CHAPTER 13 Arthroscopy in the Throwing Athlete
Excessive valgus and extension forces are generated during the throwing motion in several sports, especially baseball, tennis, football, and certain track and field events.1 The repetition required to excel in these sports can ultimately lead to fatigue and even failure of key stabilizing structures in the elbow. The medial ulnar collateral ligament (MUCL) is the primary restraint to a valgus load during the throwing motion and is most susceptible to injury after repetitive throwing. MUCL insufficiency leads to valgus instability, a condition that is significant only in overhead athletes. Over time, chronic valgus instability can result in a unique constellation of elbow pathologies that are indicative of repetitive overhead throwing.
Several investigators have described the most common injuries seen in the elbow of the throwing athlete, including MUCL injuries, ulnar neuritis, posteromedial impingement with osteophyte formation, flexor-pronator strain, ulnar stress fractures, osteochondritis dissecans of the capitellum, and capsular contracture.2–8 Although not all pathology in the thrower’s elbow is amenable to arthroscopic management, clinicians who care for throwing athletes must be familiar with all pathologic conditions and comfortable with open and arthroscopic treatments.
ANATOMY
The elbow is a hinge joint with the bony ulnohumeral articulation that provides stability at the extremes of motion, from 0 to 20 degrees of flexion and beyond 120 degrees of flexion.3 The intervening 100 degrees, which is the primary arc of motion used in overhead throwing, relies progressively on the static and dynamic soft tissue restraints to provide stability.
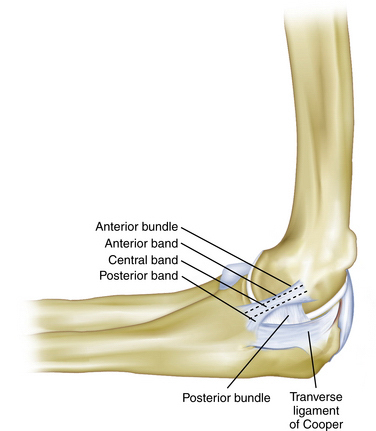
The MUCL is not a single ligament but is rather a complex consisting of an anterior bundle, a posterior bundle, and a transverse component (Fig. 13-1).9 The anterior bundle is the most well-defined structure, and it originates on the medial epicondyle and inserts on the sublime tubercle. The anterior bundle is subdivided into three components: an anterior band, a central band, and a posterior band. The anterior and posterior bands tighten in a reciprocal manner during flexion and extension, respectively. The posterior bundle is a less distinct fan-shaped structure. The transverse ligament is the least distinct anatomic structure and provides very little stability to the elbow because it does not cross the joint. Biomechanical studies have demonstrated that the anterior bundle is the primary constraint to valgus stress about the elbow.10–12 Further studies have shown that the anterior band of the anterior bundle provides most of the stability from 30 to 90 degrees of flexion, whereas the posterior bundle becomes functionally significant between 60 degrees and maximum flexion.13
The mechanics of overhead throwing, particularly pitching, account for the various pathologies seen in overhead athletes. Valgus forces have been estimated to reach 64 N during the late cocking and early acceleration phases of throwing.3,14 After the early and late cocking phases, the elbow goes from rapid flexion to extension, and the tangentially directed forces produce a valgus and extension moment, with resulting tensile forces across the medial side of the elbow, compressive forces across the lateral aspect of the joint, and shear forces in the posterior compartment.3,4,15 The repetitive stress on the MUCL eventually leads to attenuation and ultimately rupture, resulting in an insufficient ligament complex, abnormal valgus rotation of the elbow, and instability. The term valgus extension overload describes this phenomenon.2,16 As the athlete continues to throw with instability, the valgus overload is accentuated, and excessive valgus moments lead to stretch of other medial structures, resulting in ulnar neuritis, flexor-pronator tendinopathy, or medial epicondyle apophysitis in the skeletally immature patient.
Corresponding overload on the lateral side of the elbow may lead radiocapitellar chondromalacia, osteophyte formation, and loose bodies. During extension, posterior shear forces can produce olecranon osteophytes at the posteromedial tip with a corresponding kissing lesion on the posteromedial trochlea.3 The clinician who treats throwing athletes must be familiar with these pathologies and be alert for underlying MUCL insufficiency as the cause of many of these disorders, because treating the pathology without ligament reconstruction often fails to relieve the athletes’ symptoms and allow them to return to sport.
PATIENT EVALUATION
Physical Examination
Inspection of the elbow begins with an assessment of the resting position of the elbow and its carrying angle. A normal carrying angle is approximately 11 degrees of valgus for men and 13 degrees of valgus for women.3 An increase in the carrying angle of valgus may indicate an adaptation to the repetitive stress of valgus instability. Angles of greater than 15 degrees in professional pitchers have been documented in the literature.17 The lateral, posterior, medial, and anterior regions of the involved elbow should be examined for swelling, obvious deformity, scars, or signs of previous trauma.
In the posteromedial region of the elbow, the ulnar nerve is easily palpable in the groove, which is located between the medial epicondyle and the olecranon. The examiner should test for a Tinel sign and for hypermobility. This is done by palpating the nerve as the elbow is brought from extension to terminal flexion to determine whether the nerve subluxates or completely dislocates over the medial epicondyle. Palpation of the posteromedial region of the elbow should also focus on the olecranon, which can reveal osteophytes or swelling that occur in throwing athlete with valgus extension overload syndrome. The medial subcutaneous border of the olecranon should also be palpated for tenderness, which in the throwing athlete, can be caused by a stress fracture.18
Examination of the lateral region of the elbow begins with palpation of the lateral epicondyle. Tenderness directly over the epicondyle is consistent with lateral epicondylitis; tenderness directly over the anconeus soft spot can indicate a symptomatic lateral plica, a condition that is commonly found in throwing athletes. In one study, this was the most reproducible finding in a group of patients who were treated for this condition.19
Range of motion should be assessed for elbow flexion and extension and for forearm supination and pronation, as well as the nature of the extension and flexion end points. Cain and associates describe the “end feel” at the extremes of motion in the physical examination of the throwing athlete.3 Normal extension terminates in the firm sensation of the posterior bony articulation making contact in the olecranon fossa, and normal flexion terminates in the abutment of the soft tissues of the distal humerus and the proximal forearm. Variations in the normal end points, particularly a bony end feel in extension, can indicate pathology such as posterior osteophytes. The examiner should focus on the end feel at extension and not necessarily on motion itself. Elbow flexion contractures have been detected in up to 50% of professional pitchers, and they do not necessarily indicate injury.
To perform the valgus stress test, the patient’s distal forearm is placed under the examiner’s axilla as a valgus load is applied to the elbow in 30 degrees of flexion (Fig. 13-2). The absence of a distinct end point combined with pain or tenderness indicates a positive test result and insufficiency of the anterior band of the anterior bundle of the medial collateral ligament (MCL).
The moving valgus stress test, as described by O’Driscoll,20 is performed with the patient in an upright position and the shoulder abducted 90 degrees (Fig. 13-3). Starting with the elbow in full flexion and the shoulder in maximal external rotation, the elbow is quickly extended while a constant valgus torque is maintained. For an examination result to be positive, the pain generated by the maneuver must reproduce the medial elbow pain that the patient has with activities, and the pain should be maximal between the position of late cocking (120 degrees) and early acceleration (70 degrees) as the elbow is extended.
Other relevant tests of the throwing athlete include the radiocapitellar compression test for osteochondritis dissecans of the radiocapitellar joint, the clunk test for posterior olecranon impingement, and the flexion-pronation test to detect a symptomatic snapping lateral plica. The radiocapitellar compression test is performed by placing the elbow in full extension and loading the joint with supination and pronation to produce mechanical symptoms. The clunk test for posterior olecranon impingement stabilizes the upper arm and brings the elbow into extension to produce posterior elbow pain (Fig. 13-4). The flexion pronation test is performed by placing the arm in maximum pronation and then passively flexing the elbow to approximately 90 degrees, which causes snapping in a positive test.19
Diagnostic Imaging
The routine preoperative radiographic evaluation of the elbow includes anteroposterior, lateral, and oblique views. Stress views may be helpful in assessing ligamentous laxity, and olecranon axial views at 110 degrees of flexion may reveal posteromedial osteophytes in valgus extension overload syndrome. However, it has been our experience that a true lateral view of the elbow in hyperflexion is adequate to diagnose posteromedial osteophytes. Contralateral comparison imaging studies of the elbow are helpful when evaluating elbow joint laxity and when trying to distinguish true growth disturbances from variant ossification centers in the pediatric population. Computed tomography can be helpful when trying to assess suspected bony pathology, including stress fractures and avulsion fractures.
Magnetic resonance imaging (MRI) remains the gold standard for evaluating pathology of the soft tissues about the elbow, including ligamentous injury, tendinopathy, and lesions of the articular cartilage. The accuracy of MRI in the evaluation of subtle MCL injuries and the role of arthrography and contrast remain controversial. At our institution, we use a noncontrast MRI with specially designed sequences (Fig. 13-5). Potter and colleagues demonstrated a high sensitivity and specificity for MRI in detecting ligamentous, soft tissue, and cartilaginous injuries.21–23 This technique maintains the minimally invasive nature of the test and limits cost. A major additional advantage is excellent visualization of the articular cartilage in a highly specific and sensitive manner.24
TREATMENT
Indications and Contraindications
Arthroscopy is an important method used for the diagnosis and treatment of valgus extension overload, with careful consideration given to choosing the appropriate indications. When valgus overload injury results in disabling symptoms for the athlete, surgical reconstruction of the anterior band of the ulnar collateral ligament may be indicated. Further indications for elbow arthroscopy in the throwing athlete include removal of loose bodies, excision of olecranon osteophytes, synovectomy, capsular release, capsular contracture, débridement of impinging osteophytes, articular cartilage lesions addressed, and the assessment and treatment of osteochondritis dissecans of the capitellum.25–28
The primary contraindication to elbow arthroscopy is any change in the normal bony or soft tissue anatomy that precludes safe entry of the arthroscope into the elbow joint.29 We do not recommend performing arthroscopy when there has been a previous ulnar nerve transposition or when adequate distention of the joint cannot occur. Arthroscopy is contraindicated if there is soft tissue infection in the area of the portal sites.
The surgeon should have a comprehensive understanding of the surrounding anatomy and advanced technical experience of arthroscopic technique. Attention to detail is essential to prevent compromise of the surrounding neurovascular structures or damage to the delicate articular cartilage.30
Conservative Management
Athletes who fail conservative management are candidates for surgery. It is not uncommon for throwing athletes to have myriad pathologies that require arthroscopic treatment and open MCL reconstruction. In addition to our aforementioned criteria for arthroscopic management of valgus extension overload, we perform a MCL reconstruction concomitantly based on the following criteria: MRI evidence of MCL injury; a history of medial elbow pain in the region of the MCL that develops during the late cocking and early acceleration phase; and pain that is severe enough to prevent the athlete from an acceptable level of competition.
Arthroscopic Technique
Patient Positioning
The prone position, first described by Poehling and coworkers,31 places the patient prone on chest rolls with the arm stabilized by an arm holder and allowed to hang off the table. The shoulder is abducted to 90 degrees, and the elbow is flexed to 90 degrees. Some surgeons prefer this position because it eliminates the need for traction, places the elbow in a more stable position, and allows easier access to the posterior aspect of the joint.26,31 If necessary, this position allows conversion from arthroscopy to an open surgical procedure, but we have found this to be very difficult.31 Disadvantages of the prone position include general anesthesia and poor access to the airway by the anesthesiologist.
The lateral decubitus position, originally described by O’Driscoll and Morrey,32 has advantages similar to those of the prone position, including improved arm stability and posterior joint access. However, in the lateral decubitus position, the anesthesiologist’s access to the airway is not compromised. The main disadvantage is that access to the anterior compartment may require repositioning by placing the patient in a lateral position with the shoulder flexed forward at 90 degrees over a padded bolster.
The supine-suspended position, originally described by Andrews and Carson,25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree