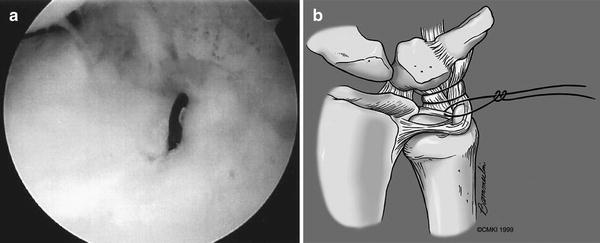
Fig. 12.1
A lunotriquetral ligament tear as seen from the 6-R portal
1.
Congruency
(a)
The lunate and triquetrum should be colinear. If the view of the lunotriquetral joint from the midcarpal radial portal is blocked by a separate lunate facet [25], place the arthroscope in the midcarpal ulnar portal to gain visualization. Under these conditions, the radial articular edge of triquetrum should be aligned with the most ulnar articular edge of the hamate facet of the lunate (Figs. 12.2a, b).
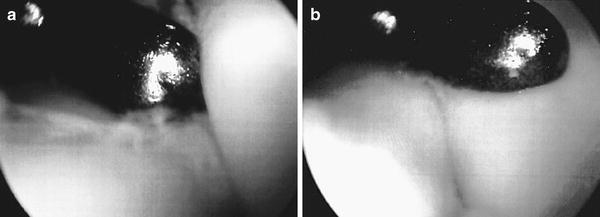
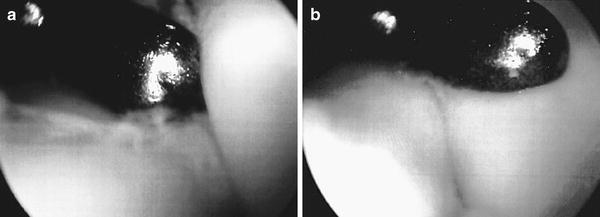
Fig. 12.2
(a) An incongruent LT joint as seen from the ulnar midcarpal portal. The probe has been inserted from the radial midcarpal portal. The triquetrum is to the right and the lunate is to the left. (b) The triquetrum has been reduced and stabilized with K-wires and now is congruent with the lunate (left)
(b)
Although congruent, the LT joint may be unstable due excessive laxity.
2.
Laxity
(a)
Assuming normal, the scapholunate joint can be used as a reference. Laxity should be assessed both upon triquetral rotation and separation from the lunate.
(b)
Upon midcarpal arthroscopic assessment of an unstable LT joint, the dorsal portion of the triquetrum is often rotated such that its articular surface is distal to the lunate (Fig. 12.3). The triquetrum can be translated to a reduced state in which the articular surfaces of the triquetrum and lunate are collinear.
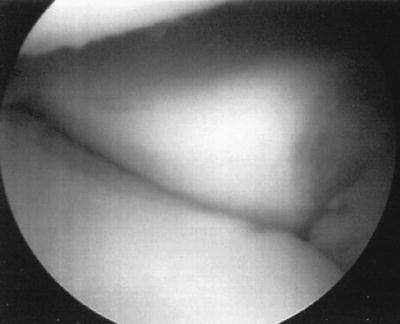
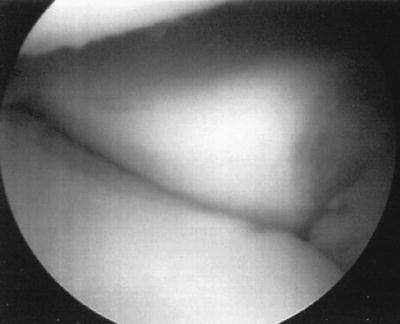
Fig. 12.3
As seen from the radial midcarpal portal, the dorsal portion of the triquetrum is rotated distally with respect to the dorsal portion of the lunate
(c)
An unstable LT joint may have colinear articular surfaces however, the triquetrum can be ulnarly translated so as to “gap open” the LT joint. The normal SL joint can be used as a reference.
The final midcarpal assessment of the LT joint is the dorsal capsular structures. The dorsal radiocarpal and dorsal intercarpal ligaments attach to the lunate and triquetrum in part. In certain cases, avulsions of the dorsal capsuloligamentous structures have been observed (Fig. 12.4).
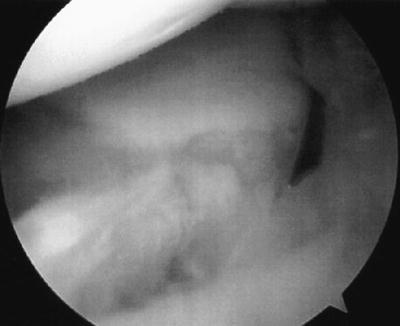
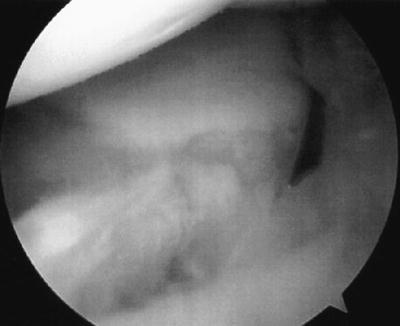
Fig. 12.4
Viewing from the radial midcarpal portal, the dorsal capsuloligamentous structures have been avulsed from their bony attachment
The arthroscope is placed in the 3-4 portal during disc-lunate to ulno-capitate to disc-triquetral ligament plication. The volar 6-U (v6-U) is established. The v6-U portal is similar to the normal 6-U portal; however, it is placed just dorsal to the disc-carpal ligaments (Fig. 12.5). Care is taken to avoid injury to the dorsal sensory branches of the ulnar nerve during placement.
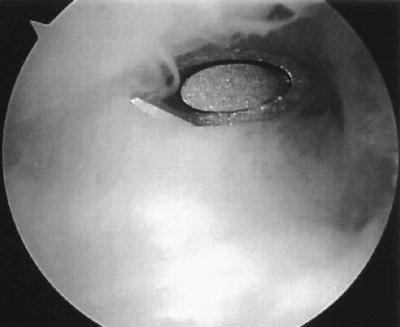
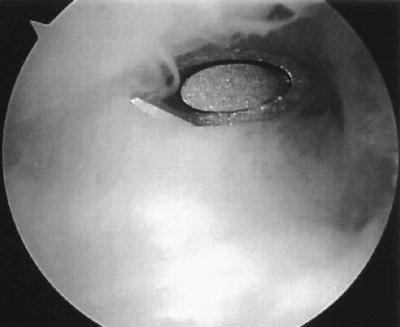
Fig. 12.5
The spinal needle has entered the radiocarpal joint at the level of the ulnar carpal ligaments. Some fraying of the disc-carpal ligaments is seen and is associated with LT ligament injury
The interval between the disc-lunate and disc-triquetral ligament identifies the lunotriquetral joint and interosseous ligament. Debridement of the lunotriquetral ligament, disc-carpal ligaments, and additional pathology is performed. Through the v6-U portal, an 18 G spinal needle is passed just volar to the disc-triquetral, ulno-capitate, and disc-lunate entering the radiocarpal joint at the radial edge of the UL ligament just distal to the articular surface of the radius. A #2-0 PDS suture is placed through the needle into the joint. The suture is retrieved either sequentially through the 6-R and the through the v6-U or directly through the v6-U using a wire loop suture retriever and then and tagged as the first plicating suture (Fig. 12.6a–c). In likewise fashion, a second plicating suture is placed approximately 5 mm distal to the first so that the suture loops are parallel to the lunate and triquetrum and is tagged as the second plicating suture (Fig. 12.7a–c). Tension on the first stitch often facilitates a second needle passage through the ulnolunate and ulnotriquetral ligaments. Adequacy of the plication (tension the stitch) and its effect on LT interval stability should be assessed after each suture passage.
Fig. 12.6
(a) The spinal needle has traversed from ulnar to radial just palmar to the ulnar carpal ligaments. The tip of the needle has reentered the radiocarpal joint radial to the disc-carpal ligament. In the photo, the lunate is above and the ulnar border of the distal radius (lunate fossa) is seen obliquely at the level of the spinal needle. (b) A 2-0 PDS suture has been passed through the spinal needle and retrieved out the v6-U portal. The disc-carpal ligaments are visualized with the lunate above. (c) The suture passage is diagrammatically represented. The disc-triquetral ligament is to the right. The first 2-0 PDS plication suture is passed from ulnar to radial with a spinal needle through the volar 6-U portal. The disc-triquetral, ulno-capitate, and disc-lunate ligaments are incorporated in the suture [c: With permission from The Christine M. Kleinert Institute for Hand and Microsurgery, Inc.]
Fig. 12.7
(a) The disc-triquetral ligament is to the left. The first plicating suture is seen below and to the right (ulnar) exiting the ulnarly through the v6-U portal. The spinal needle is seen distal (above), as it is ready to be passed for the second plicating suture. (b) The second 2-0 PDS plication suture. Tension on the first suture facilitates placement of the second suture, which is placed approximately 5 mm distal to the first suture. (c) The plication sutures are represented diagrammatically [c: With permission from The Christine M. Kleinert Institute for Hand and Microsurgery, Inc.]
Finally, through the v6-U portal, a spinal needle is passed through the volar aspect of the capsule at the pre-styloid recess and then through the peripheral rim of the TFCC. The wire retriever is introduced through the ulnar capsule and the suture is brought out the v6-U portal to tighten the ulnar capsule (Fig. 12.8a, b). The three sets of sutures are tied at the termination of the procedure after the lunotriquetral joint has been congruently reduced and stabilized with K-wires.