CHAPTER 26 ![]() Arthroscopic treatment of posterior instability—surgical technique
Arthroscopic treatment of posterior instability—surgical technique
 In athletics, recurrent posterior subluxation of the shoulder is due to repetitive microtrauma in a variety of arm positions, most commonly leading to posterior capsular attenuation and labral tear.
In athletics, recurrent posterior subluxation of the shoulder is due to repetitive microtrauma in a variety of arm positions, most commonly leading to posterior capsular attenuation and labral tear. One of the most common patient complaints in recurrent posterior shoulder instability is often ambiguous and diffuse shoulder pain. This is common in young, athletic patients who may present with a diagnostic dilemma—suspect posterior instability.
One of the most common patient complaints in recurrent posterior shoulder instability is often ambiguous and diffuse shoulder pain. This is common in young, athletic patients who may present with a diagnostic dilemma—suspect posterior instability. A number of specialized physical examination tests have been devised to specifically elucidate posterior and posteroinferior capsulolabral pathology in the shoulder, including the jerk test, Kim test, modified load and shift test and sulcus test.
A number of specialized physical examination tests have been devised to specifically elucidate posterior and posteroinferior capsulolabral pathology in the shoulder, including the jerk test, Kim test, modified load and shift test and sulcus test. Specific magnetic resonance arthrogram findings indicative of posterior shoulder instability include posterior translation of the humeral head relative to the glenoid, posterior labrocapsular avulsion, posterior labral tear or splitting, discrete posterior capsular tears or rents, reverse humeral avulsion of the glenohumeral ligaments, posterior labrum periosteal sleeve avulsion, increased osseous and chondrolabral retroversion, and subscapularis tendon avulsion.
Specific magnetic resonance arthrogram findings indicative of posterior shoulder instability include posterior translation of the humeral head relative to the glenoid, posterior labrocapsular avulsion, posterior labral tear or splitting, discrete posterior capsular tears or rents, reverse humeral avulsion of the glenohumeral ligaments, posterior labrum periosteal sleeve avulsion, increased osseous and chondrolabral retroversion, and subscapularis tendon avulsion. Posterior glenohumeral stabilization is done via an anatomic-based arthroscopic approach, which allows for enhanced identification and repair of posterior capsular laxity, complete or incomplete detachment of the posterior capsulolabral complex, and inferior capsular tears.
Posterior glenohumeral stabilization is done via an anatomic-based arthroscopic approach, which allows for enhanced identification and repair of posterior capsular laxity, complete or incomplete detachment of the posterior capsulolabral complex, and inferior capsular tears. The authors’ preferred surgical treatment of recurrent unidirectional posterior subluxation of the shoulder is an arthroscopic posterior capsulolabral repair with suture anchors. When a patulous posterior capsule or a posteroinferior component of instability is also present, an arthroscopic superiorly directed capsular shift and capsular plication is added.
The authors’ preferred surgical treatment of recurrent unidirectional posterior subluxation of the shoulder is an arthroscopic posterior capsulolabral repair with suture anchors. When a patulous posterior capsule or a posteroinferior component of instability is also present, an arthroscopic superiorly directed capsular shift and capsular plication is added.Introduction
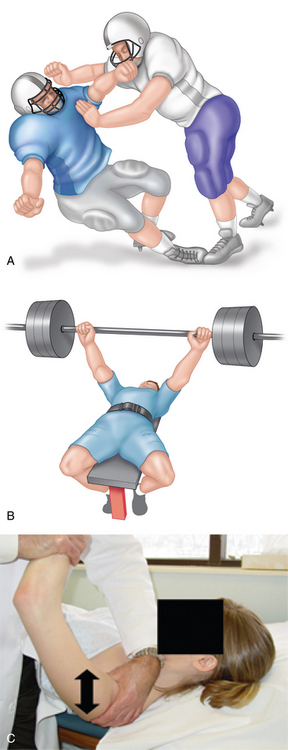
In comparison with anterior shoulder instability, posterior instability is uncommon, occurring in 2% to 10% of cases.1–5 A posteriorly directed blow to an adducted, internally rotated and forward-flexed upper extremity is classically described as the sentinel traumatic event.6 However, recurrent or locked posterior shoulder dislocations from macrotrauma are exceedingly rare in the athletic population.2,7 Instead, athletes typically present with posterior shoulder instability secondary to repetitive microtrauma, which can occur in multiple arm positions and under a variety of loading conditions. In 1952, McLaughlin first acknowledged the existence of a wide clinical spectrum of posterior shoulder instability, ranging from locked posterior dislocation to the often subclinical recurrent posterior subluxation (RPS).2
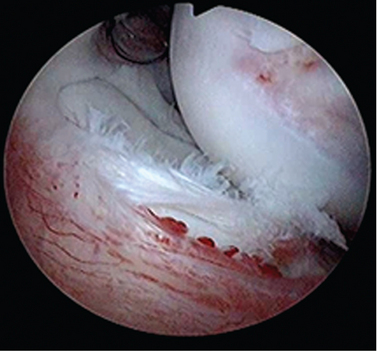
In athletics, RPS has been observed in weight lifters, football lineman, golfers, tennis players, butterfly and freestyle swimmers, overhead throwers and baseball hitters, among others.8–10 The etiology of RPS is repetitive microtrauma, most commonly leading to posterior capsular attenuation and labral tear (Figs. 26-1 to 26-3). Regardless of the sport, athletes with RPS often present with ambiguous complaints of diffuse pain and shoulder fatigue, without distinct injury, often making it challenging to elucidate the underlying pathology and diagnosis.
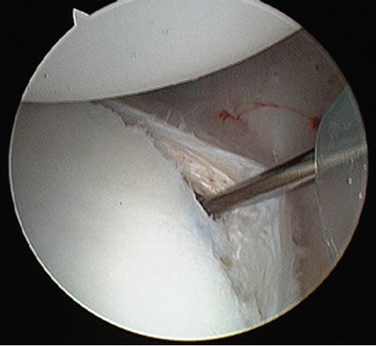
FIGURE 26-1 Posterior labral tear from the glenoid (right shoulder, viewed from the anterior portal).
A thorough history and physical examination, coupled with specific imaging studies, are required to determine the exact pathogenesis of and appropriate treatment options for RPS. With increased clinical awareness, imaging advances such as the magnetic resonance arthrogram (MRA), and the development of specific provocative physical examination tests, the identification of RPS in the athletic population is improving. Several variables that must be considered during the workup include mechanism of injury (true posterior traumatic dislocation versus repetitive microtrauma versus an acute or chronic subluxation), specific direction of instability (posterior versus posteroinferior or posterosuperior), and the pattern of instability (unidirectional or multidirectional) because these factors will ultimately affect treatment and outcome.11
Successful treatment of RPS begins with thorough identification of all of the structural abnormalities present in the affected shoulder, which can include any combination of the labrum, capsule, supporting ligaments, and rotator cuff. Over time, posterior glenohumeral stabilization has evolved from various open procedures to an anatomic-based arthroscopic approach, which allows for enhanced identification and repair of intra-articular pathology including posterior capsular laxity, complete or incomplete detachment of the posterior capsulolabral complex, and inferior capsular tears.12 Although postoperative results are generally good to excellent after stabilization for RPS, there is room for improvement. Accordingly, research continues on both the biomechanical and clinical fronts to further refine our diagnostic and treatment approaches to RPS.
History and physical examination
Thorough knowledge of an athlete’s sport, position, and training regimen is critical in deducing the pathogenesis and specific pathology associated with RPS. Based on this information, treatment options may ultimately include labral debridement, labral repair, posterior capsular release, or posterior capsular plication. Pollock et al noted that two thirds of athletes who ultimately required surgery presented with complaints of difficulty using the shoulder outside of sports, particularly with the arm above the horizontal.13 An inquiry also should be made regarding mechanical symptoms because one study found that 90% of patients with symptomatic RPS noted clicking or crepitation with motion.14 Often times this crepitus can be reproduced during examination and is due to discrete posterior capsulolabral pathology.
Physical examination of a shoulder suspected of RPS begins with inspection, focusing on asymmetry, scapular dysrhythmia, and muscular atrophy. A skin dimple over the posteromedial deltoid of both shoulders has been found to be 62% sensitive and 92% specific in correlating with posterior instability.15 Tenderness to palpation as a result of inflammation is next assessed at the posterior glenohumeral joint line, greater tuberosity, and biceps tendon. A majority of patients with posterior instability have been found to have posterior joint line tenderness, likely caused by posterior synovitis or posterior rotator cuff tendinosis secondary to multiple episodes of instability.13
Glenohumeral stability is assessed on both shoulders with the patient supine, and the differences between the two are documented. The “load and shift” maneuver is performed with the arm held in 90 degrees of abduction and neutral rotation.16 In this position, a moderate axial load is applied to the glenohumeral joint in combination first with an anterior force in an attempt to translate the humeral head over the anterior glenoid rim. The test is repeated with a posterior directed force (Fig. 26-4). Anterior and posterior laxity is quantified as 0 for a humeral head that does not translate to the glenoid rim; 1+ for a humeral head that translates to but does not translate over the glenoid rim; 2+ for a humeral head that translates over the glenoid rim, but spontaneously reduces; and 3+ for a humeral head that translates over the glenoid rim and does not spontaneously reduce.
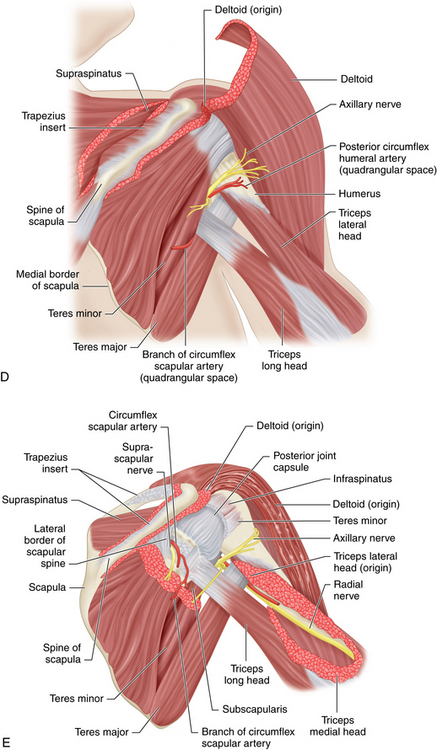
(D and E from Reider B: Operative techniques, sports medicine surgery, Philadelphia, 2010, Saunders, Figs. 10-2 and 10-3.)
Generalized ligamentous laxity also may contribute to MDI and thus should be graded on the 9-point Beighton Scale with the following tests: (1) ability to hyperextend the elbows (1 point for each extremity), (2) ability to passively touch the thumb to the adjacent forearm with the wrist in flexion (1 point for each extremity), (3) ability to passively hyperextend the small finger metacarpophalangeal joint more than 90 degrees (1 point for each extremity), (4) ability to hyperextend the knees (1 point for each extremity) and (5) ability to touch the palms to the floor with feet together (1 point).17 Patients who score 5 points or greater on the Beighton Scale are considered ligamentously lax.
A number of specialized tests have been devised to further elucidate capsulolabral pathology in the shoulder. The jerk test is used to assess posterior stability in the seated position. The medial border of the scapula is stabilized with one hand, and the other hand applies a posteriorly directed force to the 90 degree forward flexed, adducted, and internally rotated arm. The test is positive if posterior subluxation or dislocation of the humeral head occurs while simultaneously reproducing the symptoms of pain and apprehension; variable sensitivity of the jerk test has been reported.7,18,19
The Kim test also can aid in the diagnosis of posterior and posteroinferior shoulder instability.20 With the patient seated, the arm is placed in 90 degrees of abduction in the scapular plane and an axial load is applied. The arm is subsequently forward elevated an additional 45 degrees, and a posteroinferior vector is placed on the glenohumeral joint. Kim et al concluded the test is positive with a sudden onset of posterior subluxation with pain. This test, in combination with the jerk test, was found to be 97% sensitive in detecting a posteroinferior labral lesion. The authors also found that patients who experienced pain with the Kim Test were more likely to require operative intervention to alleviate their symptoms than those who did not experience pain.
In some cases of RPS, particularly those involving overhead throwers, a posterior labral tear is associated with a superior labral tear, resulting in the type VIII superior labrum anterior and posterior (SLAP) tear.21 Accordingly, when examining a shoulder suspected of RPS, the O’Brien’s test for superior labral pathology also should be performed. For this test, the patient is seated and the arm is forward elevated 90 degrees, adducted 10 degrees, and internally rotated with the elbow extended. A downward force is placed on the arm. A positive test is confirmed when pain elicited in this position does not occur in the same position with the arm externally rotated and the same force applied.
Physical examination findings in posterior shoulder instability
Imaging
Three radiographs of the shoulder are routinely obtained for the workup of RPS: (1) an anteroposterior view in the plane of the scapula, (2) an axillary view, and (3) a scapular Y lateral view. In most patients with RPS, radiographic images are normal, although in some cases a posterior glenoid lesion or impaction of anterior humeral head (reverse Hill-Sachs lesion) can be visualized. In rare instances, a fracture of the lesser tuberosity will give evidence to a previous posterior dislocation.22 Additionally, the West Point radiographic view can be useful for detecting fractures of the glenoid rim or subtle ectopic bone formation around the glenoid.23,24
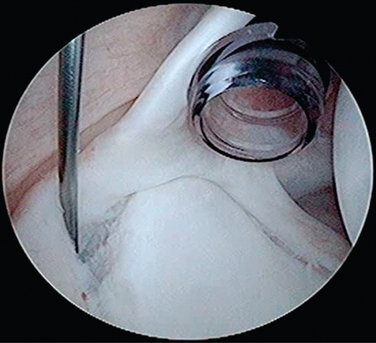
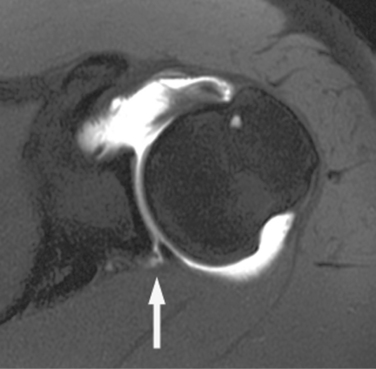
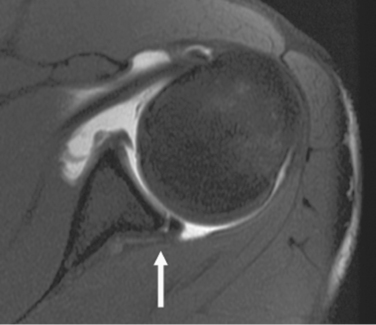
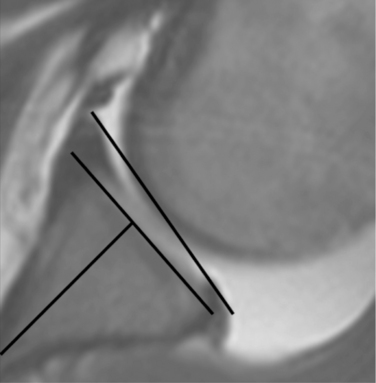
Magnetic resonance arthrogram (MRA) is the most sensitive diagnostic test for identifying lesions of the posterior labrum and capsule.25 Specific MRA findings indicative of posterior shoulder instability include posterior translation of the humeral head relative to the glenoid, posterior labrocapsular avulsion, posterior labral tear or splitting, discrete posterior capsular tears or rents, reverse humeral avulsion of the glenohumeral ligaments (HAGL), posterior labrum periosteal sleeve avulsion (POLPSA), and subscapularis tendon avulsion26,27 (Fig. 26-5). The Kim classification is used to specifically describe posterior labral tear morphology: type I, incomplete detachment; type II (the “Kim lesion”), a concealed complete detachment; type III, chondrolabral erosion; and type IV, flap tear of the posteroinferior labrum28 (Figs. 26-6 to 26-8). The Kim lesion appears arthroscopically as a crack at the junction of the posteroinferior glenoid articular cartilage and labrum, through which a complete detachment of the deeper labrum from the glenoid rim can be identified (see Fig. 26-7).
In further work by Kim et al, 33 shoulders with atraumatic posterior instability were studied with MRA to examine chondrolabral changes.29 In comparison to age-matched normal shoulders, the affected shoulders had a glenoid that was shallower, with more osseous and chondrolabral retroversion present in the middle and inferior glenoid (Fig. 26-9). The study was not able to determine whether these changes were etiologic or pathologic, but nonetheless they should be sought when diagnosing posterior instability of the shoulder. Similar findings were presented in a 2006 study by Bradley et al, in which MRA of 48 shoulders with RPS revealed increased chondrolabral retroversion (10.7 degrees versus 5.5 degrees) and increased glenoid bony retroversion (7.1 degrees versus 3.5 degrees) in comparison to controls.8 More recent data by Bradley et al has revealed that 16 baseball pitchers with RPS examined with MRA had even higher chondrolabral retroversion (11.5 degrees) and glenoid bony retroversion (8.4 degrees).30 Additionally, Tung and Hou found that in 24 patients with RPS, MRA revealed more posterior humeral head translation, posterior labral tears, and posterior labrocapsular avulsions when compared with normal controls.25
As a supplementary test, dynamic MRA can be performed, as discussed previously, to demonstrate labral “peel back” in the ABER position, which is consistent with posterosuperior labral tear.31 This finding has been seen most commonly in the overhead thrower, who often presents with concomitant posterior and superior labral tears in the type VIII SLAP morphology. Last, in our practice the use of CT is limited to cases where a significant amount of bony glenoid retroversion is suspected and an accurate measurement is desired when considering operative intervention.
Nonoperative treatment
A variety of operative and nonoperative treatment methods for posterior shoulder instability have been described. Rehabilitation with an emphasis on strengthening the rotator cuff, posterior deltoid, and periscapular muscles is frequently the first line of treatment and may allow an athlete to return to the preinjury level of sport.13,32–37 It is recommended to maintain this physical therapy protocol for a minimum of 6 months in order to decrease an athlete’s functional disability. Previous studies have reported subjective improvement in up to 70% of athletes with this protocol. Objectively, the RPS is typically not completely eliminated, but the functional disability during athletics is improved sufficiently to allow participation in sport without significant problem. If an athlete is not able to return to the preinjury level of competition, operative treatment is a reasonable option.38,39 Therapy has traditionally been more effective in those patients who have an atraumatic cause of RPS, as opposed to those with generalized ligamentous laxity or who have suffered a discrete traumatic event.32,34
Surgical treatment
Many operative procedures have been described for the treatment of posterior instability. Overall, the results of surgical treatment of posterior instability have been less consistent compared with those for anterior instability, particularly in the overhead thrower.38,40,41 While in general there is a relative paucity of clinical data on attempted posterior shoulder stabilization, the last decade has produced multiple noteworthy studies. Overall, there has been a trend from open to arthroscopic repair and from nonanatomic to anatomic reconstruction. However, multiple confounding variables make the literature difficult to compare, including differing causes of instability (RPS versus traumatic dislocation), patterns of instability (unidirectional posterior versus MDI), surgical techniques (open versus arthroscopic), patient populations (athletic versus nonathletic, throwers versus nonthrowers), postoperative rehabilitation protocols, postoperative functional demands (return to work, sport or neither) and definitions of clinical success and failure.
Historically, multiple open procedures for posterior shoulder stabilization have been performed, involving patients of wide demographics, variable patterns of instability, and differing levels of athletic competition. These have included the reverse Putti-Platt procedure, biceps tendon transfer, subscapularis transfer, infraspinatus advancement, posterior opening glenoid wedge osteotomy, proximal humeral rotational osteotomy, bone block augmentation of the posterior glenoid or acromion, posterior staple capsulorrhaphy, allograft reconstruction, capsulolabral reconstruction, and open capsular shift.2,7,,32,37,38,41–54 Scapinelli found that 10 shoulders that underwent an inverted scapular spine bone graft to the posterior border of the acromion to treat recurrent posterior shoulder instability resulted in 100% success at 9.5 year follow-up.50 Notable soft tissue tightening procedures have included the reverse Putti-Platt procedure and the Boyd and Sisk procedure of rerouting the long head of the biceps tendon to the posterior glenoid.51,52 In 1980, Neer et al reported good results in their description of a laterally based posterior capsular shift to tighten a patulous posteroinferior capsule.53 Similarly, multiple authors have attempted a medially based posterior capsular shift for posterior capsular tightening.32,37,38 Misamore et al reported on 14 patients with traumatic unidirectional posterior instability treated with an open posterior capsulorrhaphy and evaluated at a mean 45-month follow-up.37 Based on Rowe grading criteria, 13 of 14 patients were found to have excellent results and 12 of 14 returned to their preinjury level of athletic competition.
In further pursuit of anatomic-based repair, Rhee et al presented a review of 33 shoulders that underwent an open, deltoid-saving posterior capsulolabral reconstruction for recurrent posterior instability.45 At a 25-month follow-up, 4 patients (13.3%) had recurrent instability. Wolf et al presented similar findings in a retrospective review on 44 shoulders after open posterior glenohumeral stabilization; the recurrence rate was 19%, with patients older than 37 years and those with chondral damage having poor results.44
Due to interest in minimizing iatrogenic surgical trauma, arthroscopic techniques have been implemented with gaining popularity for the treatment of shoulder instability. Arthroscopic thermal capsulorrhaphy has been used in the treatment of shoulder instability with mixed results. Bisson presented results of 14 shoulders with unidirectional posterior instability without labral detachment that were treated with thermal capsulorrhaphy; 3 patients (21%) were found to have failure at a 2-year follow-up.55 D’Alessandro et al found that 37% of patients who underwent thermal capsulorrhaphy for anterior, anteroinferior, or multidirectional shoulder instability had unsatisfactory results based on American Shoulder and Elbow Surgeons (ASES) scores, at 2- to 5-year follow-up, lending additional skepticism to the reliability of this surgical technique.56 Miniaci et al presented similar disappointing results in another study of 19 shoulders with MDI treated with thermal capsulorrhaphy, in which 9 patients (47%) had recurrent instability at an average of 9 months postoperatively, 5 patients (26%) had stiffness and 4 patients (21%) had neurologic complications.57 Accordingly, we presently do not advocate thermal capsulorrhaphy for the treatment of RPS because of the variable response patients have demonstrated to thermal energy.
Arthroscopic posterior shoulder stabilization: surgical technique
Setup and examination under anesthesia
Our preference is then to place the patient on a beanbag in the lateral decubitus position, with the affected shoulder oriented superior. An axillary roll is placed. Pillows are placed below and between the legs for prominence padding, and a foam pad is placed over the peroneal nerve of the superior leg at the level of the fibular head. The legs and trunk are secured to the table with straps. Arthroscopic posterior shoulder stabilization also can be performed with the patient in the beach chair position. However, this requires manual adjustments of arm position intraoperatively by an assistant or arm holder and also may provide suboptimal visualization of the posteroinferior labrum and capsule in some cases.
The upper extremity is prepped from the fingers to the level of the sternum anteriorly and the medial border of the scapula posteriorly. Drapes are placed to maintain a wide operative field. The operative shoulder is placed in 10 pounds of longitudinal traction (Arthrex Shoulder Holder, Naples, FL) and positioned in 45 degrees of abduction and 20 degrees of forward flexion. This position displaces the humeral head anteriorly and inferiorly, bringing the posterior labrum into clear, unobstructed view (see Fig. 26-2). A prefabricated bump or additional traction in a tangential vector can be applied to create more distraction between the humeral head and glenoid if desired, thus facilitating visualization and access to the labrum and capsule circumferentially. The acromion, distal clavicle, acromioclavicular joint, and coracoid process are demarcated with a marking pen. Before incision a “surgical pause” is performed with the operative team confirming the patient’s name, medical record number, drug allergies, written informed consent, surgical site, proposed procedure, and availability of required surgical equipment and implants.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree