CHAPTER 24 Arthroscopic Management of the Trauma Patient
Introduction
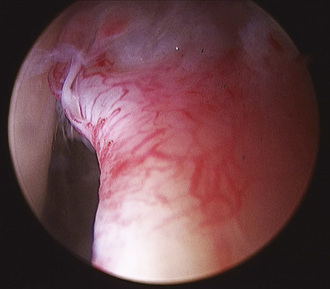
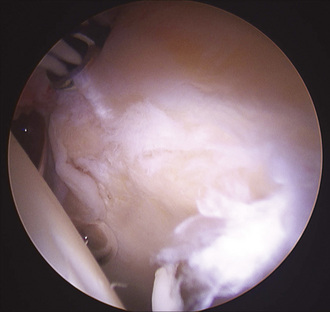
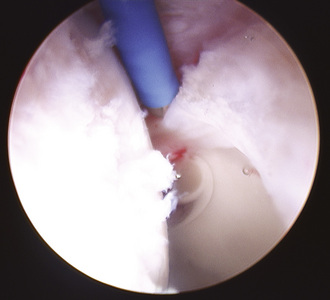
Hip arthroscopy has been described as part of treatment regimens for hip trauma and related sequelae for decades, but the role of hip arthroscopy for this application has expanded rapidly during recent years. As early as 1931, Burman noted a role for a form of hip arthroscopy for loose body or fragment removal. The role for surgical debridement of the hip expanded substantially with the observation that loose bodies were ubiquitous with hip fracture dislocations. Epstein advised that all hip fracture–dislocations should be treated with debridement in an attempt to delay the appearance of traumatic arthritis and to minimize its severity. He advocated open debridement rather than arthroscopic debridement. The prevalence of loose bodies after injury to the hip and their impact on the development of hip joint arthrosis certainly contributed to the imperfect long-term results of dislocations and fractures around the hip joint (Figures 24-1 and 24-2). Until recently, loose bone and cartilage fragments were almost always retrieved with open arthrotomy. Advances in arthroscopic tools and techniques have made arthroscopic loose-body removal highly efficient. Arthroscopy advantages include diminished blood loss, smaller incisions, decreased recovery time, reduced potential for neurovascular damage, and decreased disruption of capsuloligamentous structures. Indications for arthroscopic debridement after trauma have been extended to include the extraction of bullets, the removal of broken hardware from the joint, and joint lavage for the treatment of infection or contamination in association with bullet fragments passing through the bowel and communicating with the hip joint.
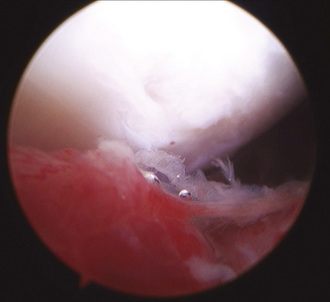
Figure 24–2 Another view of the same patient shown in Figure 24-1. Femoral head chondrolysis is evident. Intervention was limited to labral debridement, chondroplasty of the femoral head, and lavage.
The arthroscopic treatment of acetabular labral pathology most typically involves atraumatic tears or labral disease associated with impingement or hip dysplasia. Isolated cases of traumatic labral pathology have been reported since 1959, when Dameron described a bucket-handle tear of the acetabular labrum that prohibited the reduction of a posterior dislocation of the hip that subsequently required open repair. Labral injury has more recently been described as a relatively common but previously poorly recognized phenomenon in association with acetabular fractures. Ganz described reproducible labral pathology in 14 patients with displaced transverse acetabular fractures who had been treated with open reduction and internal fixation. The labrum was partially or completely detached from the superior acetabular rim in all cases. In this series, an avulsed portion of the labrum was left if it was stable and undamaged, resected if it was unstable and damaged, and repaired if it was unstable but intact or attached to a bony fragment. Ganz proposed arthrotomy at the time of acetabular fracture fixation to search for associated intracapsular injuries in displaced transverse acetabular fractures and to treat injuries accordingly. In the case of acetabular fractures, multiple authors have identified reduction as the most important factor for avoiding the development of arthrosis and for obtaining a good clinical outcome, but they have noted that even anatomic fracture reduction fails to guarantee excellent outcomes. It is likely that additional factors such as chondral damage at the time of injury, loose fragments, and labral injuries all contribute to the patient’s final long-term outcome (Figures 24-3 and 24-4).