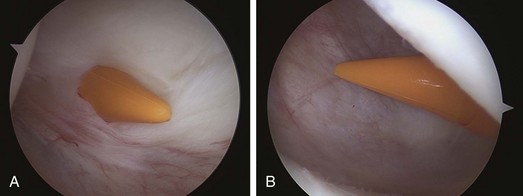
Chapter 83 Injuries to the posterior cruciate ligament (PCL) occur more frequently than previously thought, not only among patients who sustain severe trauma of the lower extremity, but also among athletes. Surgical reconstruction of the PCL is recommended for acute injuries that result in severe posterior tibial subluxation and instability, objective criteria that are often met in patients with combined ligamentous injuries. Surgical treatment of the chronic PCL-deficient knee is recommended for patients with persistent symptomatic complaints, such as pain or discomfort that fails to improve with an appropriate physiotherapeutic program. The rationale for performing a reconstruction is to restore normal joint kinematics and forces, thus minimizing the deleterious effects, such early cartilage degeneration, that PCL deficiency has been shown to have on the knee. With these premises in mind, we developed a technique of arthroscopic tibial inlay reconstruction1 to minimize the graft stresses and allowing a more anatomic reconstruction. This concept has more recently also been applied at the femoral side.2 Numerous PCL reconstruction techniques have been described in the literature. Since its first description by Clancy and colleagues3 in 1983, single-bundle PCL reconstruction has become a popular surgical option. Its focus is on the reconstruction of the larger, stiffer AL bundle via arthroscopic assistance. It has been reported that the grafted substances can be stretched owing to the concentration of stress caused by the acute angle between the graft and the intra-articular apertures of the tunnels. Therefore tibial inlay reconstruction has been proposed as an alternative technique to the transtibial tunnel single-bundle technique since early 1990s.4 Rather than using a tunnel for tibial attachment, the tibial inlay technique uses a bone trough at the tibial site of PCL insertion to which the bone block of the graft is directly fixed. This type of reconstruction has the specific aim of restoring normal knee kinematics by achieving a more anatomic tibial fixation and by avoiding what has been described as the “killer turn.”5 However, no clear evidence of biomechanical superiority has been demonstrated from either a biomechanical or a clinical standpoint.6,7 Furthermore, the need for an open approach and the specific setup for performance of a tibial inlay reconstruction have decreased its appeal for some orthopedic surgeons. Positioning, Examination Under Anesthesia, and Portals The patient is positioned on the operating room table in the decubitus position with the knee flexed to 70 to 90 degrees, with the foot on the table. A standard arthroscopic inspection is carried out with the usual AL and anteromedial (AM) standard approaches. The key point in this technique is the use of two additional portals—the PM and the posterolateral (PL)—which allows the surgeon to perform the transseptal technique (Fig. 83-1).
Arthroscopic Posterior Cruciate Ligament Inlay
Preoperative Considerations
History
Surgical Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Arthroscopic Posterior Cruciate Ligament Inlay