Fig. 33.1
Demonstration of the prone pivot shift exam, showing the elbow reduced (a), and subluxated (b) with a dimple over the dislocated radiocapitellar joint [Courtesy of Dr. Felix H. Savoie, III]
Imaging studies for PLRI can be helpful. Radiographs may reveal an avulsion fragment from the posterior aspect of the humeral lateral epicondyle in acute cases. However, radiographs are often normal. A stress radiograph or fluoroscopy while performing the pivot shift test may show the radial head and proximal ulna moving together in a subluxated and posterolaterally rotated position. Magnetic resonance imaging (MRI) of the elbow has been described to identify a lesion in the RUHL [8]. MRI arthrography is the best modality to identify lesions to the medial and lateral collateral ligaments. A formal arthrogram with injection of contrast dye into the elbow joint prior to the scan can greatly enhance the effectiveness of the test.
While much has been written about the pathoanatomy and biomechanics of the lesion, little has been reported on the surgical treatment of these patients. There are no large published series on the outcomes of the surgical treatment of PLRI. The present study reviews the outcomes of the authors’ experiences with arthroscopic repair, plication, and open grafting techniques previously described by the senior authors [4].
Surgical Technique
Most cases of simple dislocation respond to nonoperative management. However, return to full activities may take 3–4 months. In cases in which the instability recurs, or when initial evaluation reveals a bony avulsion of the lateral collateral ligament complex proximally off of the humerus, surgical treatment may be indicated. Acute repair of the RUHL may also be indicated in high level athletes, who cannot afford to miss large portions of the athletic season. Arthroscopy of the acutely injured elbow demands speed and precision. A concrete preoperative plan must be formulated and followed, with adjustment made for arthroscopic findings. Patients with significant coronoid fracture, associated radial head fracture or distal humerus fracture are not included in this report.
Arthroscopic Repair
In the elbow with an acute or chronic avulsion of the RUHL, arthroscopic repair can very effective. The procedure begins with the establishment of a proximal anterior medial portal and a diagnostic arthroscopy of the anterior compartment. Fractures of the radial head or coronoid can be identified. In the acute setting, abundant hematoma will be encountered in the joint (Fig. 33.2), and tearing of the anterior capsule is readily apparent. One can often also see the damage to the brachialis muscle through the torn capsule (Fig. 33.3a, b). A proximal anterior lateral portal can be established to clean out the associated hematoma.

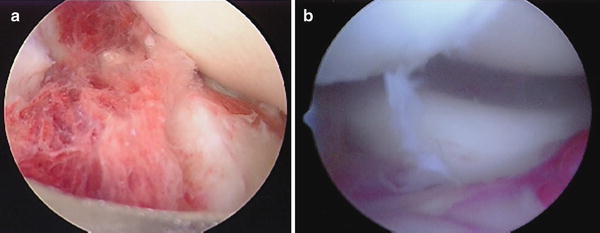

Fig. 33.2
A view from the proximal anterior medial portal of the hematoma often seen in an acute dislocation [Courtesy of Dr. Felix H. Savoie, III]
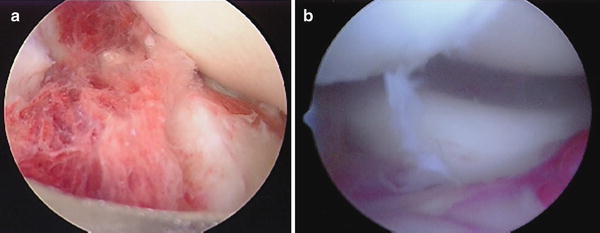
Fig. 33.3
(a) The arthroscopic view of the damaged brachialis and torn anterior capsule often noted in acute dislocations. (b) The laxity seen in the annular ligament and the displacement of the radial head from the capitellum in acute and chronic PLRI is visualized from the medial portal [Courtesy of Dr. Felix H. Savoie, III]
On the lateral side, laxity of the annular ligament and lateral collateral ligament (LCL) complex will be evident in every case. Occasionally, the LCL complex will be flipped into the radiocapitellar joint. Of importance is to view the annular ligament for damage and place a suture in it if necessary. Valgus load and forearm supination demonstrates posterolateral rotatory instability with the radial head subluxating off the capitellum, indicative of injury to the RUHL. One can also view “around the corner” of the proximal capitellum for damage to the collateral ligament part of the radial ulnohumeral ligament complex. On the medial side, an arthroscopic valgus stress test can be performed to evaluate for incompetence of the medial ulnar collateral ligament (MUCL). During evacuation of hematoma, great care is taken not to resect or damage the LCL complex.
The arthroscope is next placed into the posterior central portal, and the hematoma in the posterior compartment of the elbow is evacuated via a proximal posterior lateral portal. Both of these portals need to be relatively proximal to allow for the later repair of the ligament, usually at least 3 cm above the olecrenon tip. A view of the medial gutter will show hemorrhage, and sometimes tearing of the capsule, near the posterior aspect of the medial epicondyle (Fig. 33.4).
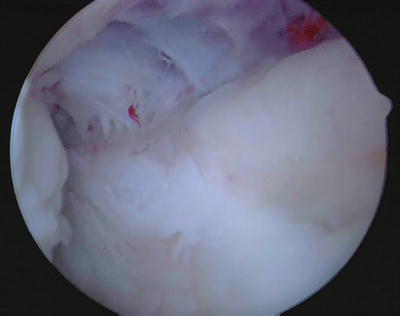
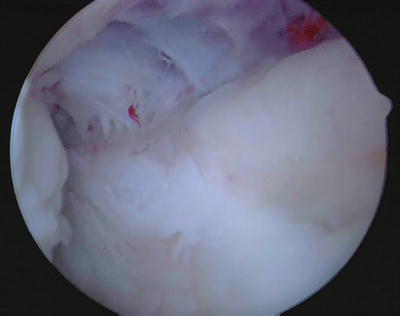
Fig. 33.4
The concomitant tearing of the capsule of the medial capsule in acute instability is visualized from a posterior portal [Courtesy of Dr. Felix H. Savoie, III]
One common finding is the ability to move an arthroscope placed down the posterolateral gutter from the posterior central portal straight across the ulnohumeral articulation into the medial gutter. This maneuver is not possible in a stable elbow, and is termed the “drive through sign of the elbow” (Fig. 33.5). It is somewhat analogous to the “drive through sign” in shoulder instability. The elimination of the laxity that allows this maneuver is one of the key aspects of confirming an adequate arthroscopic reconstruction in patients with PLRI.
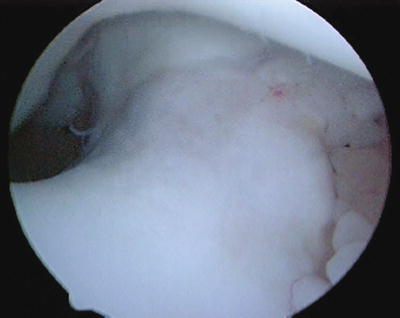
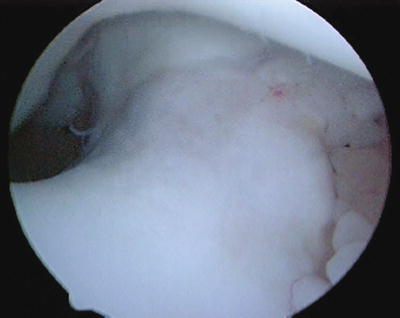
Fig. 33.5
The “drive through sign” of the elbow is performed by placing the arthroscope into the lateral gutter and moving it straight across the ulnohumeral articulation into the medial gutter [Courtesy of Dr. Felix H. Savoie, III]
The lateral gutter and capsule is evaluated next. The arthroscope is easily advanced down the lateral gutter, owing to incompetence of the LCL complex. It is very important to stay close to the ulna as the lateral gutter is evaluated and the hematoma debrided, as the avulsed ligament and bone fragments are displaced distally and may inadvertently be removed by the shaver (Fig. 33.6). The origin of the LCL complex on the posterior aspect of the lateral epicondyle can be visualized as a bare area where the ligament has avulsed off of the humerus. It is usually directly lateral and slightly inferior to the center of the olecrenon fossa. This area on the posterior humerus should be lightly debrided with a motorized shaver.


Fig. 33.6
The bone and soft tissue fragments often seen in the lateral gutter in acute dislocation [Courtesy of Dr. Felix H. Savoie, III]
Once the area of damage has been defined, an arthroscopic anchor may be placed into the humerus at the site of origin of the RUHL (Fig. 33.7). A percutaneous suture passer is placed through a “soft spot” portal to retrieve the sutures. The limbs of the suture are retrieved to place two horizontal mattress sutures through the non-injured part of the ligament. In the case of a bony avulsion, we place one set of sutures around the bone fragment and the other distal to the fragment (Fig. 33.8). The sutures are tensioned while viewing with the arthroscope down the lateral gutter, which should have the effect of pushing the arthroscope out of the lateral gutter as tension is restored to the LCL complex. The elbow is extended and the sutures are tied beneath the anconeus muscle, tightening the ligament. Motion and stability are evaluated with the arthroscope back in the anterior compartment (Fig. 33.9), confirming tension has been restored to the annular ligament.
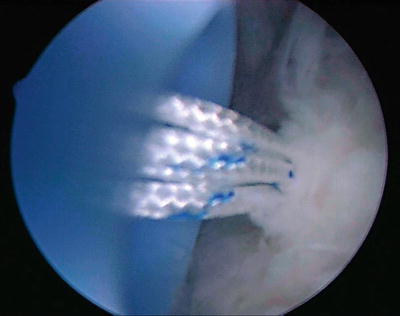
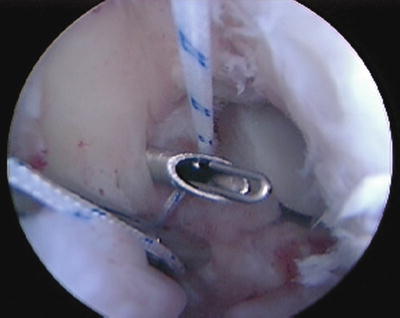
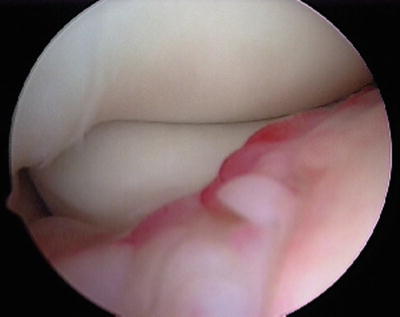
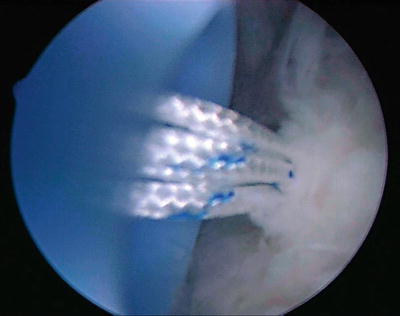
Fig. 33.7
The site of anchor placement into the humerus just lateral to the olecrenon fossa of the humerus as viewed from the posterior portal [Courtesy of Dr. Felix H. Savoie, III]
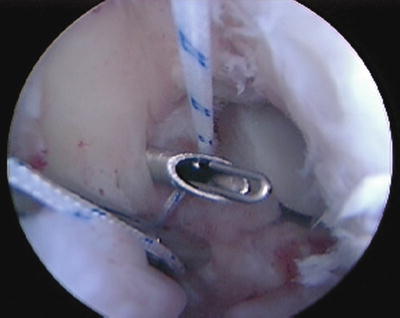
Fig. 33.8
Once an adequate anchor has been placed, the sutures are retrieved though the torn radio-ulnohumeral ligament in preparation for repair [Courtesy of Dr. Felix H. Savoie, III]
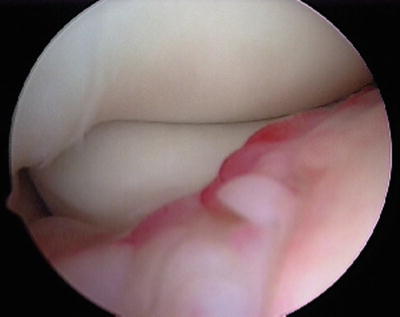
Fig. 33.9
The repaired ligament is visualized from the posterior portal [Courtesy of Dr. Felix H. Savoie, III]
Arthroscopic Plication
The development of an arthroscopic technique for the treatment of chronic PLRI was described by Smith et al. in 2001 [4]. Chronic posterolateral instability of the elbow is more readily seen during examination under anesthesia and on arthroscopic evaluation. While viewing from the proximal anterior medial portal, the ulna and radial head can be seen to subluxate posterolaterally during the performance of a pivot shift test. In most cases, the annular ligament is intact as the entire proximal radio-ulnar joint shifts on the humerus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








