Arthroscopy and Management of Ankle Fractures
Beat Hintemann
Despite having adequate open reduction and internal fixation, ankle fractures may still be associated with poor clinical outcomes (1, 2, 3 and 4). Residual problems such as chronic pain, arthrofibrosis, recurrent swelling, and perceived instability continue to occur unpredictably after ankle fractures. The cause of such poor outcomes is unclear, yet may be related to occult articular trauma (5, 6, 7 and 8). The use of arthroscopy allowed comprehensive evaluation of the pattern and extent of articular injury associated with acute ankle fractures (9, 10, 11 and 12).
SURGICAL TECHNIQUE
The operative procedure is performed under general, spinal, or epidural anesthesia. The patient is positioned supine with a padded bolster placed under the ipsilateral pelvis. The knee is flexed to about 70° using the knee holder, which allows the foot to hang free. No distraction device is used for the ankle. Following sterile preparation, surface anatomy is carefully outlined. In the swollen ankle, more care is necessary to delineate the important structures. To avoid iatrogenic lesions of the soft tissues and articular cartilage, the joint is first inflated with saline, and the portals are created by blunt dissection. The anterior approach at the lateral border of the anterior tibial tendon is used to insert the 4.5- or 2.7-mm, 30° arthroscope. If necessary, accessory anteromedial or anterolateral portals are used for the insertion of instruments. After having copiously irrigated the joint, the joint is inspected systematically (13).
Arthroscopic Assessment
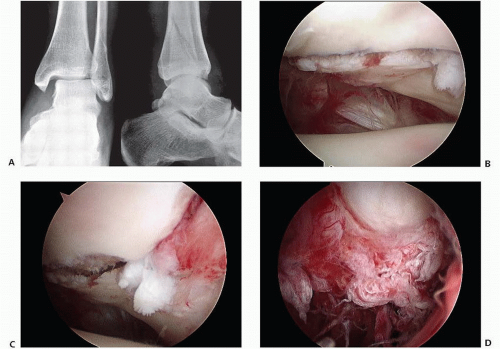
Chondral lesions are carefully assessed with regard to extent and severity, and graded as described by Outerbridge (14). Unstable chondral flaps are debrided, and free osteochondral fragments are removed. Articular surface lesions and intra-articular ligament integrity and syndesmosis stability are evaluated (Fig. 91.1).
Arthroscopic Reduction and Internal Fixation
The use of arthroscopic reduction and internal fixation (ARIF) is surgeon dependent. Reported indications for ARIF include transchondral talar dome fracture, talar fracture, low-grade fracture of the distal tibia, syndesmotic disruption, malleolar fracture, and chronic pain following definitive management of fracture about the ankle. Among the potential benefits are less extensive exposure, preservation of blood supply, and improved visualization of the pathology.
Percutaneous manipulation of fracture fragments under direct visualization is performed using fluoroscopy as needed. If arthroscopically assisted reduction of the medial malleolus or distal tibia fracture is successful, cannulated screw fixation under fluoroscopy control is undertaken without open exposure of the fracture site. If the fracture morphology precludes arthroscopic reduction, open reduction and fixation (ORIF) are then performed. This is typically the case for a fracture of the fibula.
Postoperative Care
Postoperatively, the ankle is routinely immobilized in a posterior splint until swelling-down and safe wound-healing. Thereafter, the patients are kept in a cast or a walker for a minimum of 6 weeks following surgery with a period of 4 to 6 weeks of partial weight-bearing immobilization, and additional 2 or more weeks of weight-bearing immobilization.
RESULTS
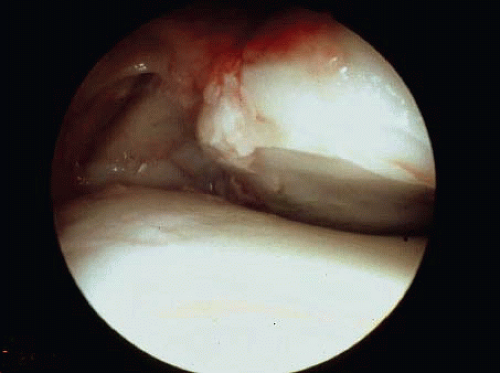
With the studies available, arthroscopy was found to be a valuable tool in acute ankle fractures in identifying and managing intra-articular damage that otherwise remain unrecognized (Fig. 91.2) (9, 10, 11, 12 and 13). Arthroscopy also provides prognostic information regarding the outcome (4). A relative contraindication to arthroscopy is important soft-tissue damage associated with fracture-dislocation because of the risk related to fluid extravasation.
Chondral Lesions
In general, chondral lesions (Fig. 91.3) were found more often than expected (Table 91.1).
Hintermann et al., (11) in a prospective study on 288 patients, first reported on arthroscopic findings in acute ankle fractures. They found a 79% rate of articular lesions. The frequency and severity of chondral lesions increased from type-B to type-C ankle fractures (P < .05), as classified with use of the AO-Danis-Weber criteria, but there was no difference between type-A and type-B fractures with regard to the frequency and severity of chondral lesions. There were more lesions in men than in women, and
in general, they were more severe in men (P < .05). They also tended to be worse in patients under 30 years and in those older than 60 years. Within each type of fracture, the lesions increased from subgroups 1 to 3 (P < .05).
in general, they were more severe in men (P < .05). They also tended to be worse in patients under 30 years and in those older than 60 years. Within each type of fracture, the lesions increased from subgroups 1 to 3 (P < .05).
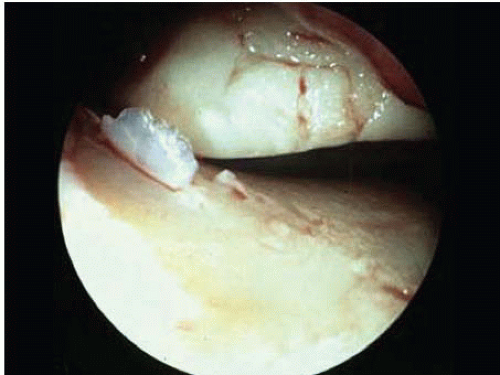 FIGURE 91.3. Besides osseous instability with incongruency, arthroscopy reveals extended lesions to articular surface (a 48-year-old female patient after PER injury). |
Table 91.1 Amount and localization of chondral lesions | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree