Fig. 34.1
Anteroposterior (a) and lateral (b) radiographs demonstrating radiolucency and rarefaction typical of osteochondritis dissecans of the elbow
MRI has become the standard modality for further evaluation [5, 25]. Not only can MRI assess the articular surface, but it can also define both size and extent of the lesion (Fig. 34.2). Early, stable lesions show changes on T1-weighted images, but T2-weighted images may remain normal. On the other hand, advanced lesions show changes on both T1 and T2-weighted images [5, 26]. Loose in situ lesions may demonstrate a cyst under the lesion. MR arthrography can provide further information as to the extent of the injury [25, 26]. Contrast can show separation of a detached or partially detached piece from subchondral bone. Progressive healing can also be followed via plain radiographs or MRI. If the fragment remains stable, the central sclerotic fragment gradually becomes less distinct and the surrounding area of radiolucency slowly ossifies [5, 9].
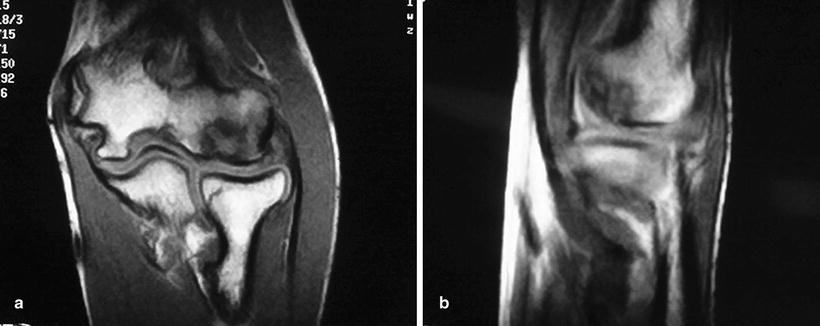
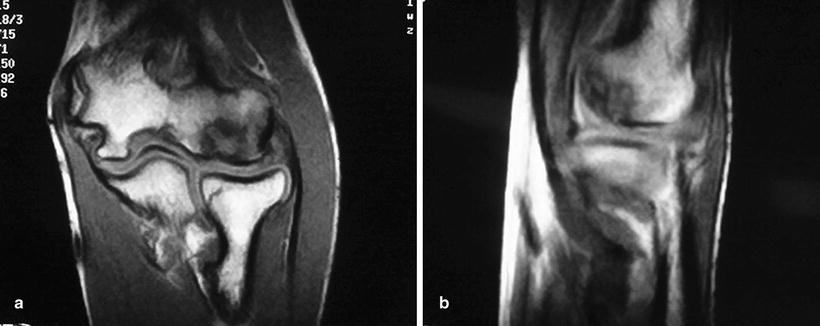
Fig. 34.2
Coronal (a) and sagittal (b) MR images of the same lesion shown in Fig. 34.1. Increased signal of the T2 image indicates disruption of the articular surface
Treatment Options
Options for the surgical management of symptomatic OCD include nonoperative measures, fragment excision, fragment fixation, and osteochondral autograft reconstruction of the lesion. Management decisions are based primarily on the integrity of the articular cartilage and status of the involved segment; whether it is stable, unstable but attached, or detached and loose. The size and location of the lesion as well as the status of the capitellar physis also affect decision making [21, 27, 28].
Stable lesions with intact cartilage and in situ subchondral fragments are managed conservatively [5, 18, 25]. Surgical indications include persistent or worsening symptoms despite prolonged conservative care, loose bodies, or evidence of instability including violation of intact cartilage or detachment [5, 18, 29, 30].
Conservative Management
Recently, some literature suggests that radiographic information alone is not sufficient to determine if a lesion can be successfully treated nonoperatively. Specifically, Takahara et al. [28, 31] retrospectively reviewed 106 cases of capitellar OCD with an average 7 year follow-up in a level II study. They found that lesions that healed completely with nonoperative treatment had the following characteristics on initial presentation: open capitellar physis, good elbow motion, and radiographic findings of localized flattening or lucency of the subchondral bone. Lesions that fit that criteria were classified as stable.
Nonsurgical treatment is typically selected for patients with intact, nondisplaced, stable lesions, and it involves activity modification with cessation of sports participation [28, 32, 33]. Sports and other aggravating activities are avoided until symptoms subside, approximately for 3–6 weeks. We recommend protecting the elbow in a hinged elbow brace during that time. The straight hinges function to off load the capitellum by correcting the normal valgus tilt of the elbow. As symptoms decrease, physical therapy can begin. Gentle range of motion exercises followed by strengthening are instituted as symptoms dictate. The athlete can usually return to unrestricted sports activities within 3–6 months after treatment has begun [19]. Patients with intact lesions caught early and treated conservatively have the best prognosis. However, it is prudent for the clinician to inform the patient and family of possible long-term sequelae [9, 10, 14, 16, 18, 23, 25].
Surgical Treatment
Operative intervention is indicated for patients that do not improve with appropriate nonoperative treatment have, the presence of loose bodies with mechanical symptoms, or an unstable lesion [7, 13]. Takahara et al. [28, 31] found that conservative treatment failed when patients with unstable lesions had one of the following findings at presentation: a closed capitellum physis, fragmentation, or restriction of elbow motion greater than 20°.
Multiple operative procedures have been described for treating these lesions including drilling of the defect [13], fragment removal with or without curettage/drilling of the residual defect [9, 10, 13, 16, 23, 34, 35], fragment fixation by a variety of methods [13, 36–39], reconstruction with osteochondral autograft [13, 38, 40–43], autologous chondrocyte implantation [13, 44], and closing-wedge osteotomy of the lateral condyle [13, 45]. Comparisons of the results of the various operative techniques, however, are difficult because of their largely retrospective nature, different outcome measures, and the relative infrequency of osteochondritis dissecans [13].
Arthroscopic surgery is becoming the standard procedure for the surgical treatment of capitellar osteochondritis dissecans [46, 47]. Advantages include the minimally invasive nature of the procedure with the potential for early rehabilitation, access to the lesion and the entire elbow joint, and ability to identify and treat concurrent lesions including the removal of loose bodies [13]. Studies on arthroscopic debridement and abrasion arthroplasty have shown encouraging short- and mid-term results [9, 21, 22, 28, 35, 47–50]. Recently a level III review of the literature by de Graff et al. [51] suggested that both good short term and long term results can be achieved in a majority of patients treated arthroscopically for OCD of the capitellum. However, their review also emphasized the need for enhanced methodology and longer follow-up. Studies Miyake et al. [52] recently retrospectively evaluated 106 patients who underwent arthroscopic debridement of a capitellar OCD lesion. They found patients with large lesions and open proximal radial physes had both poor radiographic and clinic outcomes. Excellent short term results were obtained in the remaining patient groups.
To treat OCD lesions arthroscopically, the angle of approach through portal access is of utmost importance in order to thoroughly debride, drill, or place osteochondral plugs. Most surgeons use a variation of a 6-portal approach [13, 21, 46, 53] (Fig. 34.3). These portals include standard anteromedial, anterolateral, direct posterior, posterolateral, and direct lateral portals [13, 53]. Baumgarten et al. [21] identified the use of 2 direct lateral portals as the key to effective arthroscopic treatment of osteochondritis dissecans of the capitellum. Davis et al. [53] performed a cadaveric study evaluating the dual direct lateral portals and found that 78 % of the entire capitellar surface area was accessible through these portals. In addition, the portals remain safely proximal and posterior to the lateral ligamentous complex [53]. A distal ulnar portal (Fig. 34.4) has recently been described and is placed approximately 3–4 cm distal to the posterior aspect of the radiocapitellar joint and just lateral to the palpable posterior edge of the ulna [47]. This portal is typically used as a viewing portal, while the standard soft-spot portal is used as a working portal [47]. Some authors have described an arthroscopic-assisted drilling method, using a hole drilled through the radius shaft [54]. In this novel approach to drilling of an OCD lesion, a 1.8 mm K-wire is drilled into the radial head from approximately 3 cm distal. The OCD lesion can usually be completely accessed by altering the flexion angle in both pronation and supination [54]. The angle of approach, however, can be in close proximity to the posterior interosseous nerve. Also, this procedure requires drilling across the normal cartilage surface of the radius [47, 54].

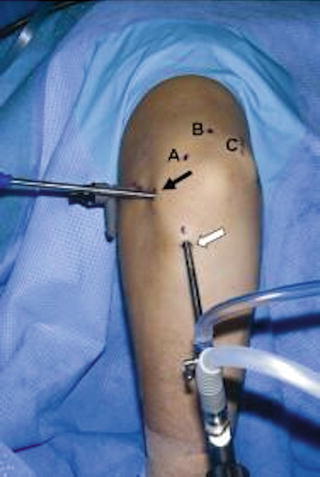

Fig. 34.3
Common arthroscopic elbow portals
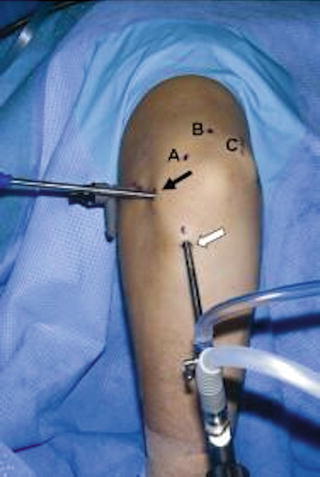
Fig. 34.4
The distal ulnar portal approximately 3–4 cm distal to radiocapitellar joint and just lateral to the palpable posterior edge of the ulna
The surgical treatment of unstable lesions depends on the size and location of the lesion. Smaller lesions can be debrided with good pain relief. There is still debate over treatment of larger lesions with debridement versus repair versus osteochondral autografts. Shimada et al. [55] suggested that lesions less than 1 cm2 could be treated with debridement, chondroplasty, and possibly microfracture or drilling, and lesions greater than 1 cm2 should be treated with osteochondral autograft or fixation. Takahara et al. [9, 28] found lesions with defects greater than 50 % of the capitellar width had a poorer prognosis after fragment removal alone.
Poor results after treatment have been noted in lesions that extend through the lateral margin of the capitellum resulting in the absence of a complete circumferential border of healthy articular cartilage and subchondral bone [13, 22, 34] (Fig. 34.5). Byrd and Jones [34] postulated that the lateral fragment noted in the study by Ruch et al. [22] is similarly associated with loss of the lateral border of the capitellum and portends a possible poor prognosis [13]. The lateral column of the capitellum supports compressive forces when the elbow undergoes either a valgus stress or an axial load. The lack of a lateral buttress impedes the formation of fibrocartilage by subjecting the defect to increased radiocapitellar forces. In a similar fashion, engagement of the radial head into the defect compromises healing. This situation may also lead to accelerated radiocapitellar arthrosis. ElAttrache and Ahmad et al. [56] stated that more than 6–7 mm of lateral column involvement may not be best treated by microfracture alone. They did report successfully treating lesions that were an average of 1.32 cm2 with microfracture alone provided there was no lateral column involvement. Interestingly, this is in contrast to the suggestion by Shimada et al. [55] that lesions >1 cm2 should be treated with osteochondral autograft or fixation. Perhaps, this is demonstrates that, to an extent, involvement of the lateral column may more important than the absolute size of the lesion when choosing treatment methods.
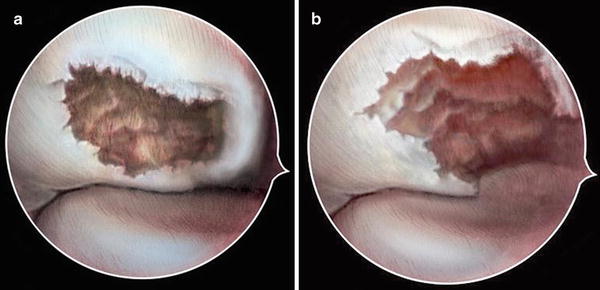
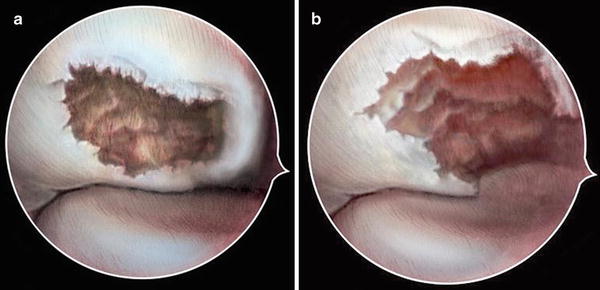
Fig. 34.5
View of osteochondritis dissecans lesion of capitellum in right elbow of patient in prone position viewing from posterolateral portal. Contained osteochondritis dissecans lesion (a) with circumferential healthy cartilage present. Similar lesion with loss of lateral column support (b)
Osteochondral autograft transplantation has been recently introduced as another treatment option for capitellum osteochondritis dissecans [13, 38, 40–43]. Indications for this procedure have included lesions involving over 50 % of the articular surface area, disruption of the lateral buttress (Fig. 34.5), and engagement of the radial head [28, 33, 57]. Cylindrical osteochondral grafts are harvested from a donor site, typically the lateral femoral condyle. The plug is inserted perpendicular to the subchondral bone (Fig. 34.6) [31, 40]. These authors have suggested that the procedure may reduce the progression to osteoarthritis and lead to better long-term results [47]. Several reports have described success with osteochondral autograft transfer and osteochondral mosaicplasty [13, 41, 43, 55, 58–61] (Table 34.1).
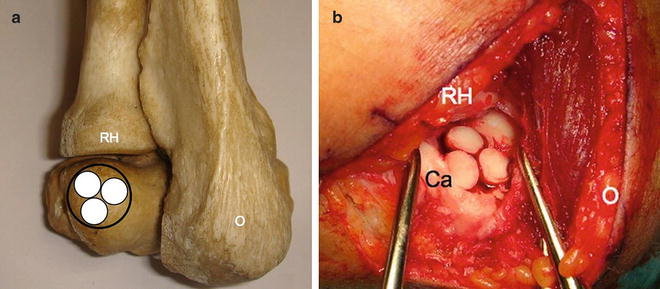
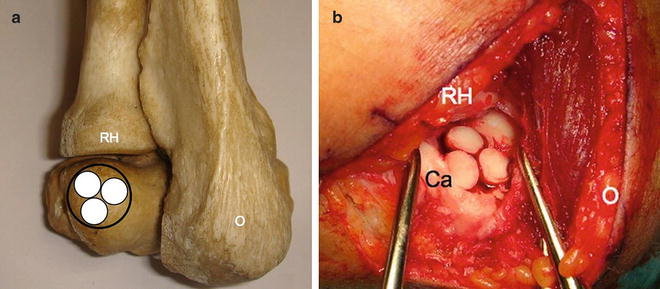
Fig. 34.6
Osteochondral autograft reconstruction of osteochondritis dissecans lesion of the capitellum: Schematic drawing (a) and intraoperative view (b)
Table 34.1
Results of osteochondral autograft transfer and mosaicplasty for OCD of the capitellum
Author | Mean follow-up | Mean score (points) | Number of patients | Pain free at final follow-up | Patients return to sport level |
|---|---|---|---|---|---|
Tsuda et al. [58] 2005 | 16 months | 193 (Timmerman, 200 max) | 3 | 3 | 3 |
Shimada et al. [55] 2005 | 25.5 months | 93.8 (Japanese Orthopaedic Association, 100 max) | 10 | 8 | 8 |
Yamamoto et al. [43] 2006 | 3.5 years | – | 18 | – | 14 |
Iswasaki et al. [59] 2006 | 24 months | 183 (Timmerman, 200 max) | 8 | 7 | 6 |
Iswasaki et al. [41] 2009 | 45 months | 191 (Timmerman, 200 max) | 19 | 18 | 17 |
Ovesen et al. [60] 2011 | 30 months | 93.5 (mayo, max 100) | 10 | 8 | 10 |
92.5 (constant, max 100) | |||||
Shimada et al. [61] 2012 | 36 months | 180 (Timmerman, 200 max) | 26
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





