Arthroscopic Treatment of Ankle Osteophytes and Osteochondral Lesions of the Talus
James W. Stone
ARTHROSCOPIC TREATMENT OF ANKLE OSTEOPHYTES
Ankle arthroscopy is a highly effective technique for managing an assortment of intraarticular disorders of the ankle, including ankle osteophytes, and talar osteochondral lesions (1, 2 and 3). The joint is constrained, related to the shape of the articular surfaces and ligaments. In general, ankle arthroscopy is more challenging technically compared to larger joints such as the knee. In the past two decades, advances have been made to the extent that ankle arthroscopy is now a standard operative technique. It is now possible to visualize the entire ankle joint with the use of noninvasive distraction. This also lessens the potential for inadvertent damage to the articular cartilage during the operations and avoids problems associated with the more invasive external fixator distraction using pins in the calcaneus and tibia. The surgical instruments have improved markedly, with small diameter and shorter arthroscopes of higher resolution, designed for smaller joints.
Osteophytes occur most commonly at the anterior margin of the tibia and may cause mechanical joint impingement in ankle dorsiflexion with painful limitation of range of motion. The etiology of anterior tibial osteophytes is not definitively known with some investigators postulating a mechanism of direct trauma to the area, for example, during kicking in soccer, and some suggesting a traction mechanism of injury from forced plantarflexion of the ankle joint (4, 5 and 6). The osteophyte appears on plain radiographs as a beak-like prominence on the anterior tibia and may be accompanied by a talar neck lesion, known as a kissing lesion, which may appear to physically impinge on the anterior tibial osteophyte in ankle dorsiflexion. However, some researchers have suggested that the tibial lesions tend to be more medial in location, sometimes extending down the medial malleolus, and the talar lesions tend to be more laterally located. Therefore, the lateral radiograph may suggest mechanical impingement that may not actually be present. Less commonly, osteophytes may form at the medial malleolus or lateral malleolus. Posterior tibial osteophytes are least common and tend to cause greatest symptoms in the plantarflexed ankle.
INDICATIONS AND CONTRAINDICATIONS
The main indication for osteophyte excision is ankle pain attributable to the presence of this lesion, in the absence of other causes of pain such as severe degenerative arthritis, osteochondral lesions of the talus, loose bodies, or soft tissue impingement lesions. Patients may complain of limitation of range of motion of the ankle joint, which is particularly noticeable during stair climbing or squatting, and surgical excision of the osteophyte may allow improved ankle dorsiflexion. However, recovery of motion is not as predictable as diminution of pain after osteophyte excision. A contraindication to performing surgical excision of the osteophyte is significant ankle degenerative arthritis causing diffuse narrowing of the joint or asymmetric bone on bone appearance on plain radiographs. In this case, osteophyte excision will predictably fail because the symptoms are actually due to the arthritic changes rather than the osteophyte.
PREOPERATIVE PLANNING
A comprehensive history and physical examination must be performed for any patient with ankle pain, and the presence of an osteophyte to determine whether the osteophyte itself is responsible for the symptoms or if other abnormalities of the joint must be addressed. Careful evaluation must be performed to differentiate anterior ankle pain arising from a primary ankle joint problem from a subtalar joint condition. A diagnostic injection of local anesthetic into the ankle and subtalar joints at separate times may assist in differentiating pain due to one or both of these joints. Patients with a symptomatic osteophyte complain of pain localized over the osteophyte that usually worsens during activities such as stair or hill climbing, squatting, or running. Occasionally, patients complain of instability or giving way of the joint but do not have objective evidence of ligament laxity. Physical examination must include evaluation of range of motion, alignment, stability, localized swelling, and tenderness over the area of the osteophyte. Passive forced dorsiflexion usually causes increased discomfort in patients with symptomatic anterior tibial osteophytes. Patients may have limited ankle dorsiflexion compared with the normal contralateral ankle. There should be no clinical evidence of joint laxity.
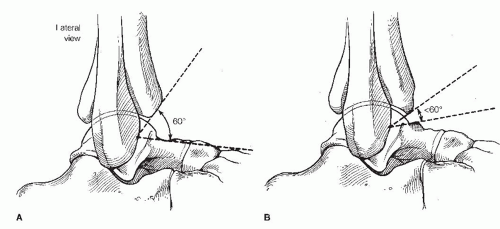
Radiographic evaluation should include routine anteroposterior, lateral, and mortise views (Fig. 33.1). Van Dijk et al. (7) observed that most anterior tibial osteophytes occur asymmetrically on the anterior aspect of the tibia, more on the medial compared with the lateral side. They found that routine lateral radiographs tend to underestimate the size of the osteophyte and suggested a modified radiographic technique to better visualize these lesions (Fig. 33.2). Lateral dorsiflexion stress radiographs may demonstrate impingement of the anterior tibial and talar neck osteophytes.
Scranton and McDermott (8) developed a classification of anterior tibiotalar spurs based on the size of the tibial spur, the presence or absence of a talar spur, and the presence of generalized
degenerative changes within the ankle joint. In type 1, there is synovial impingement, the tibial spur measures less than 3 mm, and there is no talar spur. In type 2, there are osteochondral reaction exostoses, a tibial spur larger than 3 mm, and no associated talar spur. In type 3, there is significant exostosis with tibial and talar spurs. In type 4, there is pantalocrural impingement, and degenerative changes in the ankle joint are present.
degenerative changes within the ankle joint. In type 1, there is synovial impingement, the tibial spur measures less than 3 mm, and there is no talar spur. In type 2, there are osteochondral reaction exostoses, a tibial spur larger than 3 mm, and no associated talar spur. In type 3, there is significant exostosis with tibial and talar spurs. In type 4, there is pantalocrural impingement, and degenerative changes in the ankle joint are present.
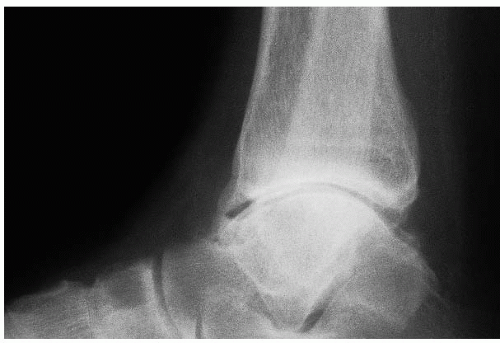 FIGURE 33.1 Lateral radiograph shows a large, anterior tibial osteophyte with a smaller, adjacent talar neck osteophyte (i.e., kissing lesion). |
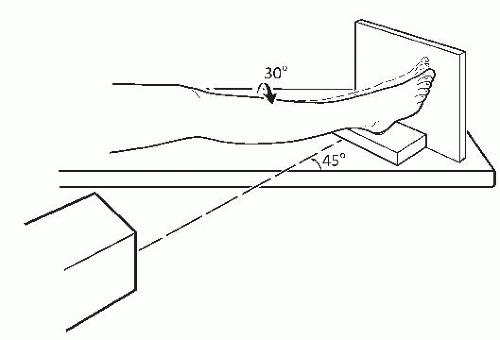 FIGURE 33.2 Technique for lateral oblique radiograph to visualize medial-sided anterior osteophytes. |
The lateral radiograph may be used as a guide to the amount of osteophyte that should be resected surgically. The lateral radiograph is taken with the ankle in neutral position and the angle between the anterior edge of the tibia and the talar neck is determined. This angle should be at least 60° in the normal ankle (Fig. 33.3). The angle decreases to less than 60° with anterior tibial and talar neck osteophytes. Any bony osteophyte projecting anterior to the 60° angle on the lateral radiograph should be resected surgically. Although this method provides a guideline for appropriate resection, arthroscopic visualization of the amount of resection is a better guide.
A computed tomography (CT) scan is usually unnecessary to evaluate these lesions but can be useful for precise localization of a spur if required preoperatively or if there is a concern about other pathology. If used, the CT scan should include thin-section axial images with sagittal and coronal
reconstructions. A bone scan may be helpful in excluding other potential causes of ankle pain, such as an osteochondral lesion of the talus or tibial, and usually shows increased uptake over the area of a symptomatic osteophyte. However, the bone scan has largely been replaced by magnetic resonance imaging (MRI) because it is able to visualize abnormalities both of the bone and soft tissue, which may be contributing to a patient’s pain.
reconstructions. A bone scan may be helpful in excluding other potential causes of ankle pain, such as an osteochondral lesion of the talus or tibial, and usually shows increased uptake over the area of a symptomatic osteophyte. However, the bone scan has largely been replaced by magnetic resonance imaging (MRI) because it is able to visualize abnormalities both of the bone and soft tissue, which may be contributing to a patient’s pain.
Although anterior tibial osteophytes may be removed using open techniques, arthroscopic surgery has largely supplanted open surgery because it may be performed on an outpatient basis with minimal morbidity while affording a more complete view of the joint than with open surgery.
SURGICAL TECHNIQUES
Technique 1: Anterior Approach to Arthroscopic Treatment of Ankle Osteophytes
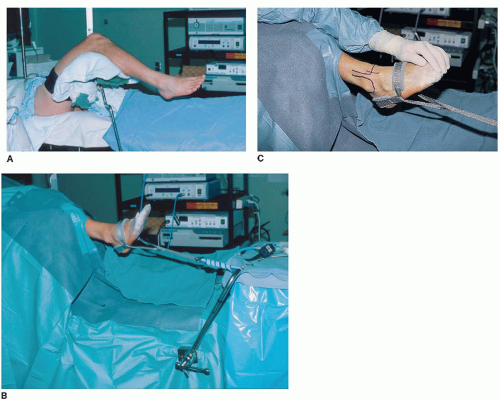
The procedure is performed under general or spinal anesthesia. The patient is positioned supine on the operating table, with the ipsilateral hip and knee flexed and supported by a well-padded leg holder beneath the knee. The leg holder should have a long thigh support with a short leg extension so that when distraction force is applied to the joint it is dissipated over a wide area of the thigh rather than a small area in the popliteal fossa, which could contribute to venous stasis and increase the risk of deep vein thrombosis. This position allows the leg to hang free with the foot and ankle in a plantigrade position, allowing access to the anterior and posterior ankle for portal placement (Fig. 33.4).
After skin preparation, sterile drapes are applied. A noninvasive ankle distractor strap is applied to the foot and connected to a sterile bar attached to the operating table using a Velcro strap. Appropriate tension is “dialed in” with the Velcro strap that is then fixed to itself. The distraction technique allows better visualization of the ankle joint than that obtained without distraction, and the ankle may be manipulated into any position of dorsiflexion or plantarflexion intraoperatively. Invasive joint distraction using pins placed into the tibia and the talus or calcaneus was used in the past. However, it does not achieve a greater degree of distraction than that obtained with noninvasive devices, is associated with significant potential morbidity, and is no longer recommended.
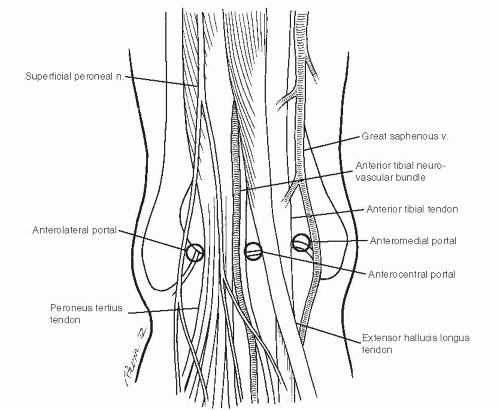
Anatomic landmarks are marked using a sterile marking pen. The medial malleolus, anterior tibial margin, fibula, tibialis anterior tendon, peroneus brevis tendon, and Achilles tendon are outlined. The course of the superficial peroneal nerve can frequently be identified in its subcutaneous position with plantarflexion and inversion of the ankle. Its position should be marked with a sterile marking pen to avoid injury to this sensory nerve.
The anteromedial portal is created first (Fig. 33.5). It is located adjacent to the medial margin of the tibialis anterior tendon. An appropriate position for the portal is ensured by using an 18-gauge needle for localization. The best position allows easy needle passage across the joint without impingement on the tibia or talus. A position too proximal results in instrument impingement on the talus, and a position too distal causes instrument impingement on the tibia. All portals are created in such a manner as to minimize risk of injury to superficial nerves.
The skin alone is incised without advancing the scalpel blade into the subcutaneous tissues. The subcutaneous tissues are then bluntly dissected with a small hemostat down to the level of the joint capsule. A cannula with a blunt obturator is then used to penetrate the capsule. The ankle joint capsule is quite thin so a sharp obturator is not required. This technique minimizes the risk of iatrogenic articular cartilage injury during creation of portal.
The 2.7-mm-diameter arthroscope is better suited for ankle arthroscopy than the 4-mm-diameter arthroscopes used for large joint arthroscopy. It is useful to have both 30° and 70° viewing angle arthroscopes available for all ankle cases. It is also useful to have a 1.9-mm-diameter arthroscope available for cases in which the joint is very tight and difficult to instrument even with a joint distractor applied.
The arthroscope is introduced into the anteromedial portal, and the anterolateral portal is created under direct visualization, again using and 18-gauge needle first to optimize portal location. The anterolateral portal is placed adjacent to the lateral border of the peroneus tertius tendon. Careful attention to portal creation technique can avoid injury to branches of the superficial peroneal nerve.
The posterolateral portal is then placed under direct visualization (Fig. 33.6). An 18-gauge needle is placed at the lateral margin of the Achilles tendon approximately 1 to 2 cm distal to the level of the anterior portals. This more distal position accommodates the convexity of the talar articular surface. While viewing arthroscopically, the needle is observed to enter the joint just beneath the posterior syndesmotic ligament. The cannula is used for dedicated inflow.
Some surgeons recommend use of the anterior portals without the posterolateral portal. However, more efficient inflow can be obtained using a dedicated posterior portal. All surgeons performing arthroscopic ankle surgery should be comfortable using a posterolateral portal, because this is advantageous in approaching other posterior ankle pathology, including osteochondral talar dome lesions, posterior osteophytes, or posterior loose bodies.
A comprehensive joint examination is then performed first from the anteromedial approach, then from the anterolateral approach to rule out other intraarticular pathology. Initial visualization may be difficult secondary to the presence of anterior joint synovitis. The inflamed synovium is removed using a 2.9- or 3.5-mm shaver. Care must be exercised to avoid directing the shaver anteriorly, inadvertently penetrating the anterior capsule and causing injury to the anterior neurovascular structures. Anterior joint visualization may be improved by decreasing the distraction force and dorsiflexing the ankle, a maneuver that causes the anterior capsule to relax and expand with irrigant fluid.
The extent of the osteophyte is then determined (Fig. 33.7A). The anterior capsule is invariably adherent to the superior surface of the osteophyte and must be dissected free. This maneuver is most easily performed using the shaver with the blade directed against the osteophyte, lifting the adherent capsule off the osteophyte proximally. Alternatively, a radiofrequency wand may be used to strip the capsule from the anterior surface of the osteophyte. This instrument has the benefit of providing precise dissection while simultaneously achieving hemostasis.
The osteophyte may be resected using an osteotome or rongeur. An easier technique is to use a 4-mm round burr introduced from the anterolateral portal to remove the lateral portion of the osteophyte while viewing with the arthroscope in the anteromedial portal (Fig. 33.7B).
The portals are then switched to remove the medial half of the osteophyte. The preoperative radiographs should be studied to determine the extent of the proposed excision. With experience, the surgeon is able to identify where abnormal bone constituting the osteophyte ends and the normal contour of the tibial begins (Fig. 33.7C). In a patient with minimal arthritis, visualization of normal articular cartilage thickness along the entire anterior margin of the tibia signals sufficient bone removal. An intraoperative lateral radiograph may assist the surgeon to determine that an adequate amount of osteophyte has been removed.
Care should be taken to examine the medial extent of any anterior tibial osteophyte. Osteophytes often extend onto the anterior surface of the medial malleolus and may cause symptomatic bony impingement with ankle dorsiflexion.
After excision of the anterior osteophyte, the arthroscope is inserted into the anterolateral portal, and the anterior aspect of the medial malleolus is visualized. Resection of bone to the normal contour of the medial malleolus must be performed.
Occasionally, an osteophyte of the tip of the medial malleolus may be observed (Fig. 33.8). Such a spur can be removed by viewing with the arthroscope in the anteromedial portal and the instruments placed into an accessory anteromedial portal. The location for the accessory portal is determined by placing an 18-gauge needle approximately 1 to 2 cm medial and
slightly distal to the standard portal and directing the needle into the medial gutter. Wound healing problems can be avoided by ensuring that the accessory portal is located at least 1 cm from the standard portal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree