Arthroscopic Treatment of Lateral Epicondylitis of the Elbow
Champ L. Baker Jr MD
History of the Technique
The initial description of arthroscopic treatment of lateral epicondylitis, or tennis elbow, appeared in 1995 in an article by Grifka, et al.1 Using the endoscopic technique, they described a Hohmann surgical release of the extensor mechanism. In their conclusion, they report, “The Hohmann incision of the tendon plate of the hand extensor muscles can be carried out using an endoscopic procedure without any problem.” Because this article was published as a technical note, no results were given. Lanny Johnson (unpublished data) described an arthroscopic release of the tennis elbow many years ago, but, to my knowledge, never published the findings or results in his patients.
In 2000, Baker et al.2 published the results of a 2-year study of arthroscopic treatment of tennis elbow. With varying modifications of technique, similar results were achieved by Owens et al.3 at Walter Reed and by Cohen and Romeo4 with a four-step technique.
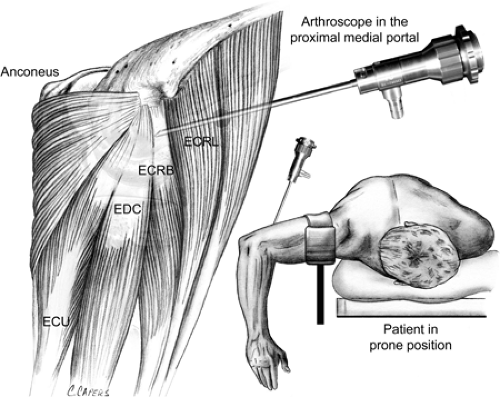
My experience with arthroscopic treatment of lateral epicondylitis began in the early 1990s and included cadaveric studies for safety and efficacy at that time as well as evaluation of clinical results of the first procedures. In 2000 these results were reported along with a description of the technique and classification of the lesions found at surgery.2 The technique involves an arthroscopic evaluation of the glenohumeral joint from proximal to medial portal and use of one or two proximal and midlateral portal sites for debriding the capsule and releasing the extensor carpi radialis brevis (ECRB) tendon.
Indications and Contraindications
Indications for surgical treatment of lateral epicondylitis include dysfunction and persistent pain over the lateral aspect of the elbow for at least 6 months despite treatment. Nonoperative treatment includes activity modification, rest, anti-inflammatory medication, stretching and strengthening exercises, and cortisone injections. Pain usually interferes with the patient’s activities of daily living and sports and is the reason for seeing a physician for treatment.
Contraindications for arthroscopic treatment include localized infection or ankylosis. Less common contraindications are a previous open lateral elbow release or a previous ulnar nerve transfer.
Surgical Techniques
For surgery, the patient can be placed in the supine, prone, or lateral decubitus position. The procedure is most often performed with the patient under general anesthesia but can be done using a regional block, depending upon the positioning of the patient.
Surface Anatomy
Identify and mark the following anatomic landmarks on the arm prior to arthroscopy: the intermuscular septum, the medial and lateral epicondyles, the ulnar nerve, the olecranon tip, the radial head, and the soft spot in the triangle created by the radial head, the epicondyle, and the olecranon. At times it is helpful to mark the area of local tenderness on the patient’s skin prior to administration of the anesthetic to help localize the site to be debrided.
Skin Incision and Deeper Anatomy
After marking the anatomic landmarks, I distend the joint with 20 to 25 cc of saline through the direct lateral portal.
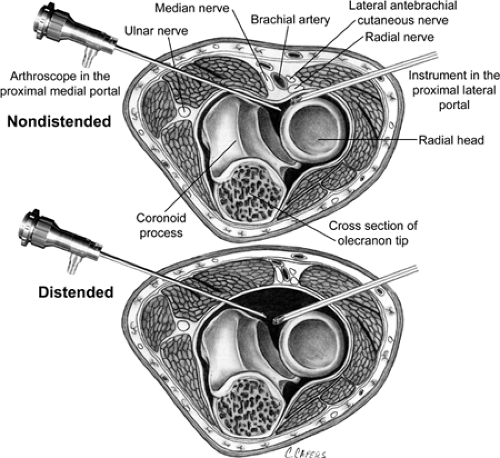
Distention increases the distance between the portal sites and neurovascular structures, making it safer and easier to establish these portals (Fig. 29-1).
Distention increases the distance between the portal sites and neurovascular structures, making it safer and easier to establish these portals (Fig. 29-1).
I establish two portals for the procedure by incising the skin with a scalpel. The proximal medial portal, which is a viewing portal, is located approximately 2 cm above the medial epicondyle and 1 cm anterior to the intermuscular septum (Fig. 29-2). By keeping the trocar and subsequently the arthroscope in contact with the anterior border of the humerus, the surgeon can avoid the risk of injury to the median nerve under the brachialis muscle and enter the joint through the superomedial aspect of the capsule. According
to work reported by Stothers et al.,5 the medial antebrachial nerve is close—an average of 2.3 mm away—and the median nerve is an average of 7.6 mm away from this portal. The brachial artery is, on average, 18 mm from the portal when the elbow is flexed. The ulnar nerve is, on average, 12 mm from the portal.
to work reported by Stothers et al.,5 the medial antebrachial nerve is close—an average of 2.3 mm away—and the median nerve is an average of 7.6 mm away from this portal. The brachial artery is, on average, 18 mm from the portal when the elbow is flexed. The ulnar nerve is, on average, 12 mm from the portal.
The proximal lateral portal is established 1 to 2 cm proximal to the lateral epicondyle directly on the anterior surface of the humerus. The trocar pierces the brachioradialis and distal brachialis before entering the elbow capsule. According to Stothers et al.,5 the posterior branch of the antebrachial cutaneous nerve is, on average, 6 mm away, and the radial nerve is, on average, 4.8 mm away with the elbow in extension, 9.9 mm away with it in flexion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree