Arthroscopically Assisted Posterior Cruciate Ligament Reconstruction
Gregory C. Fanelli
Craig J. Edson
Kristin N. Reinheimer
The incidence of posterior cruciate ligament (PCL) injuries is reported to be from 1% to 40% of acute knee injuries. This range depends on the patient population reported, and is approximately 3% in the general population and 38% in reports from regional trauma centers (1,6,13). Our practice at a regional trauma center has a 38.3% incidence of PCL tears in acute knee injuries, and 56.5% of these PCL injuries occur in multiple trauma patients. Of these, 45.9% are combined anterior cruciate ligament (ACL)/PCL tears, whereas 41.2% are PCL/posterolateral corner tears. Only 3% of acute PCL injuries seen in our practice are isolated.
This chapter illustrates the senior author’s surgical techniques for the arthroscopic single-bundle-single-femoral tunnel, and double-bundle-double-femoral tunnel, transtibial PCL reconstruction surgical procedure. We will also present the Fanelli Sports Injury Clinic 2-to 10-year results of PCL reconstruction using these surgical techniques. The information presented in this chapter has also been presented elsewhere, and the reader is referred to these sources for additional information regarding this topic (2,3,4,5,7,8,9,10,11,12,13,14,15,16,17,18,19,20,22,23).
The single-bundle-single-femoral tunnel transtibial tunnel PCL reconstruction is an anatomic reconstruction of the anterolateral bundle of the PCL. The anterolateral bundle tightens in flexion, and this reconstruction reproduces that biomechanical function. While the single-bundle-single-femoral tunnel transtibial tunnel PCL reconstruction does not reproduce the broad anatomic insertion site of the normal PCL, there are certain factors that lead to success with this surgical technique:
Identification and treatment all pathology (especially posterolateral and posteromedial instability)
Accurate tunnel placement
Anatomic graft insertion sites
Strong graft material
Minimal graft bending
Final tensioning at 70 to 90 degrees of knee flexion
Graft tensioning
Arthrotek mechanical tensioning device
Primary and back-up fixation
Appropriate rehabilitation program
INDICATIONS/CONTRAINDICATIONS
Indications
Our indications for surgical treatment of acute PCL injuries include insertion site avulsions, tibial step-off decreased 6 tolO mm or greater, and PCL tears combined with other structural injuries. Our indications for surgical treatment of chronic PCL injuries are when an isolated PCL tear becomes symptomatic demonstrated by progressive functional instability.
Contraindications
There are no significant contraindications.
PREOPERATIVE PLANNING
History and Physical Examination
The typical history of a patient with a PCL injury includes a direct blow to the proximal tibia with the knee in 90 degrees of flexion. Hyperflexion, hyperextension, and a direct blow to the proximal medial or lateral tibia in varying degrees of knee flexion, as well as a forced varus or valgus force, will induce PCL-based multiple ligament knee injuries.
Physical examination of the injured knee compared with the noninjured knee reveals decreased tibial step-offs, and a positive posterior drawer test. Since isolated PCL tears are rare, collateral ligament injury is common (posterolateral and posteromedial corner injuries), and posterolateral and posteromedial drawer tests, dial tests, external rotation recurvatum tests, varus and valgus laxity, and even anterior laxity may be present.
Isolated Posterior Cruciate Ligament Injury Diagnostic Features
Abnormal posterior laxity less than 5 mm
Abnormal posterior laxity decreases with tibial internal rotation
No abnormal varus
Abnormal external rotation of the tibia on the femur less than 5 degrees compared with the uninvolved side tested with the knee at 30 and 90 degrees knee flexion.
Posterior Cruciate Ligament/PLC Injury Diagnostic Features
Abnormal posterior laxity greater than 5 to 10 mm
Abnormal varus rotation at 30 degrees knee flexion is variable and depends on the posterolateral instability grade.
Abnormal external rotation thigh foot angle test greater than 10 degrees compared with the normal lower extremity tested at 30 and 90 degrees of knee flexion. (If you can see the difference, then PLI exists.)
Posterolateral drawer-positive
Combined Anterior Cruciate Ligament/Posterior Cruciate Ligament Injuries Diagnostic Features
Grossly abnormal anterior-posterior tibial-femoral laxity at both 25 and 90 degrees of knee flexion
Positive Lachman and pseudo-Lachman tests
Positive pivot-shifting phenomenon
Negative tibial step-off (posterior sag)
Increased varus-valgus laxity in full extension
Imaging Studies
Plain radiographs used to evaluate PCL injuries include the following views: anterior-posterior weight bearing both knees, 30-degree flexion lateral, intercondylar notch, 30-degree axial of the patellas, and stress views at 90 degrees of knee flexion of both knees. Magnetic resonance imaging (MRI) is helpful in acute cases; however, we have found MRI to be less beneficial in chronic PCL injuries. Bone scan is used in chronic cases of PCL instability presenting with pain to define early degenerative joint disease.
SURGERY
Patient Positioning and Initial Setup
The patient is positioned on the operating table in the supine position, and the surgical and nonsurgical knees are examined under general or regional anesthesia. A tourniquet is applied to the operative extremity, and the surgical leg is prepped and draped in a sterile fashion. Allograft tissue is prepared before beginning the surgical procedure, and autograft tissue is harvested prior to beginning the arthroscopic portion of the procedure. The arthroscopic instruments are inserted with the inflow through the superior lateral patellar portal, the arthroscope in the inferior lateral patellar portal, and the instruments in the inferior medial patellar portal. The portals are interchanged as necessary. The joint is thoroughly evaluated arthroscopically, and the PCL is evaluated using the three-zone arthroscopic technique (17). The PCL tear is identified, and the residual stump of the PCL is debrided with hand tools and the synovial shaver.
Initial Incision
An extra capsular posteromedial safety incision approximately 1.5 to 2.0 cm long is created (Fig. 18-1). The crural fascia is incised longitudinally, taking precautions to protect the neurovascular structures. The interval is developed between the medial head of the gastrocnemius muscle and the posterior capsule of the knee joint, which is anterior. The surgeon’s gloved finger is positioned so that the neurovascular structures are posterior to the finger, and the posterior aspect of the joint capsule is anterior to the surgeon’s finger. This technique enables the surgeon to monitor surgical instruments, such as the over-the-top PCL instruments and the PCL/ACL drill guide, as they are positioned in the posterior aspect of the knee. The surgeon’s finger in the posteromedial safety incision also confirms accurate placement of the guidewire prior to tibial tunnel drilling in the medial-lateral and proximal-distal directions (Fig. 18-2). This is the same anatomic surgical interval that is used in the tibial inlay posterior approach.
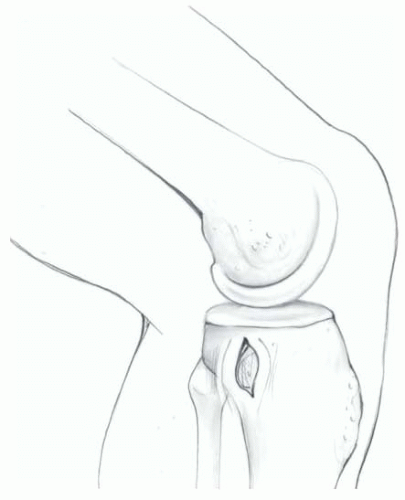 FIGURE 18-1 Posteromedial extra-articular extracapsular safety incision. (Redrawn from Arthrotek, Inc., Warsaw, Indiana, with permission.) |
Elevating the Posterior Capsule
The curved over-the-top PCL instruments are used to carefully lyse adhesions in the posterior aspect of the knee, and to elevate the posterior knee joint capsule away from the tibial ridge on the posterior aspect of the tibia. This capsular elevation enhances correct drill guide and tibial tunnel placement (Fig. 18-3).
Drill Guide Positioning
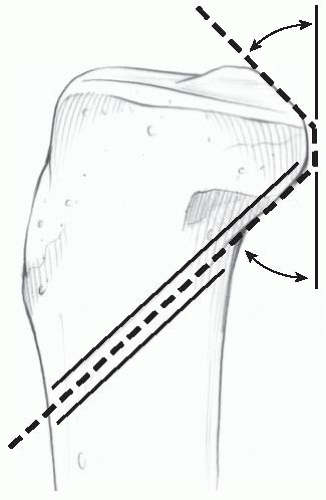
The arm of the Arthrotek Fanelli PCL-ACL Drill Guide is inserted into the knee through the inferior medial patellar portal and positioned in the PCL fossa on the posterior tibia (Fig. 18-4). The bullet portion of the drill guide contacts the anterior medial aspect of the proximal tibia approximately 1 cm below the tibial tubercle, at a point midway between the tibial crest anteriorly and the posterior medial border of the tibia. This drill guide positioning creates a tibial tunnel that is relatively vertically oriented and has its posterior exit point in the inferior and lateral aspect of the PCL tibial anatomic insertion site. This positioning creates an angle of graft orientation such that the graft will turn two very smooth 45-degree angles on the posterior aspect of the tibia, eliminating the “killer turn” of 90-degree graft angle bending (Fig. 18-5).
The tip of the guide in the posterior aspect of the tibia is confirmed with the surgeon’s finger through the extra capsular posteromedial safety incision (see Fig. 18-2). Intraoperative anteroposterior and lateral radiographs may also be used, as well as arthroscopic visualization to confirm drill guide and guide pin placement. A blunt spade-tipped guidewire is drilled from anterior to posterior and can be visualized with the arthroscope, in addition to being palpated with the finger in the posteromedial safety incision. We consider the finger in the posteromedial safety incision the most important step for accuracy and safety.
 FIGURE 18-3 Posterior capsular elevation using the Arthrotek PCL instruments. (Redrawn from Arthrotek, Inc., Warsaw, Indiana, with permission.) |
Tibial Tunnel Drilling
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree