CHAPTER 20 Arthroscopic Rim Resection and Labral Repair
Technique
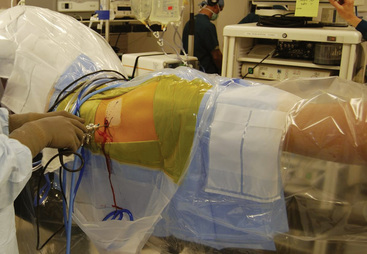
All of our arthroscopic hip techniques are performed with the patient in the supine position. After a lumbar plexus block and a general anesthetic are administered to the patient, we are very meticulous with our setup. The patients’ feet are wrapped in protective boots and placed in leather foot holders at the foot of the bed. Each lower extremity is attached to a bar that is freely mobile for abduction, adduction, flexion, and extension. The nonoperative extremity is placed in approximately 60 degrees of abduction, whereas the operative extremity will eventually be placed in neutral abduction. Before the feet are wrapped, electromyography monitors are placed near the tibial nerve for continuous monitoring during the procedure. After baseline signals are achieved, we are ready to begin the distraction of the operative extremity for optimal portal site placement. A C-arm fluoroscopy device is used to verify the amount of joint distraction that is achieved. The foot is internally rotated 90 degrees and then locked in place; this allows us to place the proximal femur nearly parallel with the floor. After the radiographic verification of adequate distraction is attained, we remove the C-arm and prepare the patient in a standardized fashion. A picture of our standard setup is shown in Figure 20-1.
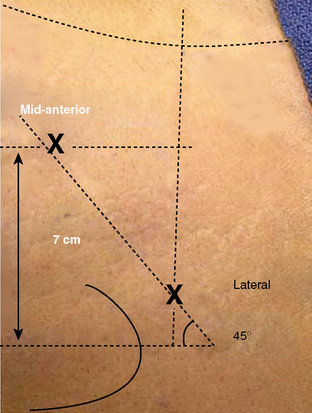
We draw out specific landmarks on the patient’s leg to properly identify the ideal location for our portals. The anterosuperior iliac spine and the outline of the greater trochanter are the most important of these landmarks. From the tip of the greater trochanter, we measure proximally 1 cm and anteriorly 1 cm; this is the ideal location for our lateral portal. From that site, we measure a distance between 5 cm and 6 cm distal and anterior on a 60-degree plane from horizontal for the placement of our unique mid-anterior portal (Figure 20-2). In our experience, these two portals are all that are necessary to achieve the adequate visualization of the most important aspects of both the central and peripheral compartments of the hip joint. We have also substantially reduced the morbidity associated with portal placement over the past year with the new position of our mid-anterior portal.
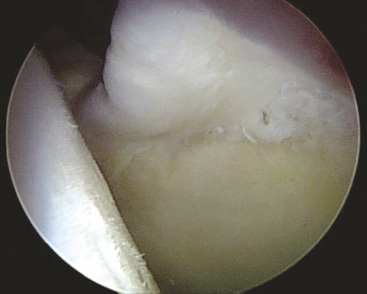
Now that we have established a portal for the arthroscope and a working portal, we can begin the diagnostic portion of the arthroscopy to visualize all aspects of both the central and peripheral compartments. Our attention is first directed to the chondrolabral junction. We use a probe to determine if there are any areas in which the labrum has been separated from the acetabular rim. It is typical with cam-type impingement to see delamination of the acetabular cartilage at the site of the labral detachment. With the use of the blunt end of a shaver or with a probe, it is possible to see a “wave sign”: the cartilage will buckle at sites where the labrum is damaged but not yet detached from the acetabular rim (Figure 20-3). It is very important to inspect these areas carefully. If they are not addressed at the time of the initial surgery, they can be the source of recurrent pain and disability as the junction between the labrum and the delaminated cartilage degenerates.
Rim trimming
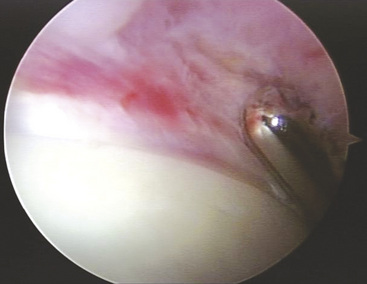
The typical pincer lesion is produced as a result of an abnormal growth of bone at the anterosuperior portion of the acetabulum (Figure 20-4). The pincer can be either primary or secondary to the chronic abutment of the femoral neck on the acetabular rim. With respect to the normal anatomy and position of the acetabulum, this area creates a relative retroversion to the acetabulum. The x-rays in Figure 20-5 show this crossover sign. This is an area in which the anterior wall is farther lateral than the posterior acetabular rim. The goals of the rim resection should be to remove this area of bone and to restore the normal anatomy and relative position of the acetabulum with respect to the pelvis and the femoral neck. If this area is not addressed, subsequent labral damage and delamination of the cartilage will continue. Typically, this anterosuperior region of the acetabular rim also corresponds with the area of labral pathology. If the tear does not extend to this region, it is necessary to detach the labrum at this site for the proper resection of bone. After this has been completed, the labrum can then be reattached with the use of suture anchors.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree