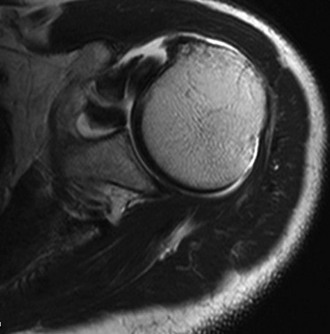
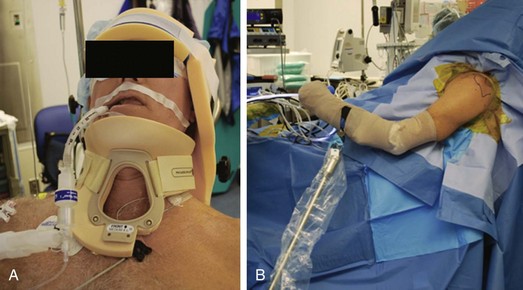
Chapter 22 As arthroscopic techniques in shoulder surgery have improved, recognition of subscapularis tendon injuries has increased. Although isolated subscapularis tears continue to be rare, estimated at 5% of rotator cuff tears,1 they are increasingly being seen in association with other supraspinatus, infraspinatus, and teres minor tears, with an incidence estimated at 27% to 43%.2 Because of this, there has been increased interest in arthroscopic subscapularis tendon repairs. The main advantages of an arthroscopic repair of the subscapularis tendon are smaller incisions, less postoperative pain, and the ability to better visualize and address coexisting pathologic processes, including labral tears, long head biceps injury, and superior and posterior rotator cuff tears. This chapter addresses the preoperative considerations and the techniques involved in performing an arthroscopic subscapularis repair. Often there is a history of trauma, which may include an abduction and external rotation moment, direct blow, heavy lifting, or traction injury.3 For degenerative tears, the patient may report a gradual worsening of anterior shoulder pain without specific trauma. Patients may note difficulty with internal rotation—for example, in tucking in a shirttail. Consider a full differential diagnosis for anterior shoulder pain, including acromioclavicular joint arthrosis or dislocation, biceps tendon tears or inflammation, anterior capsulolabral damage, and fractures of the lesser tuberosity. It is important to isolate the subscapularis muscle from other internal rotators during examination. Owing to the high association with biceps tendon pathology, careful examination with the Speed and O’Brien tests is also important. The belly press test is performed by asking the patient to press the ipsilateral hand on the abdomen, maintaining the elbow anterior to the body. The belly press test result is considered positive if the patient is not able to keep the elbow anterior to the trunk or if the wrist is flexed in attempting to press into the abdomen. The lift-off test requires the patient to be able to place the ipsilateral hand behind the back. The patient is asked to lift the hand off the back; if the patient is unable to do so, the test result is considered positive. The most sensitive test is the bear hug test.4 The patient places his or her ipsilateral hand on the contralateral shoulder with the elbow elevated forward. The test result is positive if the surgeon is able to lift the patient’s hand off the shoulder. A standard shoulder imaging series including an axillary view is obtained to assess for alternative pathologic changes, such as fractures and glenohumeral arthritis. Magnetic resonance imaging is the gold standard imaging modality for diagnosis of subscapularis tendon tears and evaluation of muscle belly quality, fatty infiltration, and displacement of the long head of the biceps tendon (Fig. 22-1). Magnetic resonance arthrography improves the sensitivity of diagnosis of partial tears and labral and biceps pathology. In addition, the coracohumeral distance is measured from the tip of the coracoid to the humerus on an axial cut with the smallest distance.2 A distance of 6.5 mm is considered narrowed. The tendon should be assessed on both axial and sagittal images, with verification of its insertion on the lesser tuberosity. We prefer the beach chair position for arthroscopic repairs of the subscapularis (Fig. 22-2). The upper extremity can be easily moved and rotated to better visualize the subscapularis and its insertion. Furthermore, the beach chair position allows the surgeon to convert easily to an open procedure if necessary.
Arthroscopic Subscapularis Repair
Preoperative Considerations
Physical Examination
Imaging
Surgical Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine