Arthroscopic Ankle Arthrodesis
James W. Stone
INTRODUCTION
The most common etiologies of joint degeneration are osteoarthritis, posttraumatic degenerative arthritis, and rheumatoid arthritis. Less common etiologies include hemophilic arthritis, congenital deformity, crystalline arthritis (gout and pseudogout), and osteochondral lesions of the talus. Management nonoperatively is often successful, but a subset of patients will continue to have pain and impairment to the extent that operative treatment is considered. Supramalleolar osteotomy, joint debridement, distraction arthroplasty, ankle arthroplasty, and arthrodesis are performed. Arthrodesis remains the standard operation for end-stage arthritis and can be performed with a variety of techniques (1, 2 and 3). In selected patients, arthroscopic ankle arthrodesis is an effective option, particularly for ankles that are reasonably well aligned, without a significant bony deficiency, and without severe stiffness (4, 5, 6, 7, 8 and 9).
INDICATIONS AND CONTRAINDICATIONS
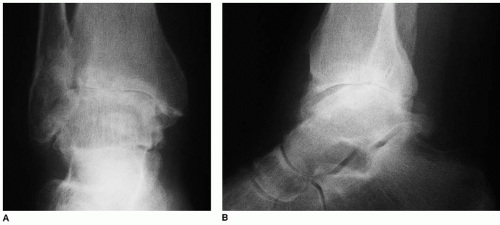
The most common indication for ankle arthrodesis is persistent ankle pain and disability from severe ankle arthritis unresponsive to nonoperative treatment, including the use of nonsteroidal anti-inflammatory medications, orthotics, braces, and corticosteroid injections. Radiographs may reveal loss of joint space, osteophyte formation, loose body formation, and joint malalignment (Fig. 36.1).
Contraindications to arthroscopic ankle fusion include patients with severe arthritic changes who also have significant ankle malalignment in valgus or varus. Arthroscopic ankle fusion cannot be used to correct deformity greater than approximately 5° to 10°. In particular, preoperative planning must be performed to ensure that the ankle can be placed into a neutral or slight valgus position. Varus position of the ankle fusion is poorly tolerated and may result in a painful callus on the lateral aspect of the foot. Patients with avascular necrosis of the talus have a lower rate of fusion with arthroscopic or open approaches and may represent a contraindication to arthroscopic ankle arthrodesis. The procedure is also contraindicated for patients with significant bone loss in the talus or tibia or active infection. Patients who have an equinus deformity who cannot be corrected to neutral position are not good candidates for surgery, unless efforts are directed toward correcting the equinus (e.g., joint debridement and tendon lengthening). Coexisting hindfoot arthritis is also a contraindication.
PREOPERATIVE PLANNING
A careful history and physical examination must be performed in preparation for an arthroscopic ankle fusion to be certain that the patient is a reasonable candidate for the procedure. The origin of the patient’s pain must be limited to the ankle joint. It is important to rule out other causes of hindfoot pain such as subtalar involvement or midfoot arthritis as contributing to the symptoms. Examination for swelling, tenderness, and range of motion of these joints is important. A good candidate for isolated ankle fusion must retain subtalar flexibility along with good midfoot motion which will substitute for the loss of ankle motion after successful fusion. Fixed varus deformity is a contraindication for the procedure. Passive dorsiflexion should be to at least neutral. If unable
to achieve neutral dorsiflexion, then the surgeon must assess whether this deformity can be corrected by removal of anterior osteophytes, perhaps in combination with gastrocnemius or Achilles lengthening.
to achieve neutral dorsiflexion, then the surgeon must assess whether this deformity can be corrected by removal of anterior osteophytes, perhaps in combination with gastrocnemius or Achilles lengthening.
Weight-bearing radiographs may be useful to assess hindfoot alignment and specialized views such as the Broden’s view of the subtalar joint are useful to rule out significant subtalar arthritis. Selective injection of the ankle joint and subtalar joint with local anesthetic may also assist in sorting out the etiology of the patient’s pain. Finally, a bone scan may be useful to obtain a broad assessment of the degree of degeneration of the other joints of the hindfoot and midfoot prior to committing to an isolated ankle fusion.
Patients with compromised skin due to peripheral vascular disease, prior surgical procedures, or those at higher risk of complication from open surgery such as a hemophilic patient may actually be better candidates for the arthroscopic procedure rather than an open arthrodesis.
SURGICAL TECHNIQUE
Ankle Distraction, Exposure, Joint Preparation
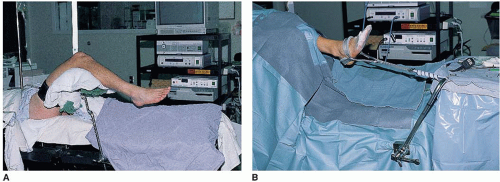
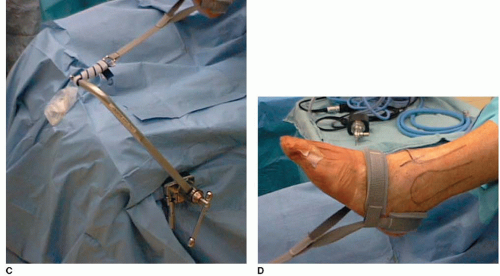
The patient is placed supine on the operating table, with the flexed hip and knee supported by a padded leg holder, as described in Chapter 33. The noninvasive ankle distractor is applied, and routine anteromedial, anterolateral, and posterolateral portals are created (Fig. 36.2).
The arthroscopic view shows large areas of cartilage loss (Fig. 36.3). If a large anterior osteophyte is present, it should be debrided as described in Chapter 33 to allow better joint visualization and better coaptation of the joint surfaces at the conclusion of the case.
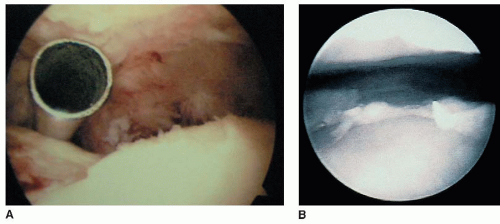
FIGURE 36.3 A: In the initial arthroscopic view of a severely arthritic ankle joint, the inflow cannula is seen. B: Large areas of complete articular cartilage loss are seen over the talar dome.

FIGURE 36.4 Various instruments, such as curettes and a shaver, are used to debride ligament, scar tissue, and articular cartilage from the medial and lateral gutters.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree