Arthropathies Associated with Systemic Diseases
Leann Maska
Amy C. Cannella
 |
A 60-year-old Caucasian gentleman with long-standing poorly controlled type 2 diabetes mellitus presents to your office with symptoms of swelling and moderate pain in his right midfoot over the past 3 weeks. He is unable to recall any specific traumatic event. On examination, the foot is warm, swollen, tender, and erythematous (Fig. 22.1). Your differential includes cellulitis, acute gouty arthritis, osteomyelitis, and fracture. An important addition to this differential is consideration of acute Charcot neuroarthropathy (CN). To rule out underlying infection, the best imaging study is combination of a three-phase bone scan with a labeled white blood cell (WBC) scan.
Joint pain is one of the most common reasons for a patient to see his or her primary care provider. Office visits in the United States for musculoskeletal pain in 2000 accounted for 280 visits per 1,000 people, and were evenly divided between acute and chronic symptoms (1). Although not inclusive, this chapter aims to cover associations between a variety of systemic diseases and their related musculoskeletal manifestations.
Endocrine Diseases with Associated Arthropathies
Diabetes Mellitus
Diabetes is an increasingly common medical condition in the United States, with a prevalence of more than 23 million people, including both diagnosed and undiagnosed cases, or one in ten adults (2). Health care providers must be familiar with the myriad of extraglandular complications of the disease. It is thought that the associated arthropathies are due to complications of diabetes, including neuropathy and microvascular disease. Furthermore, a high-glucose and insulin environment has been shown to have pathologic effects on many key cells and matrix components of connective tissues (3). Although relatively uncommon, charcot neuroarthropathy is an important problem to recognize as it leads to significant deformity and joint destruction. Conversely, adhesive capsulitis of the shoulder is quite common, but often improves with conservative management. Both are discussed in more detail below. Other notable arthropathies associated with diabetes mellitus include diffuse idiopathic skeletal hyperostosis (DISH), carpal tunnel syndrome, and osteoarthritis.
Charcot Neuroarthropathy
Clinical Presentation
The incidence of CN is reported at approximately 1 in 333 patients with diabetes (4). The exact pathogenic mechanism of CN is incompletely understood; however, a combination of both neurovascular and neurotraumatic theories is generally accepted (4). Current hypothesis suggests that somatic and autonomic neuropathy leads to increased blood flow to the joint, resulting in bone resorption and susceptibility to minor trauma. Continued mechanical stress occurs because of loss of protective pain sensation, and major destructive changes result in fractures and deformities.
 Figure 22.1 Subluxation of the navicular and soft tissue swelling as an early manifestation of a neuropathic joint (Courtesy of Gerald F. Moore, MD.) |
Patients with CN can present with an acute or chronic process. In acute CN, the earliest symptoms are persistent swelling and pain, although sensory deficits may preclude associated discomfort. A history of trauma may be present, although one study showed that nearly 75% of patients did not recall any precipitating event. Progression from acute to chronic neuroarthropathy can be rapid, with irreversible damage seen in less than 6 months. Patients with chronic CN can present with established deformity and may complain of associated difficulties with ambulation.
Examination
On physical examination, a foot with acute CN is typically warm, swollen, and tender. Moderate-to-marked erythema may also be present (4). The midfoot is most commonly involved and has a better prognosis than hindfoot involvement because of weight distribution effects. Typical deformities include a collapsed arch and rocker-bottom foot with callus formation and possible ulcerations.
Studies
Diagnosis is primarily made by clinical history and examination. Plain radiographs are inexpensive and can show anatomic bony deformities, demineralization, and periosteal reaction. When severe, CN can result in fragmentation of the metatarsal heads, or even “pencil and cup” deformities of the MTP joints. Radiographic progression can occur rapidly, oftentimes within several weeks of a normal x-ray (Fig. 22.2) (4).
It is critical to rule out infection in the diagnostic work-up of CN. Radiographs are neither sensitive nor specific for differentiating infection from CN. The combination of a three-phase bone scan with a tagged WBC scan has a sensitivity and specificity of 80% to 90%. In acute CN, a three-phase bone scan should be positive in all three phases, reflecting increased bone turnover, and a tagged WBC scan should be negative in the absence of infection. However, false positive WBC scans can occur in the setting of very rapidly advancing CN. Further imaging can be done with complementary marrow scanning, which if positive in the same area, indicates acute neuroarthropathic changes and not infection (4). Although magnetic resonance imaging (MRI) does not differentiate CN from infection, it gives excellent anatomic definition, does not require gadolinium to see edematous changes, and may be useful for monitoring progression of disease (4).
Treatment
The management of CN is limited and mainly consists of reduction in weight-bearing activity. Plaster casting for several weeks to allow the acute phase to resolve, followed by total-contact cast applications that allow for better ambulation, is commonly utilized. Other specialized footwear for acute CN applications include Charcot restraint orthotic walkers,
patellar tendon-bearing braces, total-contact bivalve ankle-foot orthoses, and pneumatic walking braces that allow earlier mobilization with relative joint immobility (4). Treatment of chronic CN centers on reducing plantar pressures and preserving skin integrity to prevent ulcerations. Orthotic consultation can be very helpful in managing and treating chronic deformities. Routine surgery is not advocated, as potential risks include long-term worsening of the condition, possible nonunion, infection, and general risk of surgery and anesthesia.
patellar tendon-bearing braces, total-contact bivalve ankle-foot orthoses, and pneumatic walking braces that allow earlier mobilization with relative joint immobility (4). Treatment of chronic CN centers on reducing plantar pressures and preserving skin integrity to prevent ulcerations. Orthotic consultation can be very helpful in managing and treating chronic deformities. Routine surgery is not advocated, as potential risks include long-term worsening of the condition, possible nonunion, infection, and general risk of surgery and anesthesia.
Clinical Course
Early diagnosis of CN can potentially prevent complications including severe deformity, ulcerations, and even limb amputation. Because CN is a relatively uncommon condition, referral to a specialist with a multidisciplinary team approach is preferred.
Adhesive Capsulitis
Clinical Presentation
Compared to 2% to 5% of the general population, approximately 20% of people with diabetes are affected at some time by adhesive capsulitis of the shoulder. This relatively common condition is defined as the insidious onset of shoulder pain with a gradual loss of both active and passive range of motion (ROM) (5).
The natural history of adhesive capsulitis is a progression through four sequential and descriptive stages: (a) preadhesive stage (diffuse glenohumeral synovitis seen on arthroscopy); (b) freezing stage (hypertrophic and hypervascular synovitis with capsular fibroplasia and scar formation); (c) frozen stage (significant hypertrophy and hypervascularity with dense capsular scar); (d) thawing phase (apparent remodeling without synovitis) (5). Pain is initially severe and improves with decreasing synovitis in later stages. A progressive decline in ROM is notable until stage 4, or thawing occurs.
Sleep-disturbing pain is often a motivating factor for patients to seek medical attention. Certain elements of the history can help determine where each patient resides on the continuum (Table 22.1). For example, a patient who is unable to sleep through the night, has significant limitations in ROM, and suffers from ongoing pain is likely in stage 2, or active freezing.
Examination
Significant limitation of both active and passive abduction of the shoulder exist; however, the extent of restriction is stage dependent. Active ROM that is accompanied by scapular movement is a clue to diagnosis. Patients often display transient severe pain with abrupt or end-range movements. Although normal strength has been considered a classic finding, recent studies using handheld dynamometry have demonstrated weakness in the internal and external rotators, abductors, and elevators (5).
Table 22.1 Stages of Adhesive Capsulitis | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Studies
History and physical examination alone are often adequate to diagnose adhesive capsulitis. However, imaging studies can help rule out other pathology. Plain radiographs are limited to finding bony pathology. Magnetic resonance imaging can differentiate soft-tissue abnormalities of the rotator cuff and labrum. Ultrasonography has also proved to be useful in deciphering adhesive capsulitis from rotator cuff tendinopathy (5).
Treatment
Discussions with the patient should include education regarding the natural history of adhesive capsulitis, preparation for an extended recovery, and alleviation of fear of a more serious disease. A home exercise program outlined by a physical therapist can be effective in relieving symptoms, and also places the patient in an active role. Glenohumeral corticosteroid injection, exercise, and joint mobilization all lead to improved short- and long-term outcomes. Corticosteroid injections have been shown to result in more rapid improvements at 4- to 6-week intervals and are therefore a reasonable option for patients with more severe symptoms, who have not responded well to rehabilitation (5). However, there is concern for potentially elevated serum glucose levels in patients with diabetes who receive intra-articular corticosteroids. If conservative management is unsuccessful, obstinate frozen shoulder may be further managed with manipulation under anesthesia or surgical capsular release.
Clinical Course
Adhesive capsulitis is usually self-limited, lasting 12 to 24 months. However, mild symptoms can persist for years, depending on the extent of fibroplasias. Some studies report that up to half of patients have limited ROM more than 3 years after symptom onset.
Hypothyroidism
Symmetrical arthropathy with stiffness of the hands and knees is a common initial presentation of patients with hypothyroidism. Examination including palpation of involved joints may reveal synovitis. Synovial fluid is typically noninflammatory with high levels of hyaluronic acid.
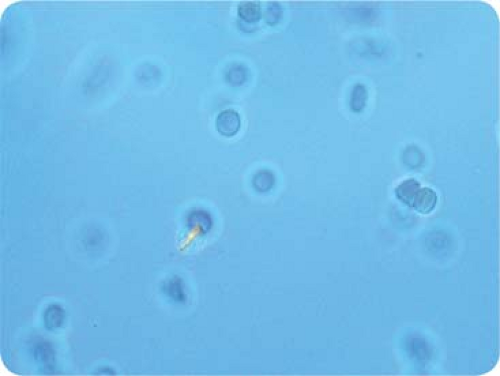
Hypothyroidism is also associated with calcium pyrophosphate deposition (CPPD), which would result in an inflammatory synovial fluid with weakly positively birefringent rhomboidal crystals seen under polarized light microscopy (Fig. 22.3). Indeed, multiple systemic diseases are associated with CPPD arthropathy (Table 22.2). Carpal tunnel syndrome can also be an initial presentation in up to 7% of patients with hypothyroidism.
Chronic autoimmune thyroiditis, or Hashimoto’s thyroiditis, has a variety of associated rheumatic manifestations, such as mild nonerosive arthritis, polyarthralgia, myalgia, and sicca syndrome. Most manifestations are secondary to hypothyroidism and do not resolve until a euthyroid state is achieved. However, in treated or euthyroid Hashimoto’s thyroiditis, arthropathies may be due to an associated autoimmune etiology, such as Sjogren’s syndrome, rheumatoid arthritis, or systemic lupus erythematosus.
Hyperthyroidism
Hyperthyroidism, including Grave’s disease, can present as pretibial myxedema and ophthalmopathy. Digital soft-tissue swelling with periostitis of metacarpophalangeal
(MCP) joints also occurs. Nail changes include onycholysis and clubbing (thyroid acropachy).
(MCP) joints also occurs. Nail changes include onycholysis and clubbing (thyroid acropachy).
Table 22.2 Systemic Diseases Associated with Calcium Pyrophosphate Deposition Arthropathy | |
|---|---|
|
Osteoporosis is a relatively common and serious manifestation of hyperthyroidism that should not be missed. Iatrogenic overreplacement of thyroxine can also lead to osteoporosis. Treatment goals include normalization of thyroid-stimulating hormone and improvement in bone mineral density as measured by densitometry.
Hyperparathyroidism and Hypovitaminosis D
Calcium homeostasis with bone metabolism and remodeling are intricately controlled by parathyroid hormone (PTH), vitamin D, and calcitonin levels. Primary hyperparathyroidism is often secondary to a parathyroid adenoma, whereas secondary disease is most commonly related to renal failure, vitamin D deficiency, and osteomalacia. Arthralgias are common in both primary and secondary disease, and can involve small joints of the hands, often sparing the proximal interphalangeal (PIP) joints. Radiographic changes include osteitis fibrosa cystica, erosions, phalangeal subperiosteal resorption along the radial edges, and even distal tuft resorption. Rheumatoid factor is typically negative and erythrocyte sedimentation rate normal. Calcium pyrophosphate deposition is associated with hyperparathyroidism, and acute gout attacks can also occur (Table 22.2). Either calcium pyrophosphate or uric acid crystals can be found in aspirated joint fluid from an acutely inflamed joint of a patient with hyperparathyroidism. Brown tumors (Fig. 22.4), which are lytic bone lesions, can be seen on radiographs and represent localized areas of fibrous tissue with increased osteoclastic activity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree