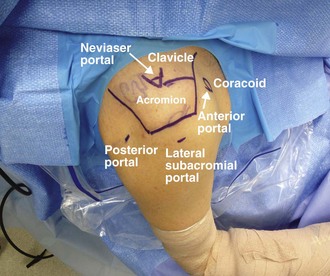
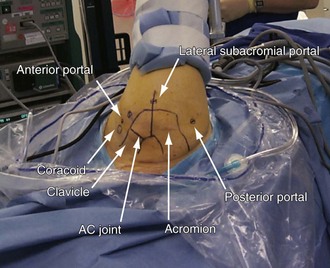
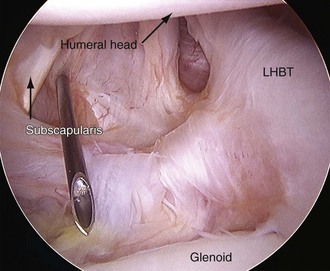
Chapter 1 Shoulder arthroscopy has become an invaluable diagnostic and therapeutic tool for the sports medicine surgeon. Through innovative thinking and technical advancement, we continue to refine our ability to recognize and treat shoulder disorders with use of minimally invasive techniques. Shoulder arthroscopy has been shown to be both safe and effective when compared with open surgery. In a series of more than 14,000 procedures, the overall complication rate of shoulder arthroscopy was 0.56%.1 Arthroscopic surgery offers the potential benefits of reduced operative time, decreased postoperative pain, decreased surgical scarring, improved cosmesis, and the ability to perform outpatient surgery. In addition, complications related to the subscapularis inherent to the deltopectoral approach can be avoided. Shoulder arthroscopy has demonstrated equivalent or superior outcomes to open procedures for a variety of shoulder conditions.2–4 For the beach chair position, the patient is positioned supine and the back of the bed is elevated to 60 degrees (Fig. 1-1). The patient is positioned such that the medial border of the scapula is just lateral to the lateral aspect of the bed. A rolled towel placed just medial to the scapula may improve operative positioning. For the lateral decubitus position, the patient is supported with either a vacuum beanbag or a combination of bolsters, kidney rests, chest strap, foam headrest, and axillary roll (Fig. 1-2). Visualization may be more anatomic if the patient is tilted 20 to 30 degrees posteriorly to bring the face of the glenoid parallel to the floor. Care should be taken to protect and pad superficial bony landmarks of the lower extremities. Ten pounds of traction is typically adequate. The lowest amount of weight (maximum 15 pounds) and shortest time of traction (maximum 2 hours) necessary to perform the procedure are recommended. In addition to axial traction, joint distention may be augmented by the addition of secondary traction close to the axilla and perpendicular to the joint. Caution should be exercised with dual traction setups to avoid distal hypoxemia. Alternatively, a sterile rolled towel placed deep into the axilla may provide improved joint distention without the need for a dual traction setup. For access to the subacromial space, smaller degrees of flexion and abduction can provide inferior distraction of the humeral head and an improved subacromial view. After induction of anesthesia but before sterile preparation and draping, an examination with the patient under anesthesia (EUA) should be performed. Both the operative and nonoperative limb should be examined, if possible. Degrees of abduction, forward elevation, and internal and external rotation in adduction and abduction, respectively, should be documented. Restrictions in motion may be observed in patients with adhesive capsulitis, glenohumeral arthritis, or frank shoulder dislocation. In patients with a history of instability, an examination for shoulder laxity should be performed via load and shift testing. After application of a force to center the humerus on the glenoid, the humerus is translated in both an anterior and a posterior direction while 90 degrees of abduction are maintained. Translation is graded as 0 for no translation, 1+ for trace translation, 2+ for translation to the edge of the glenoid, and 3+ for translation over the edge of the glenoid. Laxity to an inferiorly directed humeral force in adduction is documented as 0 for no humeral movement, 1+ for 1 cm of inferior humeral movement, 2+ for 2 cm of humeral movement, and so on.2 If external humeral rotation dampens the inferior translation, the rotator interval may need to be addressed in addition to other sources of pathologic shoulder laxity. After EUA the shoulder is prepared and draped in a sterile fashion. For the beach chair position, a sterile drape is placed over the arm holder for sterile intraoperative readjustment. For the lateral decubitus position, the arm is wrapped with Coban (3M, St Paul, Minnesota) for sterile arm traction up to but not including the wrist to avoid superficial radial nerve compression. Indelible ink is used to mark the anterior and posterior borders of the clavicle, borders of the acromion, and scapular spine. The AC joint and the coracoid process are identified and marked (see Figs. 1-1 and 1-2). The anterior portal is best placed with an “outside-in” technique, through use of a spinal needle placed under direct arthroscopic visualization (Fig. 1-3). The position of the anterior portal may vary based on the goals of the procedure. For anterior instability, placement of the portal just above the subscapularis is desirable. The portal may be placed more centrally within the rotator interval for routine diagnostic arthroscopy (Fig. 1-4). Superficially, this portal is located just lateral to the coracoid process. It travels between the deltoid muscle (axillary nerve) and the pectoralis major (lateral and medial pectoral nerves). In the deeper layer the anterior portal travels in the interval between the supraspinatus (suprascapular nerve) and the subscapularis (upper and lower subscapular nerves). The portal is also inferior to the long head of the biceps tendon (LHBT) and just lateral to the middle glenohumeral ligament (MGHL). Safety of the anterior portal is ensured by making the portal under direct visualization, incising only the skin and subcutaneous tissue with the scalpel, and remaining lateral to the coracoid process, protected from critical neurovascular structures.
Patient Positioning, Portal Placement, Normal Arthroscopic Anatomy, and Diagnostic Arthroscopy
Patient Positioning
Portal Placement
Anterior Portals
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Patient Positioning, Portal Placement, Normal Arthroscopic Anatomy, and Diagnostic Arthroscopy