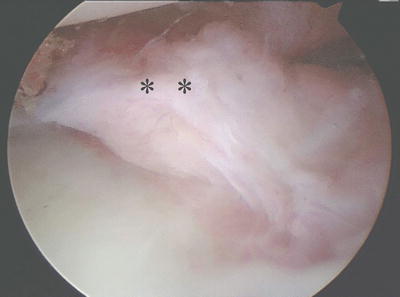
Fig. 13.1
Normal DRCL (asterisk) as seen from the VR portal. L lunate, R radius
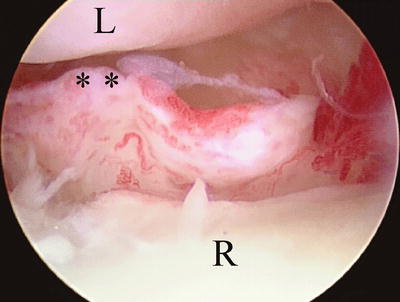
Fig. 13.3
Chronic DRCL tear with rounded edges (asterisk). L lunate, R radius
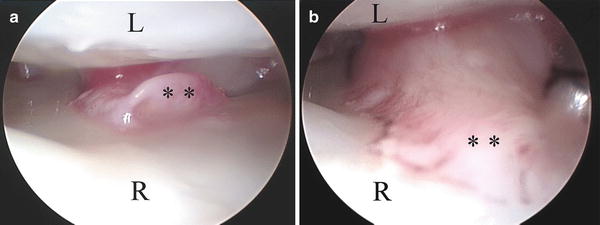
Fig. 13.4
(a) Under dry arthroscopy the DRCL tear appears small and unimpressive (asterisk). L lunate, R radius. (b) A hook probe is used to pull the DRCL tear (asterisk) into the joint, demonstrating the large amount of tissue that can impinge between the radius and lunate
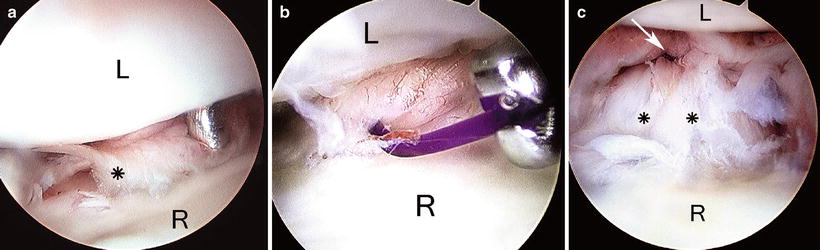
Fig. 13.5
(a) Arthroscopic view of DRCL tear (asterisk) from the VR portal. L lunate, R radius. (b) A 2-0 suture has been inserted through a spinal needle in the 4,5 portal and is being retrieved with forceps in the 3,4 portal. (c) Completed repair. Note how the DRCL tear (asterisk) has been plicated up against the dorsal capsule (arrow)

Fig. 13.6
(a) a 22G spinal has been inserted through the midsubstance of the DRCL tear. (b) A 2-0 suture has been inserted through the spinal needle and is being retrieved with forceps in the 3,4 portal. (c) Completed repair (arrow)
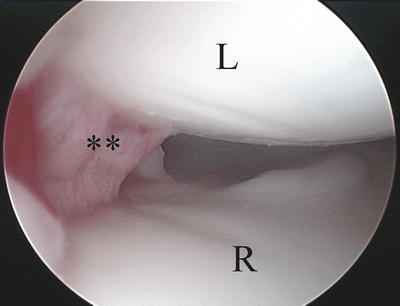
Fig. 13.7
Oblique view of a DRCL tear from the 6R portal
Following the repair the patient is placed in a below elbow splint with the wrist in neutral rotation. Finger motion and edema control are instituted immediately. At the first postoperative visit the sutures are removed and the patient is placed in a below-elbow cast for a total of 4 weeks, followed by wrist mobilization.
Outcomes
A retrospective chart review of 21 patients who underwent a DRCL repair was published in 2005 [14, 15]. None of the wrists showed a static carpal instability pattern on X-ray. A preoperative MRI was performed by the referring physician in six patients. Preoperative arthrograms were performed as a part of the diagnostic work up for wrist pain in 20 patients. None of the DRCL tears in this series were identified with preoperative arthrography or MRI. A preoperative MRI in one patient with a DRCL tear was misinterpreted as representing a dorsal wrist ganglion. There were 6 men and 16 women. The average patient age was 40 years (range, 25–62 years). All patients failed a trial of conservative treatment with wrist immobilization, cortisone injections, and work restrictions. The average length of conservative treatment was 7 months. The time interval between injury and surgical intervention averaged 25 months (range, 8–53 months).
At the time of arthroscopy, five patients were found to have an isolated DRCL tear that was solely responsible for their wrist pain. The remaining patients had additional ligamentous pathology. A dorsal capsulodesis was performed in seven patients as the primary treatment for the SLIL instability/tear. Thirteen patients underwent an arthroscopic DRCL ligament repair ± thermal shrinkage (repair = 5, repair + shrinkage = 6, shrinkage = 2). Ten of these patients underwent ancillary procedures for treatment of the coexisting wrist pathology. Lunotriquetral ligament tears were treated with debridement ± pinning. Triangular fibrocartilage tears were debrided or repaired. Scapholunate ligament tears/instability were treated with capsulodesis ± open repair. One patient had generalized arthrofibrosis which precluded a DRCL repair. Concomitant nerve entrapment was a common finding which was treated at the same time.
The average duration of the follow-up period was 16 months (range, 7–41 months), with one patient lost to follow-up at 4 weeks. Pain was graded as none, mild, moderate, and severe. Wrist extension, wrist flexion, radial deviation, ulnar deviation, and grip strength were assessed. Wrist range of motion was compared with presurgical values. Grip strength was compared with the contralateral side at follow-up evaluation.
The five patients who underwent an isolated DRCL repair were satisfied with the outcome of surgery and would repeat the surgery again because it improved their symptoms. All five patients graded their pain as none or mild. None of these patients were taking pain medications. All returned to their previous occupations without restriction. Their wrist motion was unchanged as compared to the preoperative status. Grip strengths were 90–130 % of the opposite side.
The patients with coexisting pathology had variable outcomes that were largely influenced by the treatment of the associate pathology. It was not possible to separate out the effect of the DRCL repair. At the latest review, 64 patients had undergone arthroscopy for the investigation and treatment of refractory wrist pain. Thirty-five patients were found to have DRCL tears, for an overall incidence of 55 %. As such it is prudent that the arthroscopist is diligent in recognizing and treating this condition. Ongoing research into the ideal method of treatment of these combined injuries however is still needed.
Arthroscopic Wrist Ganglionectomy
Osterman et al. pioneered the arthroscopic resection of dorsal wrist ganglia and reported on 150 procedures with only one recurrence [16]. Volar wrist ganglia that originate from the radiocarpal joint are amenable to arthroscopic resection, but those that arise from the scaphotrapezialtrapezoidal joint are not.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree