Arthroscopic Approach to The Throwing Athlete
Milford H. Marchant Jr.
Ronald E. Glousman
The painful shoulder in the overhead-throwing athlete has been a remarkable challenge to orthopedic surgeons and researchers for over 25 years. Several injury mechanisms and multiple factors contributing to shoulder pathology have been recognized over time, yet numerous questions regarding the etiology and optimal treatment strategies are still unanswered.
Similar to other areas of orthopedics, research regarding the painful thrower’s shoulder has undergone an evolution. Early investigations focusing on external impingent of the rotator cuff led to examination of the anterior capsule and the concept of microinstability. As clinical examination and arthroscopic techniques evolved, focus shifted toward the biceps anchor, labral injury secondary to internal impingement, and posterior capsular tightness in painful throwing shoulders. More recently, scapular kinematic alterations have received attention, and now there is more focus on trunk and pelvic stability. Although patient complaints and pathoanatomy present as joint-specific injury patterns, evaluation of the entire athlete is essential to appropriately guide the athlete back to preinjury participation, regardless of the need for surgical intervention. As arthroscopic surgeons, we cannot only aid in discovering and correcting the throwers’ mechanical flaws that led to their injured shoulder, but we can also attempt to repair the pathoanatomic results of misguided biomechanics.
 FIGURE 20.1. Six stages of throwing: (1) windup; (2) early cocking; (3) late cocking; (4) acceleration; (5) deceleration; and (6) follow through. (Reproduced with permission from Thomas WA, Hoenecke HR, Fronek J. Throwing injuries. In: Jonhson DH, Pedowitz RA, eds. Practical Orthopaedic Sports Medicine and Arthroscopy. 1st ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:309-321.) |
THROWING MECHANICS
While athletes in sports such as football, lacrosse, and tennis have injuries secondary to overhead stress, baseball, particularly pitching, serves as the prime example for throwing-related shoulder pathology. Shoulder injuries in baseball start early—the prevalence of shoulder pain has been reported to be as high as 35% in youth and adolescent pitchers.
Pitching is a complex series of motions that places tremendous repetitive stress on the athlete’s shoulder and elbow joints. Energy generated in the lower extremities is amplified and transferred by the pelvis and trunk to the upper extremity where the shoulder acts as a force regulator to the arm, providing the delivery of force.
The pitching motion can be divided into six phases: windup, early cocking, late cocking, acceleration, deceleration, and follow through (Fig. 20.1).
Phase I, or windup, initiates the pitching cycle. The lead foot leaves the ground and the trunk and shoulders coil, storing energy for delivery. The center of gravity remains over the pivot foot. Both hands are in contact with the ball, and the pitching arm is relatively relaxed. The windup phase ends when the ball leaves the gloved hand.
Phase II is the early cocking phase. After the ball leaves the glove, the pitching arm begins to be positioned for delivery. The shoulder is abducted and begins external
rotation, the elbow is high, slightly flexed, and the hand remains on top of the ball. The deltoid and rotator cuff muscles are active. Leading with the pelvis, the center of gravity shifts toward home plate, and the stride begins with the lead foot.
rotation, the elbow is high, slightly flexed, and the hand remains on top of the ball. The deltoid and rotator cuff muscles are active. Leading with the pelvis, the center of gravity shifts toward home plate, and the stride begins with the lead foot.
Phase III is the late cocking phase. The late cocking phase begins with lead foot contact toward home plate. The shoulders start closed, and the linear momentum gained during the stride shifts to rotational momentum during the trunk turn. The arm abducts to just above 90° so that the elbow is slightly above the shoulder, and the shoulder achieves maximum external rotation. The rotator cuff is highly active. It is not uncommon for a pitcher’s shoulder to achieve 120° to 140° of external rotation. Although controversial, the humeral head position is thought to move in a posterior direction. During the same time, the anterior force on the shoulder approaches 400 N. The trapezius and the serratus anterior act as a force couple to stabilize the scapula. Late cocking ends at the point of maximum humeral external rotation.
Phase IV is the acceleration phase. Acceleration begins simply when the ball starts moving toward home plate. The potential energy built up in the lower extremities and trunk is finally transferred to the arm. This portion of the pitching cycle produces unparalleled forces in the shoulder. The force at the glenohumeral joint is estimated to be 860 N. Shoulder internal rotation exceeds 7,000° per second (1). The subscapularis exhibits high activity. Acceleration ends with ball release.
Phase V is the deceleration phase and compromises the first one-third of the time after ball release. Weight transfer from the pivot foot to the lead has finished. The shoulder is still hard at work as the rotator cuff initiates a strong eccentric contraction to slow down the internal rotation. The biceps and brachialis muscles have also been shown to initiate a strong eccentric contraction. Other muscles about the shoulder including the trapezius, serratus anterior, rhomboids, posterior deltoid, latissimus dorsi, and teres minor all activate to slow the shoulder and prevent subluxation.
Phase VI is the final follow-through stage. It compromises the latter two-thirds of the time after ball release. Shoulder adduction is followed by relaxation.
Every pitcher’s delivery is different, and these differences can stress various parts of the shoulder. Regardless of pitching style, there are certain points in the pitching cycle that when executed poorly can cause pain or dysfunction. It is important to recognize that subtle differences in pitching form can translate into subtle differences in the shoulder pathology of injured players.
CLINICAL EVALUATION
History
The clinical evaluation of a thrower with shoulder pain starts with a detailed history. Patient age and the onset of injury are important. It is also essential to know whether the patient had previous injuries or surgical interventions, as these factors can influence decision making.
In young players, particularly those with open physes, it is critical to know their level of competition. Do they pitch? How often do they pitch? Do they rest between outings? When they do not pitch what position are they playing? How many months out of the year do they not play baseball? What pitches are they throwing? Do they pitch in showcases? These questions are often difficult for children or parents to answer, but it is important to distinguish an acute injury from an overuse injury. Physeal injuries and capsular laxity are common in young overhead athletes, and typically, these patients can be treated without surgery.
In older adult players, the acuity of the problem is often difficult to ascertain. The patient may have trouble remembering the exact onset of symptoms, but it is important to know the last time the player participated fully without pain. In some instances, it may be months or years since the onset of symptoms, and this represents a completely different clinical picture than someone with pain for just a few weeks.
Other important questions to ask both young and older age groups include joint-specific and sport- specific questions. Where in the shoulder does pain occur? When in the throwing cycle does the pain occur? Posterior shoulder pain associated with late cocking or early acceleration can involve the labrum or rotator cuff. Is the pain present all the time or after throwing? During which inning does the arm start to hurt? Is the pain associated with the feeling of instability? Has there been any loss in velocity or control? Is the loss in velocity or control because of pain or fatigue? Are there mechanical symptoms such as clicking or grinding? Does the pain radiate down the arm? Does the patient experience the sensation of the arm “going dead”?
Finally, it is important to know why the patient came to see the doctor. Are you the first, second, or third opinion? After an acute injury, the problem is usually focused. However, in the patient with a long-standing problem, the reason for the visit may be more complex. For example, the goals of a patient coming in after a season of pain often differs from the patient coming in right at the onset of symptoms. It is important to understand not only the potential pathology in the patient but also the goals of the player with regard to future playing plans.
Physical Examination
Evaluation of a thrower with shoulder pain requires a global assessment, as pathology in the glenohumeral joint could be the result of breakdown anywhere in the kinetic chain. Although actual observation of the patient in action is not always possible in the clinic, a ground up approach should be taken. Asking the patient to simulate the throwing motion evaluates footwork and timing. The
one-legged stance and squat can assess pelvic and core stability. For example, in the dynamic Trendelenburg test, a pitcher should be able to perform a single-leg half squat without ipsilateral femoral adduction, internal rotation, or contralateral pelvic drop and trunk lean (2). Proper pitching mechanics require a stable foundation.
one-legged stance and squat can assess pelvic and core stability. For example, in the dynamic Trendelenburg test, a pitcher should be able to perform a single-leg half squat without ipsilateral femoral adduction, internal rotation, or contralateral pelvic drop and trunk lean (2). Proper pitching mechanics require a stable foundation.
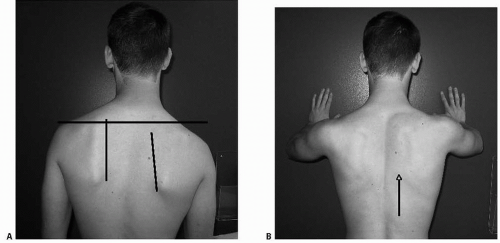
Evaluating the upper extremity in a thrower expands the standard adult shoulder exam of inspection, palpation, range of motion, strength, and stability testing. Visual inspection of the thrower’s posture, scapular position, and resting arm position is important. It is likely that the pitching or throwing arm will be overdeveloped in relation to the contralateral side, and slight asymmetry in scapular position may be present. While standing behind the patient, scapulothoracic motion should be assessed by having the patient perform active forward flexion of both upper extremities followed by a wall push-up. Gross asymmetry at rest and with motion or ipsilateral winging suggests scapular dyskinesis (Fig. 20.2). Prominence of the inferomedial border of the scapula at rest is often caused by weakness of the rhomboids, levator scapulae, and serratus anterior muscles that allow inferior displacement, lateral displacement, abduction, and protraction of the scapula in relation to the contralateral side (3). At the level of the glenoid, this produces an unbalanced platform for the humeral head, which can lead to injury of the glenohumeral joint.
Throwers often cannot point to the exact spot that elicits symptoms, particularly if labral pathology is involved. Instead, patients may complain of vague anterior or posterior pain, and very frequently complain of pain “deep” in the shoulder. Therefore, palpation may not pinpoint the diagnosis. However, thorough palpation of the shoulder region may identify periscapular crepitus or other associated symptoms such as tenderness over the biceps tendon or the acromioclavicular (AC) joint.
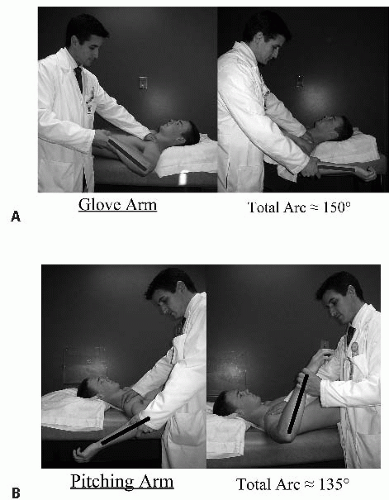
Standard range of motion testing should be followed by careful examination of glenohumeral rotation. Several longitudinal studies have shown that developmental changes in the shoulder capsule and an acquired proximal humeral retroversion lead to an arc shift that favors external rotation of the throwing arm. While supine with the arm abducted to 90°, throwing athletes, particularly pitchers, may have an additional 10° to 20° of external rotation and an equivalent loss of internal rotation in the throwing arm. However, the total arc should be within 10° to 15° of the contralateral limb. Loss of total arc with an associated glenohumeral internal rotation deficit (GIRD) >40° is pathologic and suggests a tight posterior capsule (Fig. 20.3).
Examination of shoulder strength involves testing the large motors (deltoid, pectoralis major, biceps, and triceps) as well as scapular and glenohumeral stabilizers. The rotator cuff is the primary dynamic stabilizer of the glenohumeral joint. Supraspinatus weakness or alterations in the force couple between the infraspinatus, teres minor, and the subscapularis can lead to altered kinematics throughout late cocking, acceleration, or deceleration phases. Although not entirely specific, supraspinatus strength is generally tested against resistance by comparison with the contralateral side, holding the arm in 90° of abduction and in the plane of the scapula. The infraspinatus is tested with resisted external rotation while the arm is held at the patient’s side, and the teres minor is tested by resisting external rotation with the arm forward flexed approximately 45°. The subscapularis is tested
with a posterior liftoff test and belly press maneuver (4). In addition to an abnormal wall push-up, scapular retraction with the belly press correlates with periscapular weakness.
with a posterior liftoff test and belly press maneuver (4). In addition to an abnormal wall push-up, scapular retraction with the belly press correlates with periscapular weakness.
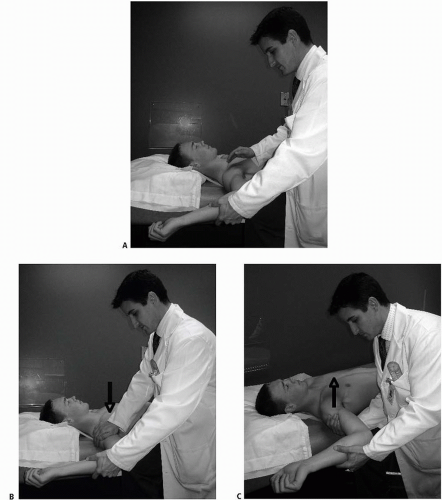
Anterior and posterior stability testing should be performed routinely. In addition to load-shift maneuvers and sulcus testing, the Jobe relocation test is a provocative maneuver that can detect subtle anterior instability and internal impingement (5). While lying supine, the patient’s arm is abducted to 90°, and maximum external rotation stress is applied. If anterior pain or apprehension is noted, it may be consistent with anterior instability symptoms. If a posteriorly directed force to the proximal humerus relieves the patient’s symptoms, or if an anterior force to the humerus worsens the patient’s symptoms (reverse relocation), the diagnosis of anterior instability is reinforced (Fig. 20.4). If posterior pain is elicited with abduction-external rotation testing, then internal impingement should be suspected.
Other provocative tests include the Neer forward flexion maneuver and the Hawkins abduction internal rotation exam for external impingement. The O’Brien active compression test examines the glenoid labrum and biceps anchor. Pain with resisted forward flexion, adduction, and internal rotation of the shoulder joint, relieved with external rotation of the shoulder joint, is suspicious for superior labral pathology (Fig. 20.5). Speed’s test, Yergason’s maneuver, Andrew’s clunk test, and the anterior slide test also stress the glenohumeral joint in an attempt to identify labral or biceps pathology (6). Currently, there is no single exam or test that can reliably delineate the solitary cause of internal derangement in the glenohumeral joint, but in combination, they can assist in formulating a differential diagnosis and orchestrating a treatment plan (7).
Imaging
Plain radiographs should be obtained to evaluate osseous abnormalities. Anterior-posterior (AP), scapular-Y, and axillary views should be routinely obtained. Glenohumeral rotation views can be ordered as necessary—the external rotation view is helpful in evaluating a young pitcher with proximal humeral epiphysiolysis. If patients have a current or past history of dislocation, the Stryker notch view is helpful in demonstrating the presence of a Hill-Sachs lesion. Standard radiographs can be helpful in identifying rotator cuff calcific tendinopathy, AC arthropathy, and exostosis of the posterior-inferior glenoid, or Bennett lesion. Although the Bennett lesion may be symptomatic, it is usually an incidental finding, and other sources of pathology should be ruled out prior to treatment of a Bennett lesion (8).
CT scanning, especially with three-dimensional reconstruction, provides enhanced evaluation of bony architecture but lacks the ability to assess the soft tissue envelope. CT scanning is not used routinely in the evaluation of throwers with shoulder pain. CT arthrography can be helpful in diagnosing full thickness rotator cuff tears and anterior labral injury but is not so reliable when evaluating partial thickness rotator cuff tears or injuries to the posterior or superior labrum.
MRI usually follows plain radiography and represents the diagnostic tool of choice for shoulder injuries in a thrower. MRI is helpful in the diagnosis of rotator cuff disease and labral pathology, including superior labrum anterior and posterior (SLAP) tears, anterior capsulolabral pathology, and perilabral cysts. Gadolinium-enhanced magnetic resonance arthrography (MRA) is thought to improve the reliability of diagnosing superior labral injuries and partial thickness rotator cuff tears. Extravasation of contrast under the superior labrum on the oblique, coronal, and axial views (Fig. 20.6) is indicative of a SLAP injury. The rotator cuff can be evaluated on several views; however, the oblique coronal provides an excellent view of the rotator cuff insertion. Anterior capsulolabral labral injury, perilabral cysts, and humeral avulsion injuries are best seen on the axial projections.
After the appropriate imaging studies, if there is any doubt as to the presence or the significance of the labral tear, other sources of pain should be considered.
Subacromial bursitis, rotator cuff tear, AC-joint pathology, Bennett lesion, coracoid impingement, synovial cyst with suprascapular nerve dysfunction, adhesive capsulitis, acute cartilage injury, and degenerative arthropathy all may contribute to pain in the throwing shoulder. Noninvasive tests such as anesthetic injections or electromyographic (EMG) analysis can further help to distinguish the primary cause of discomfort.
Subacromial bursitis, rotator cuff tear, AC-joint pathology, Bennett lesion, coracoid impingement, synovial cyst with suprascapular nerve dysfunction, adhesive capsulitis, acute cartilage injury, and degenerative arthropathy all may contribute to pain in the throwing shoulder. Noninvasive tests such as anesthetic injections or electromyographic (EMG) analysis can further help to distinguish the primary cause of discomfort.
BIOMECHANICS OF INJURY
The first step, or tipping point, in the disease process that causes pain and loss of performance in an elite thrower is still unknown. Static or passive motion biomechanical data that is currently available does not equal true active shoulder kinematics, and much is still unknown regarding the transition points between the late cocking, acceleration, and deceleration phases. Surgeons only see the resultant pathology, and since the findings are often similar, inferences have been made in attempts to complete the puzzle. Although often grouped separately, it is likely that the “dead arm” syndrome, internal impingement, SLAP lesions, posterior partial articular-sided rotator cuff avulsion (PASTA) lesions, posterior capsular contracture with GIRD, and anterior microinstability are all part of a spectrum of injury. The repetitive microtrauma associated with abduction-external rotation and traction stress induced during the throwing motion typically leads to injury (Fig. 20.7). While an injury to one solitary component can lead to injury in others, there are certain inherent characteristics that predispose a thrower to injury. Fatigue, game-time pressure, and a potential loss of focus can set the stage for altered kinematics leading to injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree