CHAPTER 23 Arthroscopy for Symptomatic Hip Arthroplasty
Surgical technique
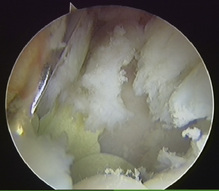
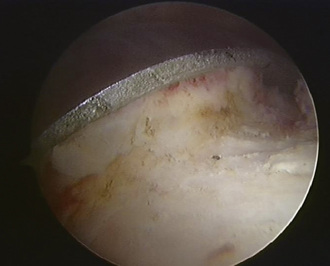
Standard lateral paratrochanteric and anterior paratrochanteric portals are made to access the central compartment; this allows for the visualization of the edge of the acetabular component, the bone–component interface (Figure 23-1), and the synovial membrane, and the surgeon is also able to look for any possible metallosis. If debridement is required, it is performed with an arthroscopic shaver or a radiofrequency probe. Synovial biopsy and further aspirates from the bone implant interface may also be obtained at this time.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree