-links along the surface of type II collagen fibrils and interconnects the fibrils with proteoglycan aggregates.29 Type XI collagen binds to the interior structure of type II collagen fibrils and regulates the diameter of the fibrils. Type X collagen is localized near the calcified cartilage zone and the hypertrophic zone of the growth plate and is thought to contribute to cartilage mineralization.29 Type VI collagen is located in the pericellular matrix and aids in the attachment of chondrocytes to the extracellular matrix.13
Proteoglycans
Proteoglycans (PGs) consist of a protein core with glycosaminoglycan (GAG) side chains.29 GAGs consist of long unbranched polysaccharide chains containing repeating disaccharides of amino sugars with negatively charged carboxylate or sulfate groups.28 Specific GAGs include hyaluronic acid (HA), chondroitin sulfate (CS), keratan sulfate (KS), and dermatan sulfate (DS). The major proteoglycan (90% of mass) in articular cartilage is aggrecan.8 Aggrecan has many CS and KS side chains and noncovalently associates with an HA backbone to form aggregates (see Fig. 20-2A). HA is a long-chain nonsulfated GAG capable of binding a large number of aggrecan molecules. Link protein, a glycoprotein, stabilizes the association between HA and each aggrecan molecule.29
Aggrecans play a key role in generating hydrostatic pressure. The negatively charged aggrecans attract cations, increasing the osmolality of the tissue. Water is then attracted into the tissue, decreasing the osmolality.45 Hydrostatic pressure created by the interaction of collagen, PGs, and water provides stiffness to the cartilage to absorb compressive mechanical loads without damage to the matrix. Displacement of water from PGs during compression of the superficial zone of matrix lubricates the joint.45
Under physiologic conditions, aggrecan turnover occurs over a period of years.26 Similar to collagen, degradation of aggrecan is observed in early cartilage degeneration, and aggrecanases are thought to contribute.1 Aggrecan synthesis and degradation can also be measured by antibodies to specific neoepitopes on fragments by synovial fluid or serum assays. Inhibitors of aggrecanases are being investigated for potential treatments for cartilage degeneration.11
Smaller PGs include decorin, fibromodulin, and biglycan.29 The function of each PG is related to the specific core protein and GAG chains that it contains. Decorin contains DS side chains and is located at the surface of type II collagen fibrils. It is thought to inhibit the lateral growth of fibrils and contributes to organization and stabilization of the fibrils. Fibromodulin has KS side chains and binds type II collagen fibrils, providing stabilization. Biglycan contains DS side chains, binds TGF-β, and interacts with type VI collagen in the pericellular matrix.29 Expression of smaller PG changes within zones and with mechanical stress likely contributes to cell stabilization and signaling through interaction with other proteins.29
Noncollagenous Proteins and Glycoproteins
The matrix contains many additional proteins that represent a small volume but a large molarity of the tissue.2 Cartilage oligomeric matrix protein (COMP), anchorin, and fibronectin function to bind chondrocytes to the matrix. COMP binds to chondrocytes in the territorial matrix.7 Anchorin binds to chondrocyte surface protein, anchoring chondrocytes to collagen fibrils. Fibronectin is an adhesion molecule expressed on the surface of chondrocytes.7 Ongoing research is investigating the roles of these proteins, but most appear to aid in organization and stabilization of the chondrocytes and matrix.29
Other proteins include growth factors and cytokines, which bind to chondrocyte receptors, altering rates of matrix synthesis and degradation. Effects of these proteins depend on their concentration, cofactors, type of target cell, and number of cell receptors. TGF-β, IGF-1, FGF, bone morphogenetic protein (BMP), and platelet-derived growth factors (PDGFs) stimulate matrix synthesis and proliferation.42 TGF-β, FGF, and PDGFs also promote proliferation and chondrogenic differentiation of mesenchymal stem cells in combination with many other factors. Matrix degradation is stimulated by interleukin-1 (IL-1), tumor necrosis factor-alpha (TNF-α), and MMPs.42
Regions Surrounding the Chondrocyte
Matrix composition and organization vary with distance from the chondrocyte. Three regions have been identified: pericellular matrix, territorial matrix, and interterritorial matrix2 (see Fig. 20-2A). The pericellular matrix directly surrounds the chondrocyte; the territorial matrix surrounds the pericellular matrix and assists in binding the chondrocyte cell membranes to the matrix. The pericellular and territorial regions also transmit mechanical signals to the chondrocytes when the matrix deforms.13 Most of the matrix is contained in the interterritorial region, which consists of collagen fibrils and PG aggregates and provides the mechanical properties of the cartilage.3
Pericellular Matrix
In all cartilage zones, the individual chondrocyte is directly surrounded by the pericellular matrix. Chondrocyte cell membranes attach to the rim of the pericellular matrix covering the cell surface. This region contains many PGs and proteins, including type VI collagen, decorin, anchorin, and fibronectin.13 This region contains little to no fibrillar collagen. The function of this region is not fully understood, but it serves to regulate the microenvironment of the chondrocyte. The presence of type VI collagen defines this region and anchors the chondrocyte cell membrane to the matrix.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree