Arthroscopic Approach to Glenohumeral Arthritis
Felix H. Savoie III
Michael J. O’Brien
Arthritis of the shoulder is not as commonly seen as arthritis of the knee and hip. However, the shoulder is the third most common joint where prosthetic replacement is performed, and the incidence of osteoarthritis of the shoulder appears to be on the rise (1). Additionally, more patients of a younger age are presenting with degenerative changes of the glenohumeral joint. These patients are less willing to tolerate or accept the decrease in activity level required for longevity of total shoulder arthroplasty. Young patients with degenerative joint disease of the shoulder are increasingly requesting alternative treatments to shoulder arthroplasty in order to maintain a physically active lifestyle.
Younger patients have shown dissatisfaction at adopting a restrictive lifestyle following shoulder replacement. Sperling et al. (2) have shown a very high subjective dissatisfaction rate with total shoulder arthroplasty in these young patients and have projected a loosening rate of over 50% by 10 years. These finding have led to an investigation into alternative measures for the active individual with degenerative joint disease of the shoulder. Early pioneer work by Ellman et al. (3) indicated little usefulness for arthroscopy in the degenerative shoulder. However, Guyette et al. (4) found value to arthroscopic subacromial decompression in patients with both low-grade glenohumeral arthritis and impingement syndrome. Weinstein et al. (5) also found benefit to arthroscopic debridement in the degenerative shoulder with a 1-to 5-year follow-up. Richards and Burkhart (6) found some benefit to capsular release in the arthritic shoulder, postulating the decrease in compressive forces from the release provided some benefit. Dews et al. have reported the results of capsular release and decompression in a subset of patients with arthritis and impingement with promising early results (Dews R, Field LD, Savoie FH, et al. Early arthroscopic contracture release for severe postoperative shoulder stiffness. unpublished data).
Arthroscopic resurfacing of the glenoid in the degenerative shoulder was initially proposed by Brislin et al., (7) with additional reports by Bhatia et al., (8) and by Pennington and Bartz (9). Savoie et al. later reported midterm follow-up of the procedure first reported by Brislin (10). These procedures were based on open work performed at the Carrell clinic by Krishnan et al. (11). Although each has utilized various resurfacing tissues, the early results have been quite encouraging. However, other reports by Elhassan et al. (12) and others have delineated less than satisfactory results with a similar procedure, calling into question whether this is a reasonable treatment protocol. More encouraging is the recent report by Wirth (13) on biologic resurfacing of the glenoid with good early results (13).
The purpose of this chapter is to describe the role of arthroscopy and arthroscopic-assisted surgery in the management of glenohumeral arthritis. It should be understood that shoulder replacement remains the gold standard and is the treatment of choice for most patients requiring surgery for arthritis of the shoulder.
CLINICAL EVALUATION
History
The patient with degenerative joint disease of the shoulder usually presents with pain and loss of motion. The usual complaints are those of stiffness in the early morning along with pain during activities requiring a full arc of motion. Occasionally difficulty with sleeping may be reported although this is more commonly noticed during changes of position. In those patients with coexisting pathology in the subacromial area, the symptoms may be more of impingement and rotator cuff tendonitis rather than arthritis. There may be additional symptoms related to the degenerative acromioclavicular joint in addition to the problems in the glenohumeral joint.
Physical Examination
The initial aspects of the physical examination center on inspection and palpation. The shoulder is evaluated for atrophy and bone contours. The neurovascular status of the extremity is similarly evaluated. Passive and active range of motion is checked, and the amount of loss is compared with the opposite side. In these patients, there is always a loss of internal rotation in abduction. In the more severe
cases, a global loss of motion that mimics adhesive capsulitis can be detected even with the arm in adduction. The differentiating factors between the two of these, besides the normal radiographic appearance of adhesive capsulitis, include the lack of tightness in palpating the rotator interval and the lack of pain on inferior glide testing. Even in the early arthritic shoulder, there may be crepitation associated with movement of the humeral head on the glenoid.
cases, a global loss of motion that mimics adhesive capsulitis can be detected even with the arm in adduction. The differentiating factors between the two of these, besides the normal radiographic appearance of adhesive capsulitis, include the lack of tightness in palpating the rotator interval and the lack of pain on inferior glide testing. Even in the early arthritic shoulder, there may be crepitation associated with movement of the humeral head on the glenoid.
It is important to check for additional pathology. Concomitant impingement, biceps tendonitis, or acromioclavicular arthritis may be present in addition to the glenohumeral arthritis. All these can be detected by the usual examination findings.
Imaging
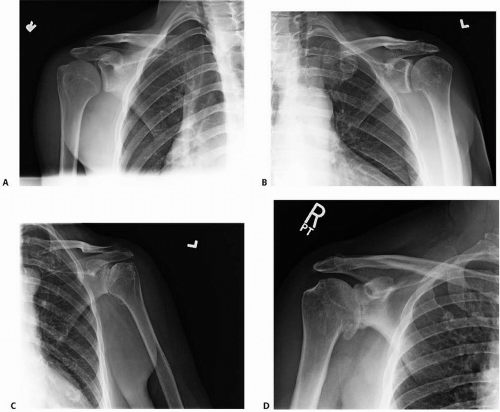
Standard PA (posterior to anterior), scapular Y, and axillary lateral radiographs are essential on the initial visit. Common findings may include small inferior spurs on the humerus noticed in the PA (posterior to anterior) view, slight posterior subluxation on the Y view, and narrowing of the joint on the axillary lateral view (Fig. 24.1). Determination of asymmetrical glenoid wear may also be assessed on the axillary lateral radiograph.
MRI testing is often performed. Current MRI units provide less than optimal assessment of the status of the articular cartilage but may be helpful in detecting additional
pathology in the labrum, biceps, and rotator cuff. There are technologic advances in the current systems that may allow better determination of the amount of damage to the articular cartilage. The addition of saline or gadolinium may be helpful in outlining suspected defects in the articular surface.
pathology in the labrum, biceps, and rotator cuff. There are technologic advances in the current systems that may allow better determination of the amount of damage to the articular cartilage. The addition of saline or gadolinium may be helpful in outlining suspected defects in the articular surface.
Classification
The most useful initial classification is the radiographic one of Weinstein et al. (5) In this system, the grading is based on radiographs. Stage I has normal radiographs. Stage II demonstrates joint narrowing with a concentric humeral head and glenoid. Stage III has moderate joint space narrowing with early inferior osteophyte formation. Stage IV includes severe joint space narrowing with osteophyte formation and loss of concentricity between the humeral head and the glenoid (Fig. 24.2).
The morphology of the glenoid can be determined by radiographic appearance utilizing the system described by Walch et al. (14) In this classification, a Type A glenoid shows concentric wear, which is either minor (Type A1) or major with substantial central wear causing a glenoid cup (Type A2). Type B has asymmetrical posterior glenoid wear with loss of joint space and sclerosis that is predominantly posterior (Type B1); or a posterior cup that gives the appearance of a double concavity or biconcavity (Type B2). Type C is defined as glenoid retroversion of greater than 25° and represents posterior glenoid hypoplasia.
The most common classification system grading articular cartilage injuries is that of Outerbridge (15). This system is based on direct inspection of the surface. Grade 1 change shows softening or blistering. Grade 2 shows fibrillation or superficial fissures of less than 1 cm, whereas Grade 3 shows deep fissuring extending to the subchondral bone and measuring more than 1 cm. Grade 4 shows exposed bone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree