CHAPTER 10 Arthroscopic Radial Head Resection
Radial head resection is a useful treatment alternative for symptomatic radiocapitellar or proximal radioulnar joint pathology. Radial head excision may improve forearm rotation and reduce impingement between the radial head and the capitellum or proximal ulna. Most reports in the literature involve open radial head resection.1 Arthroscopic radial head resection has been described only recently,2 and reports of outcomes are limited.3–5 However, as experience with arthroscopic radial head resection continues to increase, we expect more evidence to be forthcoming.
ANATOMY AND BIOMECHANICS
The radial head is an important stabilizer of the elbow. A number of biomechanical studies have investigated the effect of radial head resection on the kinematics and stability of the elbow. The radial head is particularly important as a stabilizer in the setting of valgus instability due to medial collateral ligament insufficiency.6–9 It is also important in tensioning the lateral collateral ligament,7 and posterolateral rotatory instability has been reported after radial head excision in vitro7,10 and clinically.11,12 The role of the radial head in axial stability of the forearm is evident by the common finding of proximal migration of the radius after radial head resection.13–17
Radial head excision results in increased loading of the remaining ulnohumeral articulation. This effect is caused by the altered elbow kinematics and the fact that the loads originally borne by the radiocapitellar articulation must be accepted by the ulnohumeral joint.8 Although this increased ulnohumeral load has not been studied biomechanically, it is thought to explain the high incidence of ulnohumeral osteoarthritis reported in patients after acute radial head resection for radial head fractures.14–17 Extensive biomechanical evidence supports the beneficial stabilizing effects of prosthetic replacement of the radial head.7–9,18,19 These findings suggest that, whenever possible, the radial head should be replaced after it is resected, particularly in cases of acute trauma, in which occult ligament injuries are common.
PATIENT EVALUATION
History and Physical Examination
A detailed physical examination should be performed. The carrying angle and bony contours of the elbow should be observed. Prior traumatic and surgical incisions should be documented. The range of motion of the elbow and forearm should be measured with the use of a goniometer. The examiner should confirm that the proximal radius articular deformity is the impediment to rotation. Motion can be lost as a result of soft tissue or osseous deformities. The synovial tissue in patients with hemophilic arthropathy is hypertrophic, highly vascular, and prone to impingement between the articular surfaces.22 A soft end point suggests a soft tissue cause, whereas a firm end point suggests osseous impingement. The distal radioulnar joint may be contributing to the forearm rotational stiffness.
Physical examination and imaging of the wrist are important, especially in patients with prior traumatic injuries, congenital deformities, and rheumatoid arthritis, in which distal radioulnar joint pathology is common. A careful examination of elbow and forearm stability is critical because valgus, posterolateral rotational, and axial instability are contraindications to radial head resection. Joint laxity may be caused by loss of articular cartilage, ligament attenuation resulting from chronic inflammation, or prior traumatic injuries. The examination for valgus instability includes valgus stress testing,26,27 the milking maneuver,28 and the moving valgus stress test.29 The examination for posterolateral rotatory instability includes the pivot shift test,12 the posterolateral drawer test,30 and the supine and seated push-up tests.31,32 Longitudinal radioulnar instability is difficult to detect on clinical examination. These patients often have tenderness or dorsal prominence of the ulna at the distal radioulnar joint.
Diagnostic Imaging
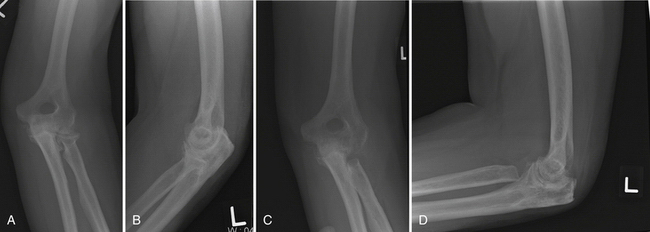
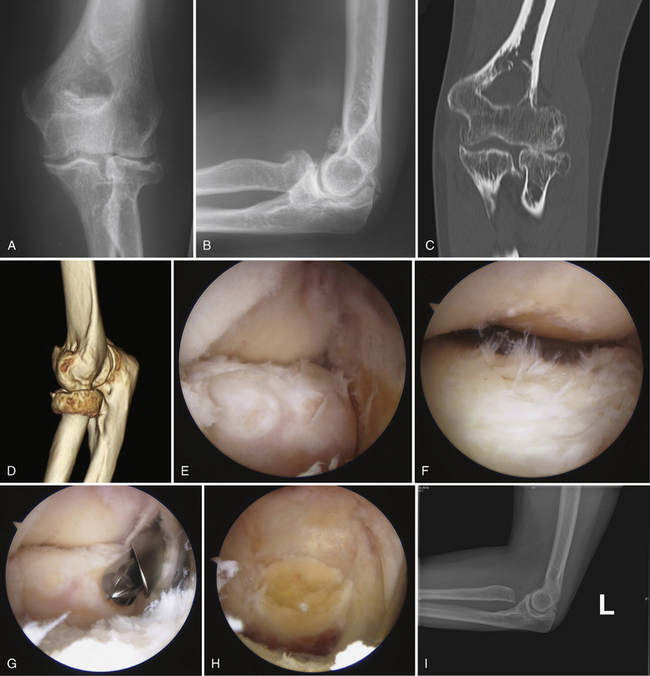
Imaging can confirm the presence of a proximal radius articular deformity or arthritis (Fig. 10-1). In addition to anteroposterior and lateral views, a radiocapitellar view can help to throw the radial head into profile. Bilateral radiographs of the wrists should be performed to assess for other contributions to the painful or limited rotation, such as radioulnar synostosis or distal radioulnar joint pathology, and to assess for longitudinal radioulnar dissociation. Stress views or a fluoroscopic examination should be considered to rule out valgus, varus, and axial instability if there is any concern resulting from the physical examination. Computed tomography (CT) with sagittal, coronal, and three-dimensional reconstructions can better define the bony anatomy (Fig. 10-2). CT may offer additional information about the ulnohumeral, radiocapitellar, and proximal radioulnar joint spaces and about articular congruity. Loose bodies and heterotopic ossification also may be better defined. Resecting the radial head without addressing these other osseous deformities may result in suboptimal results.
TREATMENT
Indications and Contraindications
The most common conditions for which arthroscopic radial head resection has been described are rheumatoid arthritis3–5,20,21 and post-traumatic arthritis (particularly radial head fractures).2–5,20,21 Radial head resection is sometimes indicated for hemophilic arthropathy of the elbow. Chronic hemophilic synovitis of the elbow can lead to enlargement and irregularity of the radial head. The margins of this hypertrophic radial head impinge against the proximal ulnar facet, acting as a mechanical block to forearm rotation. Reports in the literature of radial head resection for hemophilic arthropathy are limited to open techniques.22–25 Congenital and acquired radial head dislocations can also be treated by arthroscopic radial head resection in selected cases. Surgical intervention is typically reserved for symptoms refractory to nonoperative measures, such as activity modification and anti-inflammatory drugs. In the setting of rheumatoid arthritis, this includes an adequate trial of disease-modifying medications.
Radial head excision is contraindicated in patients with valgus, posterolateral rotatory, or axial instability. The loss of this secondary stabilizer can exacerbate preexisting instability. Advanced ulnohumeral arthritis is a relative contraindication because radial head excision alone cannot address symptoms originating from the ulnohumeral articulation. Radial head excision results in increased loading of the remaining ulnohumeral articulation, which may further exacerbate ulnohumeral joint pain.8 Radial head replacement and radiocapitellar replacement can be considered when isolated radial head excision is contraindicated, such as in the setting of instability.33 Older, lower-demand patients with advanced articular destruction and bony deformity may be better treated with a total elbow arthroplasty. Arthroscopic excision of the radial head usually is not recommended for acute radial head fractures because of the high incidence of concomitant ligament injuries.34,35 The torn capsule in the acute fracture setting can result in significant extravasation of fluid, making it a higher-risk procedure and more technically challenging.
A surgeon’s inexperience with arthroscopy of synovitic elbows can be considered a relative contraindication. Arthroscopy of synovitic elbows is technically demanding because synovial proliferation, stiffness, and deformity result in diminished capsular volume, reducing the available working room in the elbow.36
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree