Fig. 11.1
Anatomical cut on fresh corpse, lateral section through the wrist at the metacarpal II. The remaining portion of the scaphoid is removed and radiocarpal and intercarpal palmar and dorsal ligaments loose, the scapholunate ligament is cut at its anchorage to the scaphoid, its palmar and dorsal ends are connected to the capsular ligament devices palmar and dorsal
The importance and contribution of these ligaments in maintaining scapholunate stability are still not fully understood. Just like other ligaments in the body, the interosseous ligament bone scapholunate can be stretched to a yield point. Mayfield [1] showed that an elongation of approximately 225 % is required before failure of the SL ligament occurs, while the SL ligament can elongate to twice its length before it ruptures. Despite this, it seems that the trauma must involve the scapholunate complex itself to result in a rupture. Isolated lesions of the scapholunate ligament may not cause scapholunate dissociation on radiographs. Conversely, a simple weakening of the scapholunate ligament not visible on radiographs may cause mechanical problems and painful phenomena. For scapholunate diastasis to be complete and visible on radiographs, the intrinsic and extrinsic systems must both be involved. More frequently, radiological abnormalities are not seen initially after a lesion of the scapholunate ligament but only appear over time due to the progressive destruction of the extrinsic ligamentous system. This explains the frequent delay in diagnosis of this pathology.
Factors Affecting the Stability of the Distal Pole of the Scaphoid
Structures stabilizing the distal pole of the scaphoid play a significant role because of the forces transmitted by the first metacarpal ray during abduction and opposition. The flexor carpi radialis (FCR) plays both an active and a passive role: the fibrosseous subsheath of the FCR is superimposed on the distal scaphoid, reinforcing the scapho-trapezio-trapezoid ligament and scapho-capitate ligament.
The Scapholunate Interosseous Ligament
The scapholunate interosseous ligament functions as a torsion bar by acting as a viscoelastic dampener and it interconnects the scaphoid and the lunate. It is a nonhomogeneous structure having three distinct parts: the anterior (volar) ligament is confluent with the long and short radio-lunate ligaments. The intermediate membranous fibrocartilaginous and non-vascularized part corresponds to the area that can be depressed on arthroscopic palpation. The posterior (dorsal) part is the strongest and most resistant part, and it is securely attached to the dorsal capsule which inserts onto the dorsal scapholunate ligament and is continuous with the dorsal scapho-triquetral ligament and dorsal intercarpal ligament.
Anatomical Review
From a strictly anatomical point of view, the scapholunate articulation is characterized by the juxtaposition of two flat facet joints, producing a syndesmosis between the scaphoid and the lunate.
Although the scapholunate interosseous ligament has been divided into three distinct anatomical parts, it would not be realistic to assign a role to any one particular part of the ligament. The nomenclature of “interosseous” ligament should be limited to the intermediate fibrocartilaginous non-vascularized therefore unrepairable part. The anterior (volar) and posterior (dorsal) parts of the scapholunate ligament, however, are perfectly integrated into the palmar and dorsal extra synovial ligaments, respectively. These parts of the SL complex are well vascularized and have a cellular structure that has the potential to heal after surgical repair.
The proximal carpal row is a complex system that must have some degree of torsional elasticity allowing flexion-extension of the scaphoid, and at the same time have stability that can withstand compressive stresses transmitted through the distal carpal row, without deforming much. This system is much more flexible on the palmar aspect permitting limited movements between the carpal bones in the sagittal plane and allows controlled chain torsion between the scaphoid, the lunate, and the triquetrum. Therefore, procedures aimed at reconstruction of the dorsal capsular ligament by a dorsal capsulodesis to restore SL stability invariably lead to stiffness of the wrist joint.
Diagnosis of SL Instability
Patients with a lesion of the scapholunate ligament often have a history of a hyperextension injury to the wrist joint due to a fall on an outstretched hand. Wrist extension and supination is the main mechanism of injury. In acute injury, clinical examination reveals localized edema and pain localized to the dorsal scapholunate interval. Scapholunate instability can be evaluated by Watson’s “scaphoid shift test.” This test analyzes scaphoid mobility with the wrist in radial deviation and palmar flexion, while pressure is applied on the scaphoid tuberosity in a palmar to dorsal direction.
Patients with a partial lesion of the scapholunate ligament experience pain localized on the dorsal aspect of the wrist over the scapholunate interval; but there is no “click” on performing the Watson’s test. Pain experienced on the volar aspect of the scaphoid tubercle during this maneuver is not clinically significant. Patients with a complete lesion of the scapholunate interosseous ligament demonstrate subluxation of the proximal pole of the scaphoid on the posterior margin of the radius even without application of manual pressure on the scaphoid tubercle. One must, however, examine both wrists to verify that there is no constitutional instability in hypermobile patients. It is also possible to perform the Watson’s test under local anesthesia if the patient experiences too much pain.
Plain radiographs are essential in clinically suspected lesions of the scapholunate ligament. These include a standard postero-anterior (PA) radiograph (Fig. 11.2), radial and ulnar deviation PA views, and a strict lateral view (Fig. 11.3) and a clenched fist PA view. Gilula’s lines and the scapholunate interval are assessed on the PA views whereas the scapholunate angle is measured on the lateral view. A scapholunate gap of more than 4 mm is indicative of a scapholunate ligament injury. Dynamic views are also essential to diagnose a dynamic instability that would otherwise be missed on plain radiographs. The scapholunate angle, i.e., the angle between the axis of the scaphoid and a line joining the two horns of the lunate, is measured. Normal values are between 30° and 60° with an average of 47°. An angle greater than 60°, which is the result of palmar flexion of the scaphoid, should be considered pathognomonic of scapholunate instability. The TERRY-THOMAS sign is considered positive when the space between the scaphoid and the lunate appears abnormally large compared to the opposite side. Scapholunate interval greater than 5 mm even though asymptomatic is the result of a scapholunate dissociation. The scaphoid ring sign is also useful for the diagnosis of scapholunate instability. It is seen on PA radiographs due to an overlap of the distal tubercle and proximal pole of the scaphoid with the scaphoid in palmar flexion following injury to the scapholunate interosseous ligament. On normal lateral radiographs of the wrist, a C-shaped line can be drawn together palmar edges of the scaphoid and radius. In scapholunate dissociation, flexion of the scaphoid causes an abnormal scaphoid V-shaped pattern (V-sign).



Fig. 11.2
X-ray of the wrist against objectifying an important scapholunate space

Fig. 11.3
X-ray of the wrist profile objectifying a dorsal deviation of the lunate (DISI)
Treatment
Acute Lesions
In acute injuries, the first step is assessment and grading of the lesions. The patient is operated under regional anesthesia. With the patient in a supine position and the arm resting on an arm table, the elbow is flexed to 90°. A vertical traction of 5–7 lb is applied. In this way, the wrist can be analyzed at the same time by arthroscopy and fluoroscopy. We can also control the reduction and stabilization of the scapholunate injury. The joint is insufflated with 3–5 cc of normal saline. An abnormal passage of fluid from the radiocarpal joint to the midcarpal is already an indicator to an underlying lesion of the scapholunate ligament. The trocar and the arthroscope are introduced through a standard 3-4 radiocarpal portal. Care should be taken while inserting the trocar in order to avoid damage to the cartilage. The 4-5 or the 6R radiocarpal portal is used for passing a hook probe or instruments. It is possible to switch the position of the arthroscope and instruments at any time. The wrist is systematically examined starting from the radial side to the ulnar side. A lesion of the scapholunate ligament may not be properly appreciated until it is palpated/tested with the probe. The arthroscopic examination is then performed in the midcarpal joint. The arthroscope is introduced through radial midcarpal portal. Particular attention is paid to the dorsal edge of the scaphoid, which is in an abnormal anatomical position in case of complete scapholunate dissociation. In small wrists, it may be easier to insert the arthroscope through an ulnar midcarpal portal. A thorough examination of the radiocarpal and the midcarpal joints will reveal any injury to the scapholunate ligament. The ability to insert a probe/scope between the scaphoid and the lunate bones, the existence of a gap between the two bones, and the existence of a step-off between the lunate and the proximal pole of the scaphoid are all indicative of a rotational instability.
The normal ligament has a smooth and slightly concave bulge that is seen perfectly in the radiocarpal space. Often this normal concave aspect becomes convex when the ligament is traumatized and becomes weakened. Normally, there is a close contact between the scaphoid and the lunate without any step-off when seen through the midcarpal portals. With the scapholunate ligament intact, it is impossible to pass a probe from the midcarpal joint to the radiocarpal joint or vice versa. In the midcarpal joint, the position of the dorsal edge of the scaphoid is also examined. With increasing severity of scapholunate ligament injury, this tends to move into palmar rotation. GEISSLER [2] has described an arthroscopic classification of carpal instabilities. In stage I (Fig. 11.4), radiocarpal examination reveals a loss of the normal concave appearance of the scapholunate ligament, which then appears convex. This marks the beginning of weakening of the scapholunate interosseous ligament. A midcarpal examination in stage I reveals a normal and congruent SL aspect without any step-off.
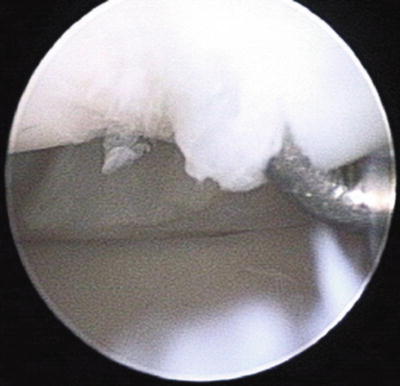
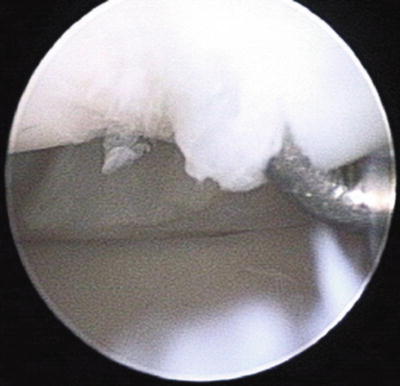
Fig. 11.4
Arthroscopic view of a radiocarpal stage I lesions, simple perforation of the scapholunate ligament
In GEISSLER stage II lesions (Fig. 11.5), radiocarpal arthroscopy reveals an SL ligament that appears convex as in stage I. However, midcarpal joint arthroscopy reveals a loss of congruence the scapholunate space. The scaphoid begins to flex and the dorsal edge is rotated relative to the lunate resulting in a slight step-off between the scaphoid and the lunate bones.
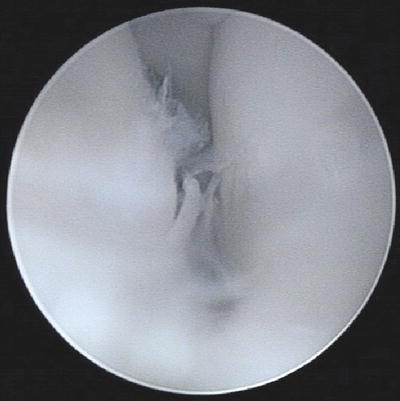
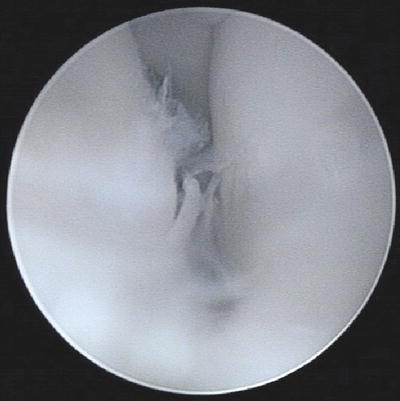
Fig. 11.5
Arthroscopic view of midcarpal injury stage II showing a moderate gap between the scaphoid and lunate
In GEISSLER stage III (Fig. 11.6), radiocarpal arthroscopy reveals damage to the SL ligament that begins in the midportion and extends toward the dorsal part. Often we begin to see an abnormal space between the scaphoid and lunate. A probe can be passed through the scapholunate space and into the midcarpal joint. Often a remnant of the scapholunate ligament remains attached to the lunate. Midcarpal joint examination reveals an abnormal discrepancy between the scaphoid and lunate with a step-off. A 2 mm probe can easily pass through the space between the scaphoid and lunate.


Fig. 11.6
Arthroscopic view of medial carpal injury stage III showing a larger gap allowing a probe between the scaphoid and the lunate the radiocarpal joint to the medial carpal
In GEISSLER stage IV (Figs. 11.7 and 11.8), the ligament is completely torn. A 2.7 mm arthroscope can pass without difficulty from the radiocarpal joint to the midcarpal joint or back through the space between the scaphoid and the lunate (“Drive Through Sign”). There is usually no continuity of the ligament between the scaphoid and the lunate at this stage.
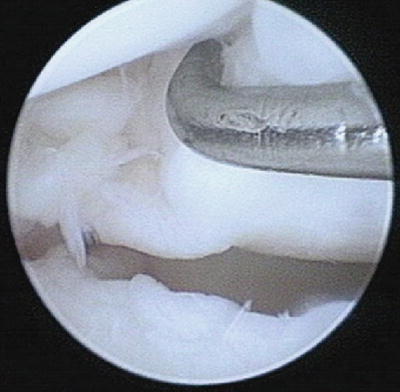

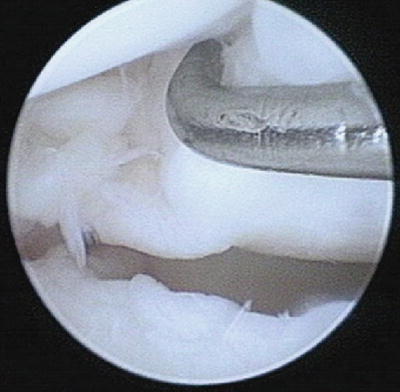
Fig. 11.7
View of a radiocarpal arthroscopic stage IV lesion, showing a complete tear of the scapholunate ligament

Fig. 11.8
Arthroscopic view of midcarpal injury stage IV showing a very large gap between the scaphoid and lunate letting a cutting 3 mm of the radiocarpal joint to the midcarpal
Patients with acute stage II or III lesions are ideal candidates for treatment by arthroscopic reduction and stabilization. The principle of treatment is to reduce the lunate and scaphoid in normal alignment and stabilization with K-wires. Under fluoroscopic control and longitudinal traction, the arthroscope is placed in the 3-4 radiocarpal portal. 1.5 mm × 10 mm K-wires are inserted percutaneously taking care not to damage the sensory cutaneous branches of the radial nerve. Leverage between the head of the capitate and the posterior horn of the lunate can provide a satisfactory reduction. Sometimes K-wires in the scaphoid and the lunate used as joysticks can control the rotation of the carpal bones. Normally 2 or 3 K-wires are placed across scapholunate space (Fig. 11.9). The K-wires are left buried under the skin and the patient is immobilized in a below-elbow splint. Ideally, the pins are removed at 8 weeks postoperatively. Rehabilitation of the wrist is commenced after removal of the K-wires and the recovery of normal mobility and strength usually requires 3 months approximately.


Fig. 11.9
X-rays control after reduction and fixation with two pins of a scapholunate ligament injury
In GEISSLER stage IV lesions, repair by conventional open surgery is classically described. The incision passes between the third and fourth dorsal extensor compartments. The extensor pollicis longus is released from its compartment and retracted radially. The extensor digitorum tendons are retracted medially. The dorsal capsule is opened. The dorsal portion of the scapholunate ligament is repaired using small anchors and a non-absorbable suture and the repair is protected with K-wires passed from the scaphoid into the lunate. Typically, a radial dorsal capsular flap is fixed to the lunate with the aid of a small anchor. The dorsal capsule is meticulously repaired. The K-wires are usually left for 8 weeks, when they are removed before starting rehabilitation.
Chronic Scapholunate Ligament Injuries
The treatment of chronic scapholunate ligament injuries poses the most difficult challenge for hand surgeons. In fact, untreated chronic scapholunate instability eventually leads to arthritic changes in the long term [3, 4]. Very often the diagnosis is delayed and is made at an advanced stage in which arthritic changes have already set in making salvage procedures imperative and precluding sporting activities, especially among athletes. The importance of treating these injuries as soon as possible cannot be overemphasized.
Numerous reconstruction techniques have been described in literature [5–27]; however they all result in loss of mobility in an attempt to restore the stability of the SL joint.
Recently a new technique of arthroscopic repair of the dorsal capsule-ligamentous portion of the SLIOL has been described to treat all stages of acute and chronic SL ligament injuries, with encouraging results [28]. The advantage of this new technique appears to be the preservation of mobility compatible with sporting activities. Some professional athletes with chronic, severe injury to the scapholunate ligament were able to resume their sporting activities.
Surgical Technique
The surgery is performed on an outpatient basis under regional anesthesia and with an upper arm tourniquet. The elbow is flexed to 90° on an arm table and the hand is suspended by means of a hand holder with traction of 3–5 kg.
Standard arthroscopic 3-4 and 6R portals for the radiocarpal joint and MCR and MCU for the midcarpal joint are used. The joints are insufflated with normal saline. A small transverse incision is made with a 15 number scalpel followed by blunt dissection with a mosquito forceps. The 2.4 mm arthroscope is introduced through the 3-4 portal and the instruments through the 6R portal—these two portals are interchangeable according to need. The midcarpal joint is explored through the MCU portal. Exploration and palpation of the structures in the two joints confirm the lesion and provide the staging.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








