Arthroscopic Approaches to Synovial Pathology
Keith Monchik
Paul Fadale
The synovial membrane of the knee is the largest and most extensive in the body. The synovium of the knee is the deepest layer of the joint capsule and frequently has several embryologic invaginations, called plica. The synovium starts at the superior pole of the patella, where it forms a large pocket beneath the quadriceps femoris. On both the medial and the lateral sides of the knee, the synovium lies on the inner surface of the capsule, except at the attachments of the meniscus to the capsule itself. On the lateral side, it is separated from the capsule by the popliteus. Anteriorly, the synovium covers the deep surface of the patella tendon, as well as attaching to the articular margins of the patella. Below the patella it lines the deep surface of the infrapatella fat pad, and a horizontal ala fold can be identified on each side of the fat pad; below, these folds converge and are continued as a single band, the patella fold (ligamentum mucosum). On either side of the patella, the synovial membrane extends beneath the aponeuroses of the vasti, and more beneath the Vastus medialis. The synovium continues along the capsule distally from the femur to the tibia. It is reflected anterior to the cruciate ligaments, which are therefore considered outside the synovial cavity. Both benign and malignant processes can involve the synovial membrane. For most conditions that require surgical treatment, arthroscopic synovectomy is a safe and effective method.
BENIGN CONDITONS
Plica Syndrome
The medial plica, normally found in approximately 70% of patients, may become hypersensitive with direct trauma to a flexed knee. The medial plica is also prone to injury due to overuse. The lateral fold is rarely symptomatic (1). Clinical presentation is similar to that of medial meniscal tears and patella tendonitis as well as other conditions of the knee. There may also be a snapping sensation along the medial aspect of the flexed knee. Therefore, one should exclude other more common pathologies before making a diagnosis of plica syndrome. In 2007, demonstrated that MRI is of limited value in detecting normal or pathologic plicae in the knee. Arthroscopic resection is considered after a failed course of anti-inflammatories, steroids, and physical therapy. Arthroscopic evaluation usually reveals an inflamed or hypertrophied medial plica. Postoperative physical therapy begins immediately, and the outcome of resection in well-selected patients is very good, approaching a success rate of higher than 80% in one study.
Pigmented Villonodular Synovitis
Pigmented villonodular synovitis (PVNS) is a slow growing, benign, locally invasive tumor characterized by the presence of inflammation and hemosiderin deposits within the synovium. It is typically a monoarticular process, most often affecting the knee joint with an incidence of 1.8 per million population. PVNS is subdivided into two entities: Diffuse PVNS (DPVNS) and localized PVNS (LPVNS). In the knee, the diffuse form is more common than the localized disease. The lobular, pedunculated LPVNS lesions most frequently present in the anterior compartment of the knee, with most arising at the meniscocapsular junction. As the synovium in the area of the anterior horn is most often affected, patients commonly present with clinical symptoms similar to meniscal pathology. However, other areas of the knee including the suprapatella fat pad, intercondylar notch, suprapatella pouch, both the medial and the lateral recesses, and the anterior horn of the lateral meniscus have been reported. Due to its localized nature, symptoms most commonly include pain, locking, catching, and instability (2). In addition, this is usually, but not always, accompanied by swelling and pain.
In contrast, DPVNS has an insidious, slow onset of pain with swelling and stiffness. In less than 30% of patients, plain radiographs may show nonspecific findings of soft tissue swelling or signs of joint effusion, which are not specific enough to establish the correct diagnosis. While synovial fluid aspiration may reveal a brownish-stained bloody fluid, this may indicate any one
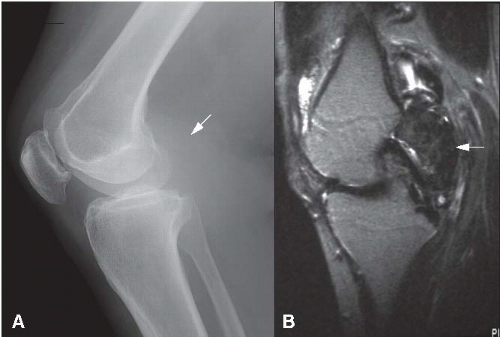
of a variety of knee pathologies and is not sensitive or specific to PVNS. CT examination may demonstrate a soft tissue mass of high density relative to skeletal muscle and in long standing cases, bone erosions and subchondral cysts. MRI is the most useful diagnostic tool. The iron in hemosiderin shortens T2 relaxation times on spin echo sequences and causes susceptibility effects on T2* gradient echo sequences resulting in low signal intensity on both types of images, but more so on the gradient echo images, which are more sensitive the presence of hemosiderin (Fig. 82.1). High signal intensity regions may be present on T1 images (fat deposition or hemorrhage) or T2 images (joint effusions or synovial inflammation). MRI is also useful in gauging the extent of the lesion, especially in areas less easily accessible with an arthroscope. Surgery is the definitive treatment for both the localized and the diffuse forms of the disease. Corticosteroids may provide temporary pain relief. In most series, recurrence following excision of LPVNS is rare. Recurrence after total synovectomy of DPVS can be as low as 9% (3). There have been rare reports of malignant transformation and metastasis in patients diagnosed with PVNS (4). In this series, the mortality rate was 50%. Arthroscopic synovectomy lends itself particularly well to the treatment of PVNS, especially the localized form. Arthroscopy has been associated with better functional results and lower rates of postoperative stiffness; however, improper use of this technique has may result in unacceptable recurrence rates. Arthroscopy allows for excellent visualization of lesions, especially in some areas not easily accessible through open treatment such as the posterior compartment. Complete synovectomy in DPVNS results in a substantially lower rate of recurrence than partial excision, but is technically very challenging. Because the posterior compartment is almost always involved in the diffuse form, the surgeon must be comfortable working with both the posteromedial (PM) and the posterolateral portals. Arthroscopic treatment carries a risk of incomplete resection in the diffuse form, as well as the theoretical risk of portal/joint seeding. However, when compared with open synovectomy, arthroscopy is associated with a shorter hospital stay and a shorter rehabilitation period. In a study by Flandry et al., rates of postoperative stiffness following open synovectomy were as high as 24% with the need for further manipulation. The combination of arthroscopic treatment with open synovectomy has not been well described, and thus its effectiveness remains unclear. Poor prognosis has been reported (both open and arthroscopically treated) with invasion of subchondral bone. Radiation therapy has been used as an alternative to surgical treatment, but the results of radiation synovectomy have been mixed.
of a variety of knee pathologies and is not sensitive or specific to PVNS. CT examination may demonstrate a soft tissue mass of high density relative to skeletal muscle and in long standing cases, bone erosions and subchondral cysts. MRI is the most useful diagnostic tool. The iron in hemosiderin shortens T2 relaxation times on spin echo sequences and causes susceptibility effects on T2* gradient echo sequences resulting in low signal intensity on both types of images, but more so on the gradient echo images, which are more sensitive the presence of hemosiderin (Fig. 82.1). High signal intensity regions may be present on T1 images (fat deposition or hemorrhage) or T2 images (joint effusions or synovial inflammation). MRI is also useful in gauging the extent of the lesion, especially in areas less easily accessible with an arthroscope. Surgery is the definitive treatment for both the localized and the diffuse forms of the disease. Corticosteroids may provide temporary pain relief. In most series, recurrence following excision of LPVNS is rare. Recurrence after total synovectomy of DPVS can be as low as 9% (3). There have been rare reports of malignant transformation and metastasis in patients diagnosed with PVNS (4). In this series, the mortality rate was 50%. Arthroscopic synovectomy lends itself particularly well to the treatment of PVNS, especially the localized form. Arthroscopy has been associated with better functional results and lower rates of postoperative stiffness; however, improper use of this technique has may result in unacceptable recurrence rates. Arthroscopy allows for excellent visualization of lesions, especially in some areas not easily accessible through open treatment such as the posterior compartment. Complete synovectomy in DPVNS results in a substantially lower rate of recurrence than partial excision, but is technically very challenging. Because the posterior compartment is almost always involved in the diffuse form, the surgeon must be comfortable working with both the posteromedial (PM) and the posterolateral portals. Arthroscopic treatment carries a risk of incomplete resection in the diffuse form, as well as the theoretical risk of portal/joint seeding. However, when compared with open synovectomy, arthroscopy is associated with a shorter hospital stay and a shorter rehabilitation period. In a study by Flandry et al., rates of postoperative stiffness following open synovectomy were as high as 24% with the need for further manipulation. The combination of arthroscopic treatment with open synovectomy has not been well described, and thus its effectiveness remains unclear. Poor prognosis has been reported (both open and arthroscopically treated) with invasion of subchondral bone. Radiation therapy has been used as an alternative to surgical treatment, but the results of radiation synovectomy have been mixed.
Chondromatosis/Osteochondromatosis
Synovial chondromatosis is a benign and rare metaplasia of the synovial membrane resulting in the formation of multiple intra-articular cartilaginous or osteocartilagenous bodies. This is most often a monoarticular condition occurring most commonly in middle-age men with over half the cases presenting in the knee. Synovial chondromatosis occurs as either a primary or a secondary form. In primary synovial chondromatosis occurs without an identifiable joint pathology, whereas the secondary form is present in the setting of preexistent disease (osteoarthritis, rheumatoid arthritis [RA], osteochondritis dissecans, etc.). Typically, patients present with pain and swelling, with or without mechanical symptoms. In the absence of calcification, plain radiographs will not reveal
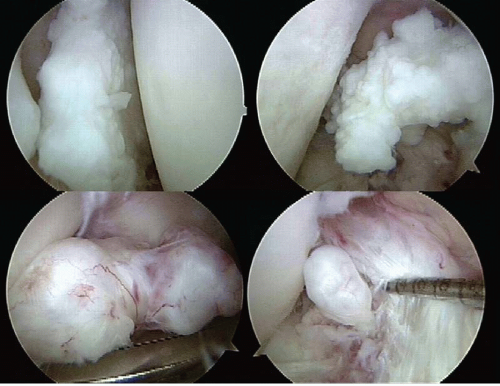
loose bodies. CT examination is useful for identifying calcified loose bodies only. MRI is useful depending on the amount of synovial proliferation and amount of calcification within the nodules. Cartilaginous nodules have intermediate signal intensity on T1-weighted images, and high signal intensity on T2-weighted images. Intra-articular gadolinium contrast increases the sensitivity for detecting lesions. Patients with recurrent painful effusions or mechanical symptoms are candidates for surgical treatment (Fig. 82.2). Arthroscopic loose body removal and synovectomy are a safe and effective treatment for this disease (5). Recurrence rates between arthroscopic and open synovectomy are equivalent (0% to 31%), with open treatment having a higher incidence of prolonged rehabilitation and decreased range of motion. Postoperatively, the prognosis is generally good with low rates of recurrence and malignant transformation. Osteoarthritis remains a significant long-term complication, sometimes requiring joint arthroplasty.
loose bodies. CT examination is useful for identifying calcified loose bodies only. MRI is useful depending on the amount of synovial proliferation and amount of calcification within the nodules. Cartilaginous nodules have intermediate signal intensity on T1-weighted images, and high signal intensity on T2-weighted images. Intra-articular gadolinium contrast increases the sensitivity for detecting lesions. Patients with recurrent painful effusions or mechanical symptoms are candidates for surgical treatment (Fig. 82.2). Arthroscopic loose body removal and synovectomy are a safe and effective treatment for this disease (5). Recurrence rates between arthroscopic and open synovectomy are equivalent (0% to 31%), with open treatment having a higher incidence of prolonged rehabilitation and decreased range of motion. Postoperatively, the prognosis is generally good with low rates of recurrence and malignant transformation. Osteoarthritis remains a significant long-term complication, sometimes requiring joint arthroplasty.
Lipoma Arborescens
Lipoma arborescens is a rare intra-articular lesion, characterized by diffuse replacement of the subsynovial tissue by mature fat cells, producing prominent villous transformation of the synovium (6). This condition is sometimes referred to as villous lipomatous proliferation of the synovial membrane. Macroscopically, it is a bulky mass of tissue with a frond-like appearance of numerous broad-based villi composed of fatty yellow tissue. Lipoma arborescens is typically located in the suprapatella pouch, affects males and females equally in the fifth through seventh decade, and is uncommon with less than 100 reported cases. A rare case of an affected pediatric patient has been reported (7). Patients typically present with a joint effusion, enlarged suprapatella pouch, decreased range of motion, stiffness, and occasionally mechanical symptoms. The lesion may arise de novo or develop in patients with degenerative joint disease, RA, or trauma. Plain radiographs may reveal soft tissue swelling in the suprapatella pouch. MRI shows villous lipomatous proliferation with signal intensity similar to that of fat on T1- and T2-weighed images, and a joint effusion. Other findings less commonly seen are a mass-like subsynovial fat deposition, associated synovial cysts, and degenerative changes. Temporary relief of symptoms has been proven with intra-articular injection of steroids or radioisotope (e.g., Y-90). Definitive treatment is complete synovectomy associated with a very low recurrence rate. Successful management by arthroscopic synovectomy has been reported.
Synovial Hemangioma
This is a benign, vascular tumor that occurs mainly in the knee as recurrent painful monoarticular hemarthrosis. It is more frequent in children and young adults and is rare with less than 200 reported cases. Patients usually present in the second decade with pain, limited range of motion,
and stiffness in the absence of trauma. Forty percent of patients may have an associated cutaneous hemangioma. A palpable, spongy, compressible mass may be present. Hemangiomas of the knee are described as synovial, juxta-articular or intermediate, where both synovial and juxta-articular component. The intermediate form is often diffuse and unresectable. Radiographs may reveal soft tissue masses, calcified phleboliths, and a hemophilia-like arthropathy with epiphyseal enlargement. MRI findings are more specific consisting of a lobulated intra-articular mass. The mass has an intermediate signal intensity on T1-weighted images. T2 images show area of hypersensitivity (pooling of blood within vascular spaces) and low signal intensity areas (fibrous septa or vascular channels). More importantly, MRI localizes the area and extent of the lesion, which aids in preoperative planning (8). Surgical excision is the definitive treatment. Preoperatively, embolization of the lesion may be useful in decreasing bleeding. Use of a coagulation/ablater during much of the resection will aid in reduced surgical bleeding (9), but no studies exist as to whether resection with a standard rotary shaver versus coagulation has improved outcomes. For localized lesions, partial arthroscopic synovectomy is effective. For diffuse lesions, a complete synovectomy is required.
and stiffness in the absence of trauma. Forty percent of patients may have an associated cutaneous hemangioma. A palpable, spongy, compressible mass may be present. Hemangiomas of the knee are described as synovial, juxta-articular or intermediate, where both synovial and juxta-articular component. The intermediate form is often diffuse and unresectable. Radiographs may reveal soft tissue masses, calcified phleboliths, and a hemophilia-like arthropathy with epiphyseal enlargement. MRI findings are more specific consisting of a lobulated intra-articular mass. The mass has an intermediate signal intensity on T1-weighted images. T2 images show area of hypersensitivity (pooling of blood within vascular spaces) and low signal intensity areas (fibrous septa or vascular channels). More importantly, MRI localizes the area and extent of the lesion, which aids in preoperative planning (8). Surgical excision is the definitive treatment. Preoperatively, embolization of the lesion may be useful in decreasing bleeding. Use of a coagulation/ablater during much of the resection will aid in reduced surgical bleeding (9), but no studies exist as to whether resection with a standard rotary shaver versus coagulation has improved outcomes. For localized lesions, partial arthroscopic synovectomy is effective. For diffuse lesions, a complete synovectomy is required.
Popliteal (Baker’s) Cyst
Lindgren described a continuous unidirectional flow between the capsular fold on the PM capsule and the gastrocnemius-semimembranosus bursa (GSB) as a result of a valvular mechanism (10), which gives rise to repeated bursal effusions or “Baker’s cyst.” The predominance of popliteal cysts are treated conservatively. Some are amenable to drainage under ultrasound guidance. However, due to a significant association of intra-articular pathology with recurrent cysts, concurrent treatment of the cyst is warranted at initial arthroscopy as recurrence rates seem to be high after simple open resection (11). Treatment of the cyst involves the obliteration of the slit-like valve, which acts as the gateway between the knee joint and the bursa. Described methods of treatment include an arthroscopic approach through an anteromedial portal (12), cystectomy through a PM cystic portal, and an arthroscopic all-inside suturing of the valvelike structure (13). Regardless of the method chosen, any other associated joint disorder must be addressed in order to minimize the risk of recurrent effusions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree