Arthrodesis of the Osteoarthritic Wrist
Robin R. Richards
Indications and Contraindications
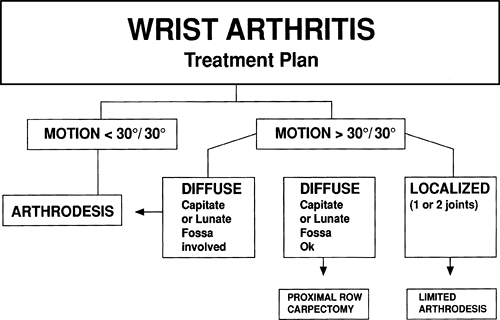
Posttraumatic arthritis of the radiocarpal and midcarpal joints is the most common indication for wrist arthrodesis. For example, a chronically nonunited scaphoid fracture or scapholunate dissociation with advanced carpal collapse and secondary degenerative arthritis can be treated effectively by wrist arthrodesis. When posttraumatic arthritis involves only the radiocarpal joint or midcarpal joint, wrist arthrodesis is an alternative to limited arthrodesis. Wrist arthrodesis often is required to salvage a failed previous, more limited arthrodesis or wrist arthroplasty (1,2). It is unlikely that any wrist reconstruction will improve motion. For this reason, wrist arthrodesis is recommended as the preferred initial treatment in cases of limited disease when wrist dorsiflexion and palmar flexion are less than 30 degrees (Algorithm 1).
Less frequent indications for wrist arthrodesis include diseases that cause significant instability, such as rheumatoid arthritis or infection. Cavaliere and Chung (3) found outcomes to be comparable and possibly better for wrist arthrodesis, in comparison to wrist arthroplasty, for patients with rheumatoid arthritis. Segmental bone loss involving the distal radius and carpus resulting from severe crush is another indication, as well as mutilating open injuries inflicted by gunshot blasts, saws, press injuries, or other industrial trauma (Fig. 27-1). Paralytic disorders can cause a wrist deformity interfering with hand function that is corrected most effectively by wrist arthrodesis in a position of stable alignment. At times, hand reconstruction for combined nerve palsy requires the use of a single residual functioning wrist motor, which is possible only by stabilization of the wrist. Addosooki et al. (4) reported on the use of wrist arthrodesis in conjunction with free muscle transfer for reconstruction following total brachial plexus palsy. Wrist arthrodesis can be indicated as a method of reconstruction following tumor resection (5). Freeland et al. (6) discussed performing the procedure for irreparable intra-articular distal radial fractures.
The primary contraindication to wrist arthrodesis is the rare situation in which motion is essential to perform a highly important or dependent activity. For example, a tetraplegic patient must have wrist dorsiflexion preserved to be capable of body transfer. A second contraindication is the necessity for wrist motion to provide for, or to augment, digital motion by tenodesis effect. De Smet (7) studied the correlation of wrist motion and disability in 205 patients who had had a variety of wrist operations. A correlation was seen between wrist motion and the Disabilities of the Arm, Shoulder and Hand (DASH) score, although the correlation was weak.
Preoperative Planning
Most patients considered for wrist arthrodesis have pain with use, limited wrist motion, and weakness. Physical findings vary with the location and extent of arthritis. It is important to note the presence and location of swelling, crepitus, and tenderness. It is desirable to record preoperative grip and range-of-motion measurements accurately. Examine the distal radioulnar joint to detect potential
problems such as pain, instability, or restriction of forearm rotation that may require surgical treatment in addition to wrist arthrodesis.
problems such as pain, instability, or restriction of forearm rotation that may require surgical treatment in addition to wrist arthrodesis.
Many patients with long-standing arthritis or wrist deformity also have symptoms of carpal tunnel syndrome. Even if the symptoms initially are mild, they can become clinically significant following surgery. Examine all patients scheduled to undergo wrist arthrodesis for the presence of carpal tunnel syndrome by Phalen’s test (8) and sensory testing. The symptoms of carpal tunnel syndrome can increase following wrist arthrodesis owing to perioperative edema formation. Carpal tunnel release should be considered before, or concomitant with, wrist arthrodesis when clinical evaluation is positive and the presence of a compressive neuropathy affecting the median nerve is confirmed by electrodiagnostic testing.
Appropriate radiographic evaluation includes an anteroposterior (AP) and lateral view as well as two oblique views. The oblique view best shows the extent of arthritic involvement. Carefully evaluate the ulnar midcarpal joint (triquetral-hamate and capitohamate) to determine if it is free of clinical and radiographic deformity or if it is arthritic and therefore requires inclusion within the fusion. The lateral view is helpful in evaluating the capitolunate and distal radioulnar joints.
Additional studies may be indicated based on the findings of the routine radiographs. An ulnar-deviated posteroanterior (PA) view often is needed to evaluate the scaphotrapeziotrapezoid joint for
arthritic deformity. A computed tomographic scan provides the best assessment for the capitolunate joint, which may be difficult to evaluate for arthritic deformity using routine radiographs. Surgery can be performed under axillary block or general anesthesia. A general anesthetic is required if an iliac crest bone graft is to be used. The involved extremity and the opposite iliac crest are prepared and draped if an iliac crest bone graft is to be performed.
arthritic deformity. A computed tomographic scan provides the best assessment for the capitolunate joint, which may be difficult to evaluate for arthritic deformity using routine radiographs. Surgery can be performed under axillary block or general anesthesia. A general anesthetic is required if an iliac crest bone graft is to be used. The involved extremity and the opposite iliac crest are prepared and draped if an iliac crest bone graft is to be performed.
 Figure 27-1 Anteroposterior radiograph of 34-year-old man who sustained a severely comminuted and contaminated gunshot wound to carpus with segmental bone loss across carpus and metacarpus. |
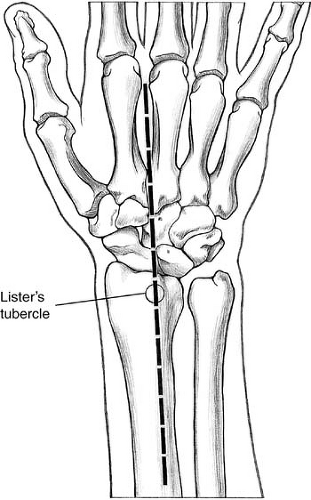 Figure 27-2 Center a straight dorsal incision from the radial aspect of the third metacarpal, across Lister’s tubercle, and across the dorsal distal radius. |
Technique
Inflate a brachial tourniquet 50 to 100 mm Hg above systolic pressure.
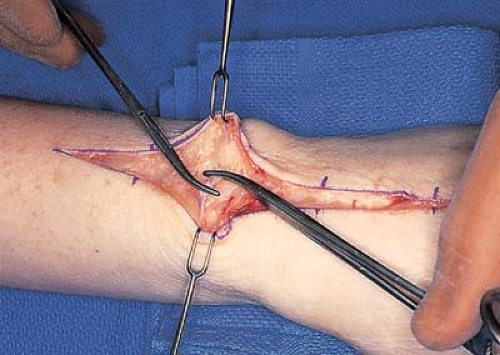
Place the wrist in neutral position with respect to radioulnar deviation, and make a straight incision beginning at the distal third of the index-middle interosseous space, proceeding across Lister’s tubercle, and ending over the radius at the proximal border of the abductor pollicis longus muscle (Fig. 27-2). One or two crossing veins may require division and suture ligature (Fig. 27-3).
Elevate a radially based skin and subcutaneous flap containing the dorsal sensory radial nerve off the extensor retinaculum.
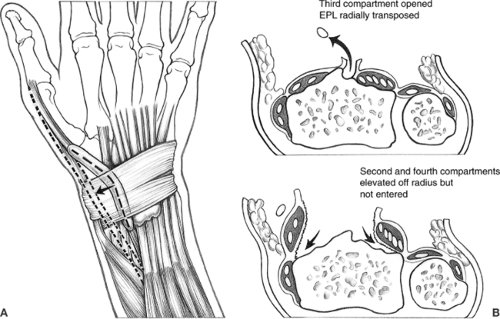
Step-cut the extensor retinaculum to allow for its repair at the conclusion of the procedure.
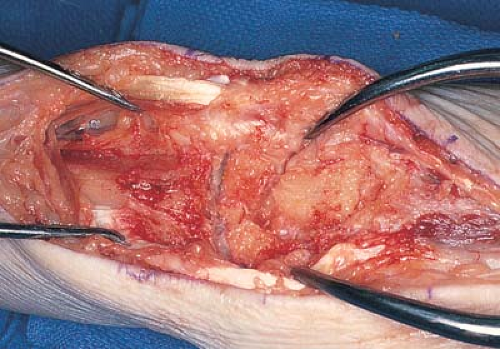
Open the third dorsal compartment, and elevate the extensor pollicis longus tendon and muscle (Fig. 27-4).
Incise the sheath distal to the retinaculum to allow adequate retraction of the extensor pollicis longus tendon (Figs. 27-5 and 27-6).
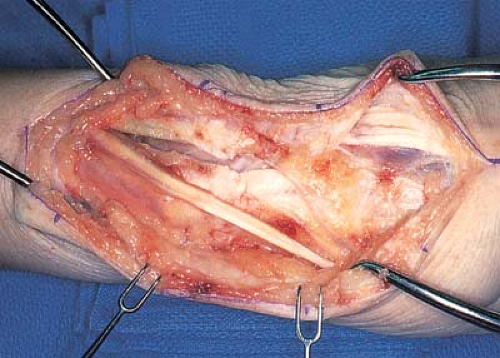
Place umbilical tapes around the extensor tendons so that they can be retracted as the procedure progresses.
Incise the periosteum over the long finger metacarpal after retraction of the overlying extensor tendons, and expose the dorsal aspect of the metacarpal subperiosteally.
Leave the radial and ulnar borders of the metacarpal undisturbed.
Make an incision through the dorsal wrist capsule, and extend it proximally to the radius along its dorsal surface.
With sharp dissection, dissect the capsule and second dorsal compartment radially, and elevate the capsule and fourth dorsal compartment ulnarly, taking care not to enter the undersurface of the compartment.
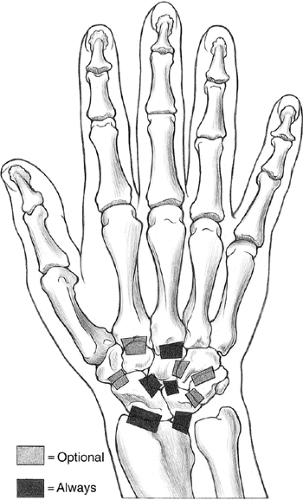
Expose the joint surfaces to be included in the fusion and decorticate them down to cancellous bone. The carpometacarpal joints of the long and index fingers, scaphocapitate joint, capitolunate joint, radioscaphoid joint, and the radiolunate joint are included as a rule.
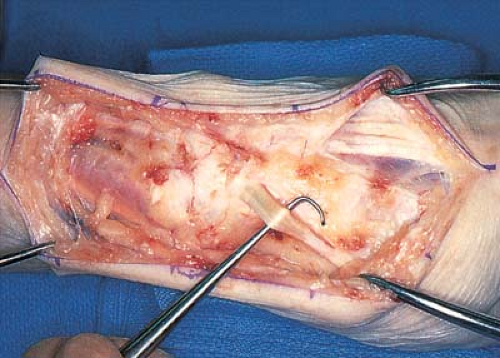
Figure 27-5 The extensor pollicis longus is identified as it exits from the third dorsal compartment.
Leave the ulnar carpus undisturbed to preserve supple motion of the ulnar hand. When preoperative radiographic and clinical examinations have shown symptomatic arthritic involvement of other joints, include these as well (Figs. 27-7 and 27-8).
Obtain exposure of the base of the index and long finger carpometacarpal joints, which is done most expediently by removing the dorsal surface of the capitate and trapezoid with an osteotome.
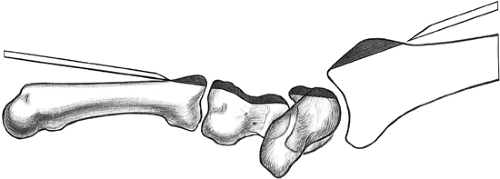
Figure 27-9 Osteotomy of Lister’s tubercle and distal radial metaphysis—osteotomy of dorsal aspect of third carpometacarpal joint along with dorsal aspect of scaphoid, lunate, and capitate.
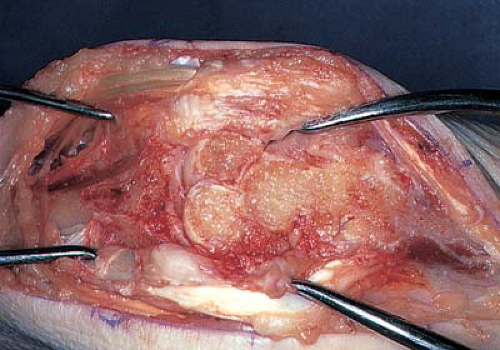
Figure 27-10 The dorsal aspects of the scaphoid, lunate, and capitate have been decorticated down to cancellous bone.
Remove the dorsal surfaces of the scaphoid and lunate down to cancellous bone by serially shaving each with an osteotome (Figs. 27-9 and 27-10) and removing up to 60% of the anteroposterior diameter. Some of these dorsal shavings can be used as additional cancellous bone graft.
Decorticate all remaining joint surfaces, including the articular surface of the distal radius, with osteotomes, rongeurs, or curettes. (I have found use of osteotomes to be the quickest method of decortication.)
Cut a transverse slot in the bases of the index and long finger metacarpals to receive a bone graft.
Take care to leave the palmar aspects of the carpometacarpal joints intact to prevent the creation of rotational deformity after plate fixation.
Technique Using Iliac Crest Bone Graft
Iliac crest bone graft can be used as an alternative to a dorsal sliding radial bone graft. Using an iliac crest bone graft somewhat increases the morbidity of the procedure. My practice has always been to harvest bone graft from the inner aspect of the iliac crest in the form of a corticocancellous slab when using iliac crest bone graft for this procedure. Using a gelatin sponge can be helpful to reduce the likelihood of postoperative hematoma formation. In recent years, I have not used iliac crest bone graft because patient discharge usually is delayed by at least 1 day because of postoperative discomfort and impaired ambulatory ability. Patients who undergo wrist arthrodesis using a sliding distal radial bone graft can be discharged home on the day of surgery. Patel et al. (9) reported minimal complications and a regrafting rate of 2.3% following the use of distal radius bone graft in 1,670 cases for various indications.
Specially designed implants are useful when performing wrist arthrodesis (10). A titanium, low-contact, dynamic compression plate has been designed and produced by Synthes (Paoli, Pennsylvania) specifically for this operation (Fig. 27-11).
To avoid prominence, taper the edges of the implant and recess the screw heads. Three versions are available. One version with a precontoured short carpal bend is chosen for a small carpus or when arthrodesis follows a failed proximal row carpectomy. A second version with a longer carpal bend is used in larger individuals. Choose a straight version is chosen when a corticocancellous intercalary bone graft is needed. These plates expedite the procedure by eliminating the need for precontouring and providing an automatic 10 degrees of dorsiflexion (Fig. 27-12). Each plate uses three 2.7-mm screws in the metacarpal, one 2.7-mm screw in the capitate, and four 3.5-mm screws in the radius. These plates usually are used in conjunction with an iliac crest bone graft.
Alternative Techniques
Minami et al. (11) reported on the use of bowed, crossed Kirschner wires (K-wires) in combination with autogenous iliac crest bone graft when performing wrist arthrodesis. Sodi et al. (12) reported
on the use of a plate for wrist arthrodesis for children and adolescents in five patients with either spinal cord injury or spasticity. Solem et al. (13) reported better results with plate fixation in extension in comparison to pin fixation in 40 wrists.
on the use of a plate for wrist arthrodesis for children and adolescents in five patients with either spinal cord injury or spasticity. Solem et al. (13) reported better results with plate fixation in extension in comparison to pin fixation in 40 wrists.
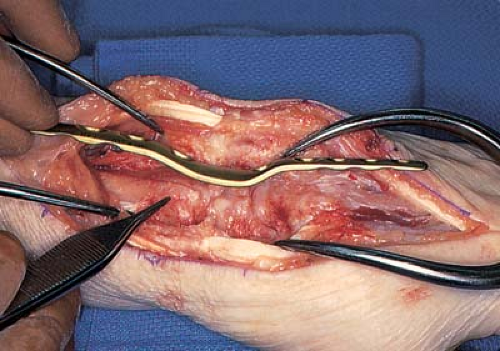 Figure 27-11 The lateral profile of a wrist arthrodesis plate takes into consideration the resulting profile after removal of Lister’s tubercle and hump. |
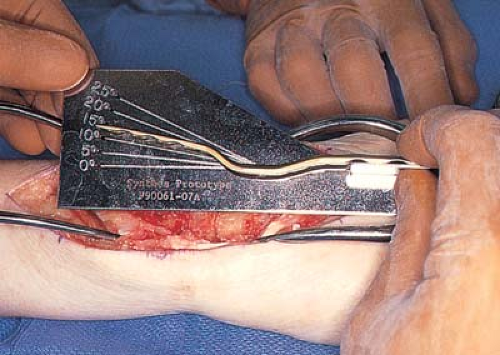 Figure 27-12 Contour the plate for arthrodesis into 10 degrees of dorsiflexion. This custom plate automatically builds in 10 degrees of dorsiflexion. |
Anderson and Thomas (14) reported successful wrist arthrodesis in 15 patients with flail or partially flail wrist using plate fixation without a bone graft. Sivakumar and Belcher (15) reported on the use of the triquetrum as bone graft in performing wrist arthrodesis. Hartigan et al. (16) report performing wrist arthrodesis in combination with proximal row carpectomy. They report using the resected carpal bones to provide local bone graft in combination with plate fixation in 17 patients. Voutilainen et al. (17




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree