Arthroscopic Treatment of Shoulder Fractures
Jesus Rey II
Sumant G. Krishnan
The appropriate management of shoulder fractures remains challenging. Therapeutic options for shoulder fractures include both conservative and surgical treatments. Indications for either treatment remain controversial and are often made based on surgeon experience rather than evidence-based algorithms. In recent years, the treatment of shoulder girdle fractures has evolved from extensive open reduction to minimally invasive surgery. Arthroscopy is increasingly being recognized as an important adjunct in treating periarticular fractures, especially to confirm accurate reduction of articular surfaces. Avoidance of large muscular dissections is attractive for potentially decreasing complications, reducing postoperative pain, enhancing healing potential, and shortening postoperative recovery time. These arthroscopic techniques also allow for complete joint inspection and more accurate assessment of concomitant injuries than conventional methods. Given the high incidence of associated injuries with proximal humerus fractures, arthroscopy may indeed be a useful diagnostic and treatment tool for associated labral lesions, rotator cuff injuries, and traumatic cartilage defects (1). However, the arthroscopic treatment of shoulder fractures requires a learning curve that depends on surgeon experience in shoulder arthroscopy. Long-term outcomes after all-arthroscopic management of shoulder fractures still remain elusive.
PROXIMAL HUMERUS FRACTURES
Overview
Proximal humerus fractures represent 4% to 5% of all fractures and are the most common fractures of the shoulder girdle. Nordqvist and Petersson, (2) in a review of all fractures treated in a single hospital during the course of a year, found that proximal humerus fractures accounted for 53% of all significant shoulder girdle injuries.
Greater and lesser tuberosity fractures can occur as isolated injuries or as a component of comminuted proximal humerus fractures. Despite the disagreement in the literature regarding the magnitude of displacement, when isolated, most authors advocate that 5 mm of posterosuperior displacement of the greater tuberosity can lead to clinically significant impingement. With nondisplaced or minimally displaced (less than 5 mm) fractures, conservative management is an option (3). Management and outcomes for lesser tuberosity fractures are even more controversial since the incidence of this injury is far less common.
Clinical Evaluation
Pertinent History
The clinical history for proximal humerus fractures varies based upon which pattern of fracture is present. Although most of these fractures result from low-energy trauma usually following a fall in an elderly individual, isolated greater or lesser tuberosity fractures occur in younger patients. Tuberosity fractures usually occur in male patients between the second and the fifth decades of life (4) as well as adolescents with open humeral physis (5).
The mechanism of injury plays an important role in the pattern of fracture. It has been shown that over 50% of greater tuberosity fractures occur in the setting of an anterior shoulder dislocation (6). Eccentric loads on the tuberosities sustained by falling onto an outstretched arm can produce an avulsion-type fracture or propagate it with subsequent displacement. Lesser tuberosity fractures represent a rare injury that occurs in younger individuals. The arm is usually placed in an abducted and externally rotated position. Forceful contraction of the subscapularis muscle avulses the tuberosity. Another mechanism for lesser tuberosity fractures is a posterior dislocation of the shoulder.
Physical Examination
Acutely, the shoulder is often extremely swollen after a proximal humeral fracture. Ecchymosis tracks down the arm and into the chest and axilla. As most patients with proximal humeral fractures are elderly, assessment for concomitant injuries is paramount.
Electromyographic evaluation has demonstrated that approximately two-thirds (67%) of all patients with proximal humeral fractures suffer acute neurologic injury from
the violence of the injury. Most commonly, this involves either the axillary nerve (58%) or the suprascapular nerve (48%) (7).
the violence of the injury. Most commonly, this involves either the axillary nerve (58%) or the suprascapular nerve (48%) (7).
For isolated lesser tuberosity fractures, symptoms include pain with passive external rotation, pain with resisted internal rotation, and tenderness over the lesser tuberosity. Since the subscapularis tendon is attached to the fractured bony structure, insufficiency of the musculotendinous unit of the subscapularis muscle is present and lift-off and belly-press tests can be used to evaluate this pathology.
Imaging
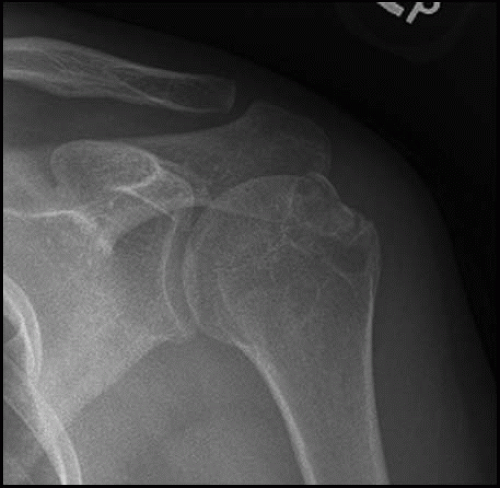
Imaging is paramount in evaluating the proximal humerus fracture. Initial radiographic evaluation consists of a Neer trauma series with anteroposterior (AP), scapular “Y” and axillary roentgenographic views (Fig. 21.1). Because of the anatomy of the proximal humerus, it may be difficult to appreciate fracture lines and fragment displacement. If plain radiographs do not offer adequate visualization, the use of computed tomographic scans with three-dimensional (3D) reconstructions can be extremely helpful in assessing fracture pattern (Fig. 21.2). For fractures involving the greater tuberosity, it has been demonstrated that the most accurate displacement measurements are determined from the AP view in external rotation and the AP view with 15° caudal tilt (8). Displaced large lesser tuberosity fragments can usually be visualized on the AP images, whereas smaller fragments are better visualized on the axillary view.
MRI can detect occult nondisplaced fractures of the tuberosities. Zanetti et al (9). reported a 38% prevalence of occult fractures of the greater tuberosity in patients suspected of having traumatic rotator cuff tears.
Classification
Neer’s four-part classification system of proximal humerus fractures has endured by virtue of its simplicity. Despite its poor interobserver reliability and intraobserver reproducibility, this classification allows a conceptual understanding of the fracture pattern by defining the fracture into separate parts.
Treatment
Nonoperative
Associated injuries, appropriate rehabilitation, and premorbid function may affect the final outcome once nonsurgical management has been established.
Good to excellent results have been reported with nondisplaced and minimally displaced greater tuberosity fractures (10). Every orthopedic surgeon should be mindful that patients who have persistent late pain after a greater tuberosity fracture treated conservatively may have rotator cuff injuries which should be evaluated and treated accordingly (11). Patients with lesser tuberosity fractures without significant displacement of the bony fragment can successfully be treated conservatively.
Operative Indications
Evidence-based indications for the operative management of proximal humeral fractures are based on various factors: fracture pattern, patient age, bone quality, medical comorbidities, level of activity, hand dominance, motivation for recovery, and timing from injury to evaluation. Despite objective evaluation parameters, surgeon experience in operatively managing these technically demanding and challenging injuries often supersedes all and plays the key role in decision making. The rationale for surgical
fixation of greater tuberosity fractures is prevention of nonunion, impingement, or mechanical blockage to abduction by a malpositioned tuberosity. The healing of the tuberosity in a malpositioned location alters the insertion of the rotator cuff tendons with subsequent weakness due to altered biomechanics.
fixation of greater tuberosity fractures is prevention of nonunion, impingement, or mechanical blockage to abduction by a malpositioned tuberosity. The healing of the tuberosity in a malpositioned location alters the insertion of the rotator cuff tendons with subsequent weakness due to altered biomechanics.
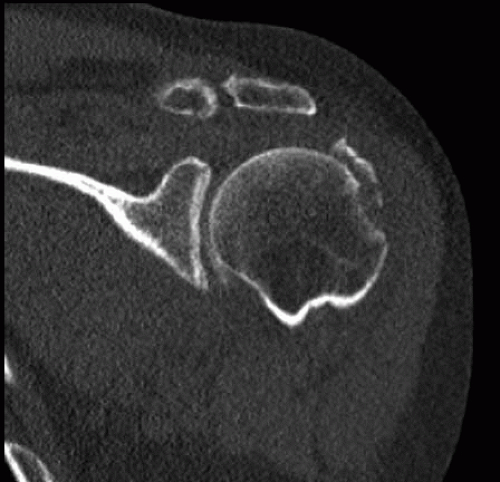 FIGURE 21.2. Coronal CT image of the same patient showing the comminuted pattern of the greater tuberosity fracture. |
Displacement of greater than 5 mm should be reduced surgically. For athletes and patients involved in overhead labor, fixation of even smaller displacements (3 mm) has been advocated.
Operative management of isolated lesser tuberosity fractures presents unique issues. Fixation techniques include heavy sutures, cannulated screws, cerclage wires, and all-arthroscopic suture anchor fixation. When these injuries are chronic, there is usually fibrous tissue interposed, which requires debridement to allow for bony healing to occur. Attention should be paid to the long head of the biceps tendon as well as the subscapularis tendon insertion as there is an intimate relationship between these structures. The superior glenohumeral ligament/coracohumeral ligament complex (pulley system) can be involved and destabilize the biceps tendon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree