Arthroscopic Ankle Arthrodesis
Brad D. Blankenhorn
Troy M. Gorman
Florian Nickisch
Timothy C. Beals
Charles L. Saltzman
Arthroscopic ankle arthrodesis was first developed in the mid 1980s, and the technique has been refined over the past 20 years. In the appropriate patient, arthroscopic joint preparation combined with percutaneous joint stabilization allows for a minimally invasive approach to ankle arthrodesis that can decrease a patient’s perioperative risks. The main advantage of arthroscopic arthrodesis over open arthrodesis is that it can be utilized in patients who have a compromised soft tissue envelope from trauma, previous surgeries, rheumatoid arthritis, or diabetes.
Over the past two decades, arthroscopic ankle arthrodesis has become a viable alternative to the open procedure and has shown consistently encouraging results (1, 2, 3 and 4). Proposed advantages of arthroscopic techniques are less postoperative pain and morbidity, decreased blood loss, and a shorter hospital stay.
ANATOMY AND PATHOGENESIS
The ankle joint is formed by the interaction of the tibia, talus, and fibula. The distal tibia along with the medial and lateral malleoli forms the ankle mortise. The talar dome is contained within this mortise. The ankle mortise confers inherent bony stability due to its congruency, but is also further stabilized by soft tissue structures. These structures include the ligaments of the syndesmosis, the ankle capsule, the anterior and posterior talofibular ligament, the calcaneofibular ligament (CFL), the intermalleolar ligament, and the deltoid ligament complex.
Ankle arthritis differs from hip and knee arthritis in that the principle cause of end-stage ankle arthritis is posttraumatic degeneration. The relative resistance of the ankle joint to primary osteoarthritis is likely due to a combination of its congruency, which results in inherent stability and restrained motion, and the cartilage’s unique tensile properties and distinct metabolic characteristics. Unfortunately, the ankle seems quite susceptible to posttraumatic arthritis, and this may be related to its thinner and stiffer articular cartilage not being able to accommodate articular step-offs or the stresses of improperly constrained motion. Step-offs lead to increased local contact stresses that the thin cartilage of the ankle may not be able to accommodate as well as the thicker cartilage in the hip and knee (5, 6). These increased localized contact stresses likely contribute to the degeneration in articular cartilage that is seen following trauma. Other disease processes such as Charcot arthropathy or osteochondritis with large osteochondral defects can lead to step-offs or incongruity in the articular surface resulting in increased contact stresses.
Secondary osteoarthritis of the ankle can develop after fracture or ligamentous injury. Rotational ankle fractures and ligamentous injury with recurrent instability are the most common causes (7, 8, 9, 10 and 11). In the senior authors’ practice over a 13-year time period, 445/639 (70%) patients with Kellgren-Lawrence grade 3 and 4 ankle arthritis were posttraumatic, and only 46 (7.2%) had primary oseteoarthritis (9). Other recorded etiologies in this study for ankle arthritis include neuropathic disease (Charcot neuroarthropathy), inflammatory arthropathies (RA), crystalline arthropathies (pseudogout), osteochondritis, osseous necrosis, and postinfectious arthropathy.
INDICATIONS
General indications for ankle arthrodesis include degenerative arthritis with significant pain unresponsive to nonoperative interventions, large OsteChondritis Dessicans (OCD) not amendable to other interventions, osseous necrosis of the talus, failed total ankle replacement, and malalignment or instability from a paralytic deformity.
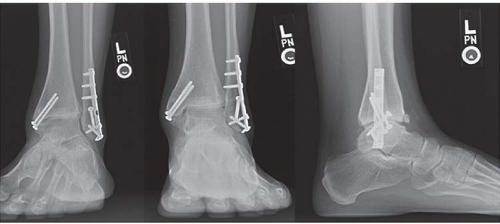
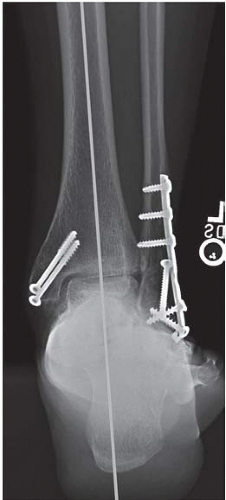
Indications for arthroscopic ankle arthrodesis remain the same with the exception of failed total ankle replacement. Well-aligned ankles and those that are easily realigned are excellent candidates for arthroscopic fusion (Fig. 93.1). Patients with soft tissue compromise (previous trauma, burn victims, patients with muscle flaps or skin grafts) or vasculopathy are strongly considered for an arthroscopic approach. Previously, it was felt that ankle varus or valgus greater than 5° was an absolute contraindication to arthroscopic arthrodesis. However, recent reports have
suggested substantial ankle varus or valgus is a relative contraindication rather than an absolute one (12, 13 and 14). The authors consider any ankle that can be realigned properly after arthroscopic debridement appropriate, but acknowledge that patients should be counseled that conversion to an open approach is prudent if an extensive capsulotomy or bony resection is required to achieve correct alignment. Additional contraindications for the arthroscopic procedure are significant focal bone loss and deformity and extremely rigid ankles. In general, the desired position of the arthrodesis is neutral dorsiflexion, 0° to 5° of ankle valgus, equal or slightly greater external rotation compared with the contralateral leg, and placement of the anterior aspect of the talar dome at or posterior to the level of the anterior aspect of the tibia.
suggested substantial ankle varus or valgus is a relative contraindication rather than an absolute one (12, 13 and 14). The authors consider any ankle that can be realigned properly after arthroscopic debridement appropriate, but acknowledge that patients should be counseled that conversion to an open approach is prudent if an extensive capsulotomy or bony resection is required to achieve correct alignment. Additional contraindications for the arthroscopic procedure are significant focal bone loss and deformity and extremely rigid ankles. In general, the desired position of the arthrodesis is neutral dorsiflexion, 0° to 5° of ankle valgus, equal or slightly greater external rotation compared with the contralateral leg, and placement of the anterior aspect of the talar dome at or posterior to the level of the anterior aspect of the tibia.
CONTRAINDICATIONS
Absolute contraindications include active infection and active Charcot arthropathy. However, after appropriate treatment of an infection and resolution of the metabolic issues associated with Charcot arthropathy, arthrodesis is an acceptable treatment for these problems. Some surgeons may consider active smoking by the patient a relative contraindication.
CLINICAL EVALUATION
Physical Exam
Examination begins with observation, especially when you have the opportunity to watch the patient walk into the exam room. Having the patient walk as part of the exam is informative, and observing overall lower extremity alignment and gait pattern is critical. Restricted ankle motion leads to early heel rise and a bent knee gait. The posture of the forefoot when it strikes the ground should be noted, as excessive forefoot varus or valgus is important to consider in surgical planning. Upon standing, the position of the hindfoot should be recorded as well. External rotation of the lower extremity is a common feature of patients with ankle arthritis.
The seated exam includes evaluation of range of motion in the ankle, hindfoot, midfoot, and forefoot. Ankle stability should be assessed by drawer testing, with the foot in both plantarflexion and neutral position. This investigates the competence of the anterior talofibular ligament (ATFL) and CFL, respectively. Talar tilt should also be assessed. Foot alignment is important as deformity in the foot may cause secondary ankle disease. For example, pes planus with medial column instability may be associated with secondary ankle valgus and eventual degenerative change. Conversely, realignment of a deformed ankle can alter the foot position and adversely or positively affect function of other joints, particularly the subtalar joint. If compensatory foot deformities are noted on exam, their passive correctability has to be assessed. Tendons should be palpated to identify potential confounding sources of pain. Furthermore, finding the point of maximal tenderness during the exam may help in diagnosis if there are multiple degenerative joints. A vascular exam should be performed with palpation of pulses and assessment of the distal capillary refill. The exam is completed with a neurologic assessment looking for motor or sensory deficits.
Imaging
Weight-bearing radiographs will better elicit deformity or soft tissue instability and should be obtained if possible. The four radiographic views we use in our clinic to evaluate ankle pain include the anteroposterior, lateral, mortise, and hindfoot alignment view. Radiographs of the degenerative ankle will show joint space narrowing, osteophyte formation, subchondral sclerosis, and subchondral cysts. When considering arthroscopic tibiotalar arthrodesis,
increased scrutiny should be applied to evaluating these standard radiographs. Anterior subluxation of the talus should be noted. Significant anterior subluxation will be difficult to correct with the limited capsular releases afforded during an arthroscopic approach. Special attention should be directed toward assessing degeneration of the distal tibiofibular joint and the formation of osteophytes in the medial and lateral gutters of the ankle. Failure to identify bony impingement in these areas can result in the inability to correct deformity or result in persistent pain postoperatively. If there is concern that these areas cannot be dealt with adequately through an arthroscopic approach, then open tibiotalar arthrodesis should be pursued.
increased scrutiny should be applied to evaluating these standard radiographs. Anterior subluxation of the talus should be noted. Significant anterior subluxation will be difficult to correct with the limited capsular releases afforded during an arthroscopic approach. Special attention should be directed toward assessing degeneration of the distal tibiofibular joint and the formation of osteophytes in the medial and lateral gutters of the ankle. Failure to identify bony impingement in these areas can result in the inability to correct deformity or result in persistent pain postoperatively. If there is concern that these areas cannot be dealt with adequately through an arthroscopic approach, then open tibiotalar arthrodesis should be pursued.
The hindfoot alignment view is important in the evaluation hindfoot varus/valgus and ankle coronal plane deformity (Fig. 93.2) (15). It is taken with the patient standing on a platform facing a collector that angles away from the platform at 20°. The X-ray tube is posterior to the ankle with the beam perpendicular to the plane of the film at the level of the ankle. On average, the most inferior aspect of the calcaneus is centered along the longitudinal mid-axis of the tibia.
CT is an excellent adjunct to standard radiographs to better delineate the three-dimensional bony anatomy. Arthroscopic tibiotalar arthrodesis may be difficult in the setting of significant bone loss or collapse, and CT allows for better evaluation of the bony structures. In addition, due to the high prevalence of posttraumatic tibiotalar arthritis, there is often orthopedic hardware from previous interventions present, and unlike MRI, cCTallows for visualization near hardware. Noninvasive joint distraction plus air-contrast arthrography enhances visualization of the ankle articular features, and can be used if there is a need to delineate between focal and global ankle arthritis (16). MRI has limited use unless one suspects an osteochondral lesion of the talus, osseous necrosis or ligamentous abnormality that will alter patient care. In such cases, MRI arthrography may be advantageous.
Selective fluoroscopically guided injections can also be helpful in patients who have clinical or radiographic findings that suggest more than one source of pain. It is reasonable to expect 75% pain relief in an area that is injected (17). It is important to identify the patients’ ankle pain as global (affecting a majority of the joint) or focal (specific region), as this distinction may guide the treatment options. It is particularly important to identify patients with coexisting subtalar pain as that population needs to be counseled more intensely about the risks of residual pain and progression of adjacent joint arthritis.
TREATMENT
Both nonoperative and operative treatments can help reduce symptoms and improve function of painful ankle arthritis. Nonoperative interventions primarily focus on treating symptoms through either medications or mechanical unloading and immobilization. The authors’ experience with nonsteroidal anti-inflammatory drugs (NSAID)s is that they seem to have variable efficacy in addressing the pain of ankle arthritis, but are still a mainstay of nonoperative treatment of ankle arthritis. The judicious use of corticosteroid or hyaluronate-based injections may provide temporary relief and be beneficial in acute exacerbations in someone who has tolerable steady state pain. Mechanical unloading or immobilization typically is conducted with a rigid ankle foot orthosis (AFO) or a leather ankle lacer with an imbedded polypropylene shell (18). If tolerated, bracing can be an effective means of controlling the pain associated with ankle arthritis. Adding a rocker bottom sole to a shoe or the use of a solid ankle cushioned heel (SACH) may also provide relief by reducing ankle excursion with gait.
Operative intervention should be considered only after failure of nonoperative treatment methods. When planning surgical interventions, it is critical to remember that recreating normal foot alignment will encourage improved foot function regardless of the chosen surgical technique. Surgical options for end-stage degenerative ankle arthritis include osteotomies about the ankle, debridement, distraction arthroplasty, total ankle arthroplasty,
and ankle arthrodesis. Ankle arthrodesis currently has the most predictable and consistent results for the treatment of end-stage ankle arthritis, and can be performed in a variety of ways including open, mini-open, and arthroscopic techniques.
and ankle arthrodesis. Ankle arthrodesis currently has the most predictable and consistent results for the treatment of end-stage ankle arthritis, and can be performed in a variety of ways including open, mini-open, and arthroscopic techniques.
If arthrodesis is the surgical treatment of choice, the next step is ensuring appropriate alignment at the fusion site. This requires taking the alignment of the entire limb into account. Malalignment or angulation of the tibia may require special consideration. In addition, adjustment may need to be made in the position of the fusion to ensure a plantigrade foot if the foot has significant forefoot varus or valgus or other foot malalignment. For example, if a patient has significant fixed forefoot varus, the ankle joint needs to be positioned in a little more valgus so a plantigrade foot can be created. Concomitant knee and ankle arthritis and deformity should be fully assessed and realignment at the knee is a priority prior to ankle arthrodesis. If there is significant deformity, arthroscopic ankle arthrodesis should be abandoned in favor of an open approach.
Careful scrutiny of the patient’s physical and radiographic exam are essential during the process of deciding which approach to take toward an ankle arthrodesis. If there is minimal or correctable coronal or sagittal plane deformity coupled with minimal degeneration of the distal tibiofibular joint and medial and lateral gutters, the patient is a good candidate for arthroscopic tibiotalar arthrodesis. A description of the technique follows.
ANTERIOR ARTHROSCOPIC SURGICAL TECHNIQUE
We recommend a general anesthetic to relax the gastrocnemius-soleus complex augmented with a regional block to aid in post-op pain control. At our center, a popliteal level indwelling catheter and a single injection saphenous block are placed with ultrasound imaging.
Patient Positioning
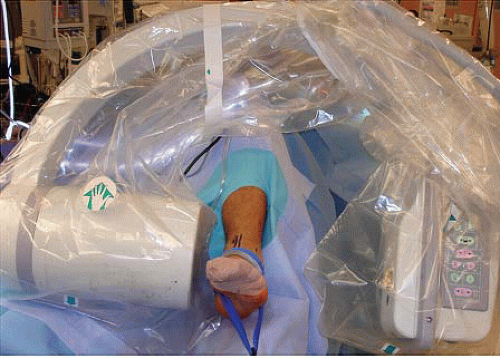
An arthroscopic ankle arthrodesis can be completed through either anterior or posterior arthroscopic portals. The anterior approach is favored for most cases, unless a subtalar fusion is also considered or there are soft tissue reasons (e.g., free flap, severe burns) not to do an anterior approach. In this situation, prone positioning and posterior portals would allow for arthroscopic preparation of both the tibiotalar and subtalar joints. For an anterior arthroscopic approach, the patient is placed in a supine position on the operating table with the operative leg in either a well leg holder (Fig. 93.3) or flat on the operative table depending on the type of external distractor used. When the leg is left out of the well leg holder, the bed can be adjusted (combination of reflex, Trendelenberg, and leg lowering) to create countertraction. Invasive distraction with a calcaneal or talar “skinny” wire or noninvasive distraction with an ankle strap can be used to facilitate joint visualization. If external strapping techniques are used to distract the joint, the force (generally <25 lb [11.3 kg]) should be decreased during preparation of the anterior talar dome, as this takes tension off the anterior capsule, allowing for easier access to talar dome. Use of thigh tourniquet is optional; we always place a tourniquet in case needed, and rarely inflate it. Prepping above the knee allows for assessment of rotational alignment. Prior to portal creation, we mark out landmarks including malleoli, palpable branches of the superficial peroneal nerve, and the expected level of the tibiotalar joint space.
Portal Creation
For anterior arthroscopy, standard anteromedial and anterolateral portals are created. The joint is insufflated by injecting approximately 20 cc (20 mL) of normal saline using an 18G needle placed anteromedially into the joint. The anterolateral portal is created after needle localization under direct arthroscopic visualization (Fig. 93.4). Both portals are created using the “nick and spread” technique to minimize the risk of injury to branches of the superficial peroneal nerve. For arthroscopic arthrodesis, the portals should be made larger than would normally be done for standard arthroscopy. The larger portals aid in the introduction of larger instruments that will facilitate a timely arthroscopic debridement. To enhance visualization and fluid flow, a 4.0-mm scope is routinely used for arthroscopic visualization. An arthroscopic pump is typically used to distend the joint; the pump is set at the lowest pressure needed to achieve visualization, and is generally adjusted several times in the operation to reduce tissue edema. It is not uncommon to have a significant amount of anterior capsular scarring and synovitis, which can make access to the joint difficult. This synovitis and scarring should be removed to facilitate visualization (Fig. 93.4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree