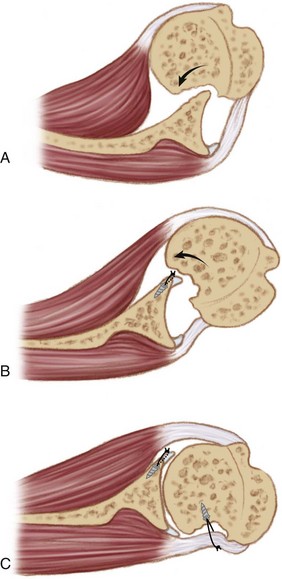
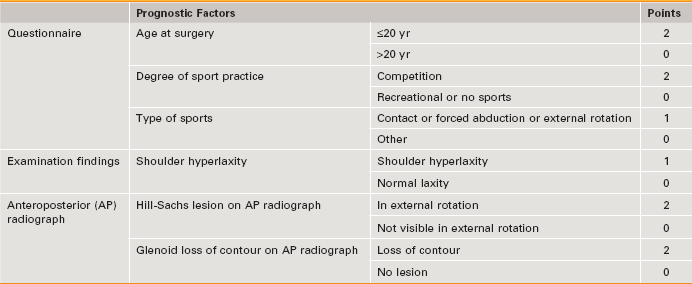
Chapter 17 Recurrence rates of up to 15% have been reported after arthroscopic labral repair for anterior shoulder instability.1 Patient age and activity level, soft tissue quality, and the presence of glenoid or humeral bone loss have been identified as predisposing factors.2 A number of potential therapeutic options exist for the management of humeral lesions that are contributing significantly to the instability complex. These include open matched osteoarticular allograft transplantation, transhumeral bone grafting, humeroplasty, rotational humeral osteotomy, and partial or complete humeral head resurfacing.3–7 In arthroscopic Hill-Sachs remplissage (AHSR), a procedure pioneered by Wolf,8 adapted from the open technique described by Connolly,9 the infraspinatus tendon and posterior capsule are used to fill the humeral defect. The term remplissage derives from the French verb remplir, meaning “to fill.” This posterior capsulotenodesis is not intended as an isolated procedure, but rather is always performed in combination with an anterior soft tissue repair. Through “filling” of the defect, the defect is rendered extra-articular and thus is prevented from engagement with the glenoid. In addition, the infraspinatus tendon and capsule act as a checkrein, preventing anterior humeral head translation10 (Fig. 17-1). History and Physical Examination Signs of anterior and inferior apprehension and hyperlaxity are sought. Anterior hyperlaxity is present if the examiner can easily subluxate the humeral head out of the socket in the anteroposterior (AP) direction on drawer testing or if passive external rotation is greater than 85 degrees with the patient’s arm at his or her side. Inferior hyperlaxity is assessed with sulcus sign testing and the hyperabduction test, the result of which is positive with a minimum of 20 degrees of asymmetrical abduction at the glenohumeral joint.11 The presence of skin striae can be a subtle but useful finding suggestive of a predisposition toward soft tissue laxity. To assist in the surgical decision-making process for cases of anteroinferior instability, a preoperative scoring system—the instability severity index score (ISIS)—was developed.12 It enables selection of patients at high risk for treatment failure after isolated arthroscopic Bankart repair. Six risk factors, shown to predict an increased recurrence rate after surgery, were integrated into a 10-point scale (Table 17-1). A score of 3 or fewer points correlates with an acceptable postsurgical recurrence risk of 5% and therefore potential suitability for isolated arthroscopic Bankart repair. For a score of 4 to 6, the recurrence risk is 10%; risk of recurrence rises to 70% with a score over 6. The associated soft tissue and osseous defects dictate the supplemental procedure, performed in addition to a Bankart repair, required to minimize recurrence in patients with an ISIS score higher than 3 (Fig. 17-2). In the senior author’s practice, a combined arthroscopic Bankart and Hill-Sachs remplissage (BHSR) procedure is performed for approximately 10% of cases requiring surgical treatment of anterior shoulder instability.
Arthroscopic Remplissage for Management of Engaging and Deep Hill-Sachs Lesions
Preoperative Considerations
Instability Severity Index Score
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Arthroscopic Remplissage for Management of Engaging and Deep Hill-Sachs Lesions