Arthroscopic Subscapularis Tendon Repair
Ian K.Y. Lo
Matthew Denkers
Due to their unique anatomy and pathoanatomy, subscapularis tears are commonly missed, particularly partial tears and full-thickness tears of upper subscapularis tendon. Although their incidence has been reported as high as 27%, many subscapularis tears occur in combination with other disorders particularly supraspinatus tendon tears. Importantly, the subscapularis tendon functions as a dynamic stabilizer, providing the anterior moment of the transverse force plane couple. Therefore, repair of subscapularis tendon tears is critical in balancing the force couples to provide a stable fulcrum for glenohumeral motion (1).
CLINICAL EVALUATION
Pertinent History
Patients with subscapularis tears usually present with pain as their predominant complaint. Although the reported mechanisms of injury are a forced external rotation or hyperextension load, many patients may not recall a traumatic episode, particularly in degenerative or combined tears of the subscapularis.
Physical Examination
Physical findings associated with subscapularis tendon tears are a painful arc of motion, a decrease in internal rotation strength, and an increase in passive external rotation. However, various special tests have been described to evaluate the integrity of the subscapularis tendon.
The lift-off test evaluates the patient’s ability to lift the back of the hand posteriorly off the lumbar region using terminal internal rotation (i.e., subscapularis function). However, this classic test can be normal in patients with upper subscapularis tendon tears and may not be positive until greater than 50% to 75% of the subscapularis tendon is torn. Furthermore, some patients cannot bring the affected arm into the starting position because of pain or restricted range of motion. In this scenario, the belly-press test or Napoleon test may be used.
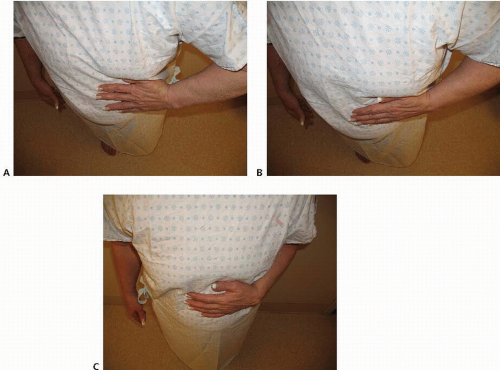
When performing the belly-press test (2,3), the patient presses on the abdomen with the palm of the hand and brings the elbow anterior to the mid-coronal plane of the body using internal rotation. The result of the test is considered positive (i.e., a subscapularis tear) when the patient’s elbow drops posteriorly behind the mid-coronal plane and pressure on the abdomen is provided instead by extension of the shoulder. The Napoleon test (4) is similarly performed, but also considers the position of the wrist. In patients with a subscapularis tear, when the elbow drops posteriorly the wrist also correspondingly flexes against the abdomen (the position in which Napoleon commonly held his hand against his stomach during portraits). The amount of subscapularis tearing has been correlated with the degree of wrist flexion. Tears of less than 50% of the subscapularis tendon can have negative Napoleon signs (i.e., wrist fully extended), tears involving greater than 50% but not the entire tendon have an intermediate result (i.e., wrist flexed 30° to 60°), and tears involving the entire subscapularis tendon have a positive Napoleon test (i.e., wrist flexed 90°) (4) (Fig. 13.1).
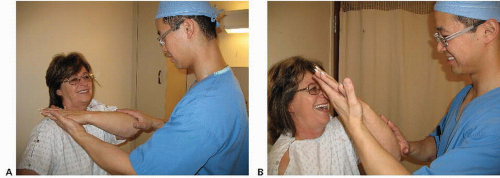
The bear-hug test has been recently described and may be more sensitive than the previous tests for small upper subscapularis tendon tears (5). In the bear-hug test, the patient first positions the hand of the affected side on the contralateral shoulder with the elbow in a forward flexed position (5) (Fig. 13.2A). As the examiner pulls the patient’s hand off the shoulder using an external rotational load, the patient resists using internal rotation. The result of the test is considered positive if the examiner is able to lift the patient’s hand off the shoulder and is suggestive of at least a partially torn subscapularis (Fig. 13.2B).
In addition to subscapularis tendon insufficiency, patients should also be evaluated for subcoracoid impingement. Although controversial, subcoracoid impingement has been associated with subscapularis tears and may be an etiologic factor and a cause of persistent shoulder pain (6). Presumably, the origin of this pain is secondary to impingement between the subscapularis tendon/lesser
tuberosity against the coracoid process. Most patients clinically will demonstrate pain and tenderness about the coracoid and subcoracoid region with a positive coracoid impingement test. This test result is considered positive when pain and/or clicking are elicited by passive forward flexion, adduction, and internal rotation (7,8).
tuberosity against the coracoid process. Most patients clinically will demonstrate pain and tenderness about the coracoid and subcoracoid region with a positive coracoid impingement test. This test result is considered positive when pain and/or clicking are elicited by passive forward flexion, adduction, and internal rotation (7,8).
Diagnostic Imaging
A few studies have specifically evaluated the use of diagnostic imaging in the evaluation of the subscapularis tendon. Plain radiographs are usually nonspecific, but may demonstrate static anterior subluxation of the humeral head on axillary radiographs in patients with chronic subscapularis tendon insufficiency. In addition, proximal humeral head migration on anterior-posterior radiographs is highly suggestive of a massive, rotator cuff tear that may include the subscapularis tendon.
Ultrasound can provide an inexpensive, noninvasive, dynamic assessment of the rotator cuff, but is highly observer dependent. Ultrasound has been reported to be approximately 85% accurate in detecting full-thickness subscapularis tears, but is not as accurate in demonstrating partial thickness tears, particularly small upper subscapularis tendon tears.
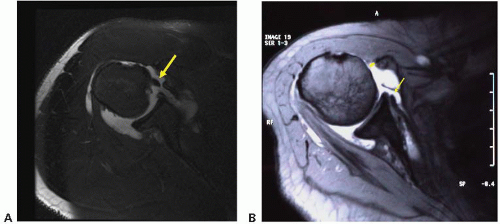
MRI is considered the modality of choice for evaluating rotator cuff pathology. The addition of contrast enables better delineation of rotator cuff pathology and may improve diagnostic accuracy, particularly of upper subscapularis tears. Subscapularis tears can be demonstrated as areas of disorganization or disruption of normal tendon morphology and high signal intensity on T2-weighted images. In addition, adjacent pathology may be suggestive of subscapularis tearing. Medial dislocation of the long head of the biceps tendon is highly suggestive of a subscapularis tear since subscapularis tears commonly disrupt the medial sling of the biceps tendon resulting in biceps instability (Fig. 13.3A).
Although MRI arthrography has been reported to be 91% sensitive and 86% specific for detecting subscapularis tears (9), others have reported less promising results. Fullthickness, upper subscapularis tears and partial thickness tears are commonly missed on MRI. In one study, surgically confirmed subscapularis tears were identified in only 31% (5/16) of patients on MRI (10).
MRI may also be used to estimate the chronicity of the tear. Patients with severe atrophy and fatty degeneration on MRI or CT generally have poor tendon quality and limited tendon excursion, potentially indicating an irreparable subscapularis tear (11,12). However, other authors have argued that despite atrophy and fatty degeneration, many subscapularis tears are commonly reparable and may postoperatively function as a tenodesis to provide a stable fulcrum of motion (13).
In addition to subscapularis pathology, imaging studies should be evaluated for evidence of subcoracoid impingement. The subcoracoid space (i.e., between the lesser tuberosity and the coracoid) can be reduced by a number of potential causes including lesser tuberosity fracture, calcific tendinosis, postoperative changes (e.g., glenoid version alterations and coracoid osteotomy), or prominence of the coracoid. Importantly, it should be remembered when interpreting imaging that proximal humeral migration and anterior subluxation of the glenohumeral joint can exacerbate narrowing of the subcoracoid space, particularly when imaging studies are obtained supine (e.g., MRI).
One measurement technique, the coracoid index, measures the length of the coracoid tip, which projects lateral to a line drawn tangential to the glenoid face on axial CT scans. The normal projection of the coracoid lateral to this line was 8.2 mm (range: −2.5 to 25 mm) in 67 patients (14). Although not clearly defined, abnormal or excessive projection or angulation of the coracoid beyond this tangential line may predispose to subcoracoid impingement.
The more accepted method of measurement is to use the coracohumeral distance (i.e., the distance between the coracoid tip and the humerus/lesser tuberosity) as measured on axial CT or MRI images. In normal shoulders, the coracohumeral distance is 8.7 to 11.0 mm (7,8). In contrast, a narrowed coracohumeral distance is commonly associated with subscapularis tears (Fig. 13.3B). In one study of
patients requiring a subscapularis repair, the coracohumeral distance was 5.0 ± 1.7 mm, compared with 10.0 ± 1.3 mm in a control group that had no rotator cuff, subscapularis, or subcoracoid pathology (15). Therefore, many authors consider a coracohumeral distance of less than 6 mm as evidence of narrowing although its exact role in the pathogenesis of subscapularis tendon tearing remains unclear.
patients requiring a subscapularis repair, the coracohumeral distance was 5.0 ± 1.7 mm, compared with 10.0 ± 1.3 mm in a control group that had no rotator cuff, subscapularis, or subcoracoid pathology (15). Therefore, many authors consider a coracohumeral distance of less than 6 mm as evidence of narrowing although its exact role in the pathogenesis of subscapularis tendon tearing remains unclear.
TREATMENT
Nonoperative
Nonoperative treatment of subscapularis tears is similar to nonoperative treatment for standard posterosuperior rotator cuff tears. A few protocols have been specifically designed to address the subscapularis tendon. However, general conservative management may include cold/heat therapy, pain medications, nonsteroidal anti-inflammatories, injections (e.g., subacromial or glenohumeral), or physical therapy.
Operative Indications and Timing
The indications for arthroscopic subscapularis repair are essentially the same as indications for arthroscopic rotator cuff repair. Patients with significant pain and disability despite conservative management for 3 to 6 months are candidates for arthroscopic repair. Similar to acute tears of the posterosuperior rotator cuff, acute subscapularis tears should be treated urgently to prevent further retraction and atrophy. In patients with chronic tears, particularly those with significant tendon retraction and fatty infiltration of the subscapularis tendon, arthroscopic repair may still be attempted but may be unsuccessful. Alternative treatments including allograft or tendon transfer (e.g., split pectoralis major transfer) may be considered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree