Arthroscopic Pcl Reconstruction: Transtibial and Arthroscopic Inlay Techniques
Matthew V. Smith
Jon K. Sekiya
Posterior cruciate ligament (PCL) injuries are relatively uncommon compared with anterior cruciate ligament (ACL) injuries. Unlike the ACL, the PCL has the potential to heal (1, 2). However, this does not always result in normal knee kinematics (3, 4 and 5). Despite this, outcomes after nonoperative treatment for isolated PCL injuries have been favorable (6, 7). Therefore, nonoperative treatment has been advocated for most isolated PCL injuries. However, patients with chronic PCL deficiency can develop pain and disability over time (8). Currently, controversy exists about the surgical indications for the treatment of isolated PCL injuries. Additional controversy exists regarding the appropriate surgical technique to treat PCL-deficient knees. In this chapter, we discuss the evaluation and management of the PCL-deficient knee, highlighting the transtibial single-bundle PCL augmentation technique and the arthroscopic inlay technique.
CLINICAL EVALUATION
Although ACL injuries commonly occur as a result of a noncontact deceleration injury, isolated PCL injuries usually occur from a direct blow to the knee or from a hyperextension injury. A direct blow can occur in motor vehicle accidents when the proximal tibia directly impacts the dashboard with knee in flexion. A PCL injury can also occur during athletic activities when the proximal tibia strikes the ground with the foot in plantar flexion (6). Although PCL injuries can occur with varus, valgus, or twisting forces, these injuries are often associated with collateral ligament injuries. Because of PCL injuries are less common than ACL injuries, PCL injuries are often overlooked during evaluation after a knee injury. Unfortunately, these injuries can be subtle and patients may not know exactly how or when the injury occurred. Despite this, it is important to try and clarify the mechanism of injury to help determine the diagnosis.
In addition to clarifying the mechanism of injury, it is important to determine the timing of injury, as an acute PCL tear may require a different treatment than a chronic tear. It is also important to know if the patient had a previous knee injury that may explain any ligamentous laxity. Age and activity level are key factors in determining treatment options, particularly in patients with partial PCL tears. In addition, it is essential to understand the patient’s occupational requirements. When considering surgical treatment in patients with chronic PCL deficiency, it is imperative to determine if pain or instability is the primary complaint. Chronic PCL deficiency has been associated with a higher incidence of medial compartment and patellofemoral chondral damage as well as meniscal tears (9). PCL reconstruction in a painful and degenerative knee may not yield favorable results.
Physical Examination
The physical examination of an injured knee starts with inspection for swelling and ecchymosis. An effusion is likely to develop with an acute PCL injury. Swelling or ecchymosis on the medial or lateral aspect of the knee should heighten concern for a collateral ligament or capsular injury. As with any lower extremity injury, thorough evaluation and clear documentation of the neurovascular status of the affected extremity is critical, especially in multiple ligament knee injuries (10). Peroneal nerve injury has been reported between 13% and 16% in posterolateral corner (PLC) injuries (11, 12).
After evaluating the neurovascular status of the limb, a thorough ligamentous exam should be performed. In patients with a PCL injury, the posterior sag of the tibia reduces with the anterior force applied during a Lachman exam. This may give the examiner the impression that the Lachman’s is positive even though the ACL is intact. Prior to performing the Lachman’s exam, be sure that the proximal tibia is approximately 1 cm anterior to the medial femoral condyle. Anterior drawer findings and a quadriceps active test (tibia reduces with quad muscle activation) may help to clarify the injury pattern. Evaluation of varus and valgus laxity as well as rotary instability is a critical part of evaluating a PCL-deficient knee since associated ligament injuries are common (13). Rotary instability may result from a PLC injury. PLC deficiency has been shown to increase graft forces after PCL reconstruction (14). The PLC
is assessed with the Dial test. A patient with an isolated PLC injury will demonstrate 10° to 15° of increased external rotation at 30° of knee flexion compared with the opposite side. PCL- and PLC-deficient knees will also show increased external rotation at 90° of flexion. Lastly, in patients with subacute or chronic injuries, it is important to evaluate the overall static and dynamic limb alignment. A chronic untreated PLC injury may result in a dynamic varus thrust that should be treated with an osteotomy prior to any ligament reconstruction.
is assessed with the Dial test. A patient with an isolated PLC injury will demonstrate 10° to 15° of increased external rotation at 30° of knee flexion compared with the opposite side. PCL- and PLC-deficient knees will also show increased external rotation at 90° of flexion. Lastly, in patients with subacute or chronic injuries, it is important to evaluate the overall static and dynamic limb alignment. A chronic untreated PLC injury may result in a dynamic varus thrust that should be treated with an osteotomy prior to any ligament reconstruction.
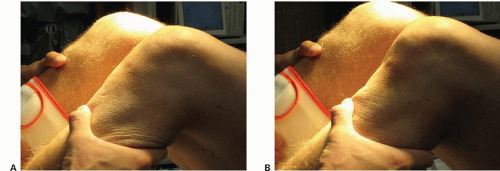
PCL injuries are graded by the posterior drawer, which amount of posterior translation of the tibia relative to the femur with knee at 90° of flexion. The posterior drawer is the most accurate test to identify PCL deficiency (15) (Fig. 74.1). This can be evaluated clinically and radiographically. Grade 1 injuries demonstrate less than 5 mm of posterior tibial translation. Posterior tibial translation between 5 and 10 mm is considered a grade 2 injury. Greater than 10 mm of posterior translation is considered a grade 3 injury. In patients with grade 3 PCL injuries, it is important to closely evaluate the PLC as biomechanical studies have shown that PLC sectioning is required to get grade 3 posterior tibial translation in a PCL-deficient knee (16, 17 and 18). Clinically, if the proximal tibia translates to a level flush with the medial femoral condyle but not farther, it is likely a grade 2 PCL injury. If the proximal tibia drops posterior to the medial femoral condyle, it is likely a grade 3 injury.
Imaging
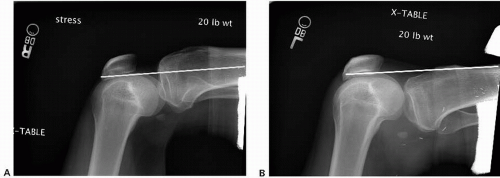
Radiographic evaluation of an injured knee starts with plain X-rays. Necessary views include an anterior-posterior (AP), a lateral, and an oblique view. Avulsion fractures of the tibial insertion should be evident on these views. A notch view, a Merchant’s view, and a weight-bearing 45° flexion posterior-anterior view are additional views that may provide important information in chronic PCL injuries. In patients with chronic PCL deficiency, standing long-leg alignment films are useful to determine the presence of malalignment. Stress radiographs with TELOS or with 20 lb (9.07 kg) of posterior force applied to the tibia with the knee in 70° to 90° of flexion can provide an objective measure of injury grade compared with the contralateral knee (Fig. 74.2). Gravity lateral views comparing both knees can be used if stress views cannot be performed.
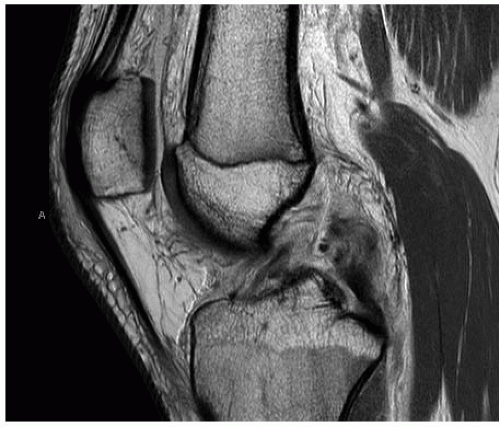
MRI is the imaging modality of choice to evaluate the integrity of the soft tissues in the knee. MRI is especially useful in identifying acute PCL injuries (19) (Fig. 74.3). It can also help define associated ligament injuries, meniscal injuries, and chondral injuries. Chronic PCL injuries may not be evident on MRI as healing may take place over time (1). Therefore, it is important to rely on the clinical exam findings to determine the pattern of injury. In addition to MRI, dynamic ultrasound has been shown to be effective in diagnosing associated PLC injury (20). This may be particularly helpful in subacute or chronic PLC injuries when MRI does not clearly demonstrate injury.
TREATMENT
Treatment for acute PCL injuries continues to evolve. Traditionally, nonoperative management of isolated acute PCL tears has been advocated. Nonoperative treatment of isolated acute PCL tears includes bracing in full knee extension for at least 2 weeks to reduce the posterior sag of the tibia relative to the femur during healing (21, 22). During rehabilitation, emphasis is placed on quadriceps strengthening since patients with good quadriceps strength tend to have better functional outcomes (7). In addition, hamstring strengthening is discouraged during the healing phase to minimize posteriorly directed forces across the knee. While short-term results of nonoperative treatment are favorable, good outcomes can diminish over time (6, 7 and 8). Keller et al. (8) reported that 90% of patients with PCL deficiency complained of knee pain with activity and 43% complained of problems with walking at an average of 6 years after injury. This has led some to advocate
for earlier surgical intervention, especially in patients with higher grade PCL injuries, as surgical outcomes are generally good with up to 90% patient satisfaction (13, 23, 24 and 25). Current operative interventions have failed to consistently improve posterior laxity to normal (23, 24, 26, 27). However, the degree of PCL laxity does not appear to correlate with outcomes (28). On the other hand, outcomes after acute and subacute (<3 months) surgical intervention for PCL deficiency are better than those after surgical intervention for chronic injuries (23). Nonoperative treatment in patients with multidirectional instability from a combined PCL and associated ligament injury do not fair as well as those with isolated PCL injuries (29).
for earlier surgical intervention, especially in patients with higher grade PCL injuries, as surgical outcomes are generally good with up to 90% patient satisfaction (13, 23, 24 and 25). Current operative interventions have failed to consistently improve posterior laxity to normal (23, 24, 26, 27). However, the degree of PCL laxity does not appear to correlate with outcomes (28). On the other hand, outcomes after acute and subacute (<3 months) surgical intervention for PCL deficiency are better than those after surgical intervention for chronic injuries (23). Nonoperative treatment in patients with multidirectional instability from a combined PCL and associated ligament injury do not fair as well as those with isolated PCL injuries (29).
Operative intervention for acute PCL injuries is clearly indicated in patients with a bony avulsion of the PCL tibial insertion, in combined ligamentous injuries and in knee dislocations unless there is a contraindication to surgery like poor health status or poor functional status. Operative intervention for isolated PCL tears remains controversial. Surgery may be warranted in patients with persistent symptoms of instability or pain after a trial nonoperative management. Operative treatment options for PCL injuries include PCL repair, PCL augmentation, and PCL reconstruction. Primary PCL repair alone has generally fallen out of favor because of average results (30). There may be a role for passing sutures into the PCL remnant and pulling it into the femoral tunnel with a graft during PCL augmentation (31). Transtibial single-bundle PCL augmentation with autograft or allograft can be used to improve stability in partial PCL tears where the PCL is intact but lax (32). This is particularly helpful in acute injuries when the PCL still has the potential to heal. PCL reconstructions for complete tears can be done with single-bundle or double-bundle grafts using transtibial or inlay techniques.
Single-Versus Double-Bundle PCL Reconstruction
The PCL consists of two main bundles, anterolateral (AL) and posteromedial (PM) (33). The AL bundle originates more anterior on the lateral face of the medial femoral condyle than the PM bundle. The AL bundle inserts more lateral than the PM bundle on the tibial fovea. The AL bundle is tight in flexion, whereas the PM bundle tightens in extension. With the knee in full extension, there is little translation of the tibia relative to the femur in a PCL-deficient knee (34, 35). Therefore, reconstructing the AL bundle is the key component to PCL reconstruction. The addition of a PM bundle reconstruction has been shown to improve stability in biomechanical testing by decreasing posterior tibial translation and enhancing rotational control, especially in a PLC-deficient knee (18). Since PLC injuries commonly accompany PCL injuries, the improved rotational control provided by a double-bundle reconstruction may improve knee kinematics more so than a single-bundle reconstruction (Fig. 74.4). However, there is evidence that a double-bundle PCL reconstruction may over constrain the knee when the PLC is intact (18). The addition of a PM bundle may also increase AL bundle graft
tension especially if the PM bundle is not placed in the correct position on the femur (36). Currently, there are no clinical studies that demonstrate improved outcomes comparing the two techniques (25, 37, 38 and 39).
tension especially if the PM bundle is not placed in the correct position on the femur (36). Currently, there are no clinical studies that demonstrate improved outcomes comparing the two techniques (25, 37, 38 and 39).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree