Arthroscopic Setup, Instrumentation, Portals, and Operative Pearls
Kevin W. Farmer
Gautam P. Yagnik
John W. Uribe
Knee arthroscopy is the most commonly performed orthopedic procedure (1). As surgeons add this procedure to their repertoire, it is important to develop a consistent approach to the operation. Through consistency, complications are minimized, operative time is decreased, and the potential of missed pathology is diminished. This chapter will describe the authors’ approach to a basic knee arthroscopy. It is important to realize that there are several ways to approach this procedure, and surgeons should utilize their training and experience to ensure an efficient performance in the operating room.
PREOPERATIVE MARKING
Wrong-site surgery is a concern for all orthopedic surgeons. The operating surgeon should mark the operative site before the administration of any anxiolytic or narcotic medications (Fig. 53.1). An evaluation of malpractice claims found knee arthroscopy to be the most common procedure involved in a wrong-site surgery (2). Orthopedic surgeons have an estimated 25% chance of wrong-site surgery during their career (3). In 1998, the American Academy of Orthopaedic Surgeons began the “sign your site” campaign, recommending the operating surgeons initials are placed in indelible ink on the operative site such that the marking is unambiguous and will be present on the operative site after prepping and draping (see Fig. 53.1) (4). The Joint Commission on Accreditation of Healthcare Organizations further expanded the recommendations to include a time-out to verify the initials in the field, the correct patient and site, the correct procedure, correct position, and the availability of appropriate equipment (5). Recent studies have demonstrated that chloraprep was 22 times more likely to remove site markings before prepping (6), and that ink in the sterile field does not increase infection risk (7).
ANTIBIOTICS
There are no randomized controlled trials looking at the role of prophylactic antibiotics in arthroscopic surgery. The incidence of infections with arthroscopy is extremely low, thus it would take a very large study to ensure an appropriate power (8). Nonetheless, we routinely give 2 g of cefazolin, or 600 to 900 mg of clindamycin for true penicillin allergies, within 1 hour of tourniquet use or incision.
ANESTHESIA
Local anesthetic with a mixture of lidocaine and bupivacaine both intra-articularly and at the portal sites have been used successfully in basic knee arthroscopies (9). Any bony work would have to be minimized, as this would likely elicit a pain response. Use of a tourniquet would also have to be minimized in an awake patient in this setting. It is important to confirm the maximum dose that can be safely used during the case to avoid serious complications. Given the recent findings of chondrolysis with the use of bupivacaine, this option may become less favorable with many orthopedic surgeons (10).
Regional anesthesia with sedation or spinal anesthesia are appropriate options for knee arthroscopic procedures, especially in the setting of medical comorbidities that limit general anesthesia. There is some evidence that regional anesthesia may decrease hospital admissions in an outpatient setting. A regional anesthetic is preferred to spinal due to decreased rates of urinary retention (11). Complications including femoral neuritis and hematomas have been reported. All patients with a femoral nerve block should be placed in a knee immobilizer until quadriceps function returns to minimize fall risks (12).
General anesthetic is the most commonly used modality for knee arthroscopy. It minimizes the time constraints placed by some local and regional anesthetics and allows for complete muscle relaxation if necessary. A combination of general and regional anesthetic provides effective intraoperative relaxation and postoperative pain control.
Our preferred anesthesia protocol is usually general anesthesia for simple arthroscopies. If we are expecting a more involved procedure, we will often use a regional anesthetic, if preferred by the anesthesiologist and the
patient, in combination with a general anesthetic. We are less likely to use a regional anesthetic in cases that have an increased risk of nerve injury, as we like to perform an adequate neurovascular examination at the end of the case.
patient, in combination with a general anesthetic. We are less likely to use a regional anesthetic in cases that have an increased risk of nerve injury, as we like to perform an adequate neurovascular examination at the end of the case.
EXAMINATION UNDER ANESTHESIA
Once the patient has appropriate muscular relaxation, an examination under anesthesia should be performed in all cases. The examination should include evaluation of effusion, range of motion, crepitance, patellar mobility, and stability. Specialized tests such as the Lachman, pivot shift, and dial test should be performed in appropriate cases (Fig. 53.2). One should always compare findings with the contralateral side.
SETUP
A well-padded tourniquet should be placed high on the thigh in all cases, even if its use is not expected (Fig. 53.3). It is important to ensure proper table positioning before draping. If fluoroscopy is needed, the table should be adjusted so all obstructing objects are out of the way. The patient should also be moved on the bed to the appropriate position based on surgeon’s preference. This position is often distal, allowing the foot of the bed to be lowered if needed.
 FIGURE 53.2. An examination under anesthesia should always be performed and compared with the contralateral side. |
PATIENT POSITIONING—LEG HOLDER
The use of a leg holder is the author’s preferred method for knee arthroscopy. We favor this position as it maximizes the freedom of movement of the knee and can be utilized without the need for an assistant. The leg holder is placed on the operating table at the distal break in the table. This allows the foot of the bed to be lowered during the case (Fig. 53.4). The patient should be positioned so the leg holder is four finger breadths above the superior pole of the patella (Fig. 53.5). This position provides enough room to allow varus/valgus stress without compromising portal placement, but may need to be altered based on the case (i.e., if more exposure is needed proximally for a posterolateral corner reconstruction). A pad is placed under the contralateral leg, and we let this hang off the end of the table (Fig. 53.6). A lithotomy leg positioner may also be used. Since the leg holder has a venous tourniquet effect if sufficiently tightened, we inflate the tourniquet before placing in the leg holder (see Fig. 53.3). The foam leg
holder is then placed and tightened with the leg in internal rotation to prevent locking the leg in a naturally externally rotated position (Fig. 53.7). Examination of the medial compartment is accomplished with a valgus stress placed with the leg on the surgeon’s outside hip (Fig. 53.8). Examination of the lateral compartment is accomplished by placing a varus stress on the knee with the leg on the surgeon’s inside hip (Fig. 53.9).
holder is then placed and tightened with the leg in internal rotation to prevent locking the leg in a naturally externally rotated position (Fig. 53.7). Examination of the medial compartment is accomplished with a valgus stress placed with the leg on the surgeon’s outside hip (Fig. 53.8). Examination of the lateral compartment is accomplished by placing a varus stress on the knee with the leg on the surgeon’s inside hip (Fig. 53.9).
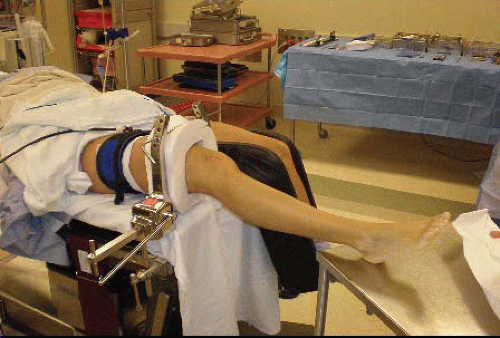 FIGURE 53.4. The operative leg holder should be placed at the distal break in the bed, so the foot of the table can be lowered. |
 FIGURE 53.5. The leg holder should be placed approximately four finger breadths above the superior pole of the patella. |
 FIGURE 53.6. The contralateral leg should be well padded during the operation. Compression stockings and pneumatic compression devices are useful in longer cases.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|







